Basic ECG Interpretation - Caroline Wesonga RN BSN CRRN
advertisement
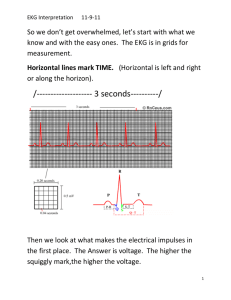
RUNNING: EKG INTERPRETATION 1 Simulation Lab: Lesson Module 2 Activity Presented to Dr. Eva Stephens THE UNIVERSITY OF TEXAS MEDICAL BRANCH at GALVESTON In Partial Fulfillment Of the Requirements for the Course GNRS 5320: Teaching Practicum By Caroline Wesonga RN BSN November 13th 2014 EKG INTERPRETATION 2 Basic ECG/Telemetry The Electrocardiogram The tracing recorded from the electrical activity of the heart forms a series of waves and complexes that have beet arbitrarily labeled PQRST and U waves To identify ECG Rhythms, you must know what each wave means, and how it should appear normally. P Wave- generated by the SA node; represent electrical depolarization of atrium PRI interval-should be 0.12-0.20 QRS complex- The QRS makes the complex and should be 0.8-0.12 T Wave - Looks a lot like a P Wave, but comes after the QRS and represent depolarization of the ventricles U Waves - does not always occur; likely represent depolarization of the Purkinje fibers. EKG INTERPRETATION 3 ECG paper is a grid where time is measured along the horizontal axis each small square is 1 mm in length and represent 0.4 seconds each larger square is 5 mm in length and represent 0.2 seconds so 5 large squares represent 1 second Basic EKG Interpretation There are essentially 5 steps for EKG Interpretation 1. Rate (Calculate the Heart Rate) The quickest and easiest method to calculate heart rate from an ECG is to count the number of R-R wave and multiply by 10. If the heart rate is fast>100bpm it is called tachycardia if the rate is slow <60bpm it is called bradycardia 2. Rhythm (measure the regularity or rhythm of the R-wave Basically do the R wave occur in a regular even pattern? or they are irregular 3. P Wave (Examine the P wave) Does it look normal? is there a P wave before each QRS complex? Are there extra P waves with no partner QRS? or do you even see any P wave at all? 4. PRI interval- Measure the P-R interval. Is it within 0.12-0.20 seconds long? 5. QRS-Measure the duration of the QRS complex. Is it 0.08-0.12 seconds long? EKG INTERPRETATION Two Methods of Counting Heart Rate Six Second Method Ventricular Rate Count the number of complete QRS within a period of 6 seconds Multiply that number by 10 to determine the number of QRS complexes in a minute Best Used for Irregular Rhythms Small Box Method Count the number of small boxes between two consecutive waveforms (R-R Interval or P-P interval) and divide by 1500 4 EKG INTERPRETATION 5 Basic Rhythms to know Normal Sinus Rhythm 1. Rate 2. Rhythm 3. P Wave: Normal in appearance, regular, One P Wave for every QRS complex 4. PRI interval-0.12-0.20 seconds 5. QRS-0.8-0.12 seconds You must know what is normal to know what is abnormal! Sinus Bradycardia 1. Rate-Below 60bpm 2. Rhythm- Regular 3. P Wave - Normal in appearance, regular, P Wave for every QRS Complex 4. PRI Interval-0.12-0.20 seconds 5. QRS- 0.08-0.12 EKG INTERPRETATION Clinical Significance: This rhythm is often seen as a normal variation in athletes, during sleep or in response to a vagal maneuver or many medications especially beta blockers Treatment Treat the underlying cause, atropine, isuprel or artficial pacing if patient is hemodynamically compromised Sinus Tachycardia 1. Rate-100-150bpm 2. Rhythm-Regular 3. P Wave- normal in appearance, regular, one P wave for every QRS Complex 4. PRI-0.12-0.20 5. QRS-0.08-0.12 seconds Underlying causes CHF hypoxia PE Increased temperature stress response to pain Treatment Identification of the underlying cause and correction if the heart rate is >150bpm it is considered SVT (Supraventricular Tachycardia) 6 EKG INTERPRETATION 7 ATRIAL RHYTHMS Atrial Tachycardia 1. Rate - 100-150 2. Rhythm-Regular 3. P Wave- May encourch on T Wave 4. PRI interval -Diffciult to measure due to the speed of the rhythm 5. QRS-up to 0.12 Causes Anxiety excitement exertion pain drugs that increase sympathetic tone (epinephrine, dopamine, cocaine) drugs that block the vagal tone (atropine) fever PE Hyperthyroidism intravascular volume loss Clinical significance When the ventricular filling time is limited, cardiac output is decreased, decreased perfusion to other vital organs occur resulting in confusion, dizziness, lightheadedness, SOB, syncope, heart failure and MI. Treatment consult attending is symptomatic. Treatment is based on recognition of the underlying cause. Adenosine is often used EKG INTERPRETATION Supraventricular Tachycardia 1. Rate- 150-250 2. Rhythm-Regular 3. P Wave- May merge with T. Difficult to see due to the rate 4. PRI - Difficult to measure 5. QRS- upto 0.12 Causes Caffeine, tobacco, alcohol, emotional stress, heart failure. Hemodynamic effects- may decrease cardiac output Treatment Treat rate by doing vagal stimulation, adenosine, cardio version, sedation, oxygen Atrial Flutter 1. Rate-250-300bpm 2. Rhythm-regular but can be irregular 3. P Wave- No definable P Waves present. Usually saw tooth pattern is present 4. PRI interval- unable to determine 5. QRS- 0.8-0.12 seconds 8 EKG INTERPRETATION 9 Clinical significance With rapid ventricular response are the same as Atrial Tachycardia. The Atria do no contract and empty as they normally do causing as loss of the atrial kick and a reduction of as much as 25% of the cardiac output Causes It occurs in diseased hearts eg valvular (esp. Mitral) disease. CHF cardiomyopathy Acute MI COPD PE After cardiac surgery Treatment Depend on the clinical condition Beta blockers, Calcium Channel blocker, digitalis DC cardio version Control rate with Calcium Channel Blockers Convert Rhythm with Cardioversion, amiodarone Atrial Fibrillation 1. Rate-Atrial rate is usually slow, normal or fast aka (Afib with RVR) 2. Rhythm: Irregularly Irregular "Hallmark for this Dysrhythmia" 3. P Wave- No present, usually saw tooth EKG INTERPRETATION 4. PRI- Unable to determine 5. QRS- 0.08-0.12 Causes Associated with COPD, CHF chronic ischemic disease, valvular disease, hyperthyroidims, sleep apnea, hypertensive disease Clinical significance The Atria do not contract and empty as normal causing loss of the Atrial kick and a reduction of as much as 25% of the cardiac output. Treatment Atrial Fibrillation <48Hours Oxygen ABCD-(Amiodarone, Beta Blockers, Calcium Channel Blockers), Direct Current Cardioversion Atrial Fibrillation >48 hours Oxygen ABC- (Amiodarone, Beta Blocker, Calcium Channel Blockers) Delay cardioversion until the patient is antiocoagulated and atial thrombi excluded Premature Atrial Contractions 1. Rate- Dependents on the underlying rhthym - slow, normal or fast 2. Rhythm- Irregular because of the premature beats 10 EKG INTERPRETATION 11 3. P Wave- P wave of PAC usually has different shape than the sinus P wave because they originate from a different atrial pacemaker 4. PRI-PAC interval may be different from underlying rhythm 5. QRS- up to 0.12 seconds Clinical Significance Isolated PACs may occur in persons with apparently healthy hearts and are not significant in persons with heart disease, however, frequent PACs may indicate enhanced automaticity of the atria, or a reentry mechanism resulting from a variety of cause such as CHF or Acute MI in addition, PACs may warn of or initiate more serious supraventricular arrhythmias such as atrial tachycardia, atria flutter or atrial fibrillation Causes May be associated with emotional stress or excessive caffeine intake sympathomimetic agents (epinephrine, isuprel) hypothyroidism various types of structural heart disease and increase in frequency with age Treatment Digitalis Beta Blocker Calcium Channel Blockers VENTRICUALAR RHYTHMS Ventricular Tachycardia 1. Rate- Greater than 100bpm EKG INTERPRETATION 2. Rhythm- Usually Regular 3. P Wave- None or buried in the QRS Complex 4. PRI - Unable to measure 5. QRS- Wide, a bizzare morphology > 0.12 Ventricular Tachycardia is three or more consecutive PVCs Clinical significance Signs and symptoms vary depending of the nature and severity of cardiac disease cardiac output decreased as much as 25% or more Considered a life threatening arrhythmia Causes physiologic ishchmia hypotension hypoxia hypokalemia heart failure Treatment If pulse is present Amiodarone or lidocaine synchronized cardioversion treat underlying cause (Stable -treat with medication, if unstable cardiovert) 12 EKG INTERPRETATION If Pulse is absent Treat at V-Fib- immediate defrillation and ACLS protocols, identification of the underlying cause is also needed Ventricular Fibrillation 1. Rate- Unable to measure 2. Rhythm- Erratic, irregular, cannot measure 3. P Wave- Unable to measure 4. PRI - Unable to measure 5. QRS- Unable to measure Causes Acute myocardial Infarction Digitalis toxicity Drug overdose Electrocusion Treatment Follow ACLS Protocol CPR Epinephrine Amiodarone Magnesium 13 EKG INTERPRETATION Premature Ventricular Contractions 1. Rate- Slow, normal or fast 2. Rhythm- Underlying rhythm consistent with occasional premature ventricular beats 3. P Wave- Related to underlying rhythm, PVCs has no P-wave 4. PRI- Related to underlying rhythm 5. QRS- Related to underlying rhythm. PVC is >0.12 seconds Clinical significance of PVCs not uncommon in normal adult of all ages occurs more frequently with advancing age young adults may have PVCs because of anxiety or excessive caffeine intake common with mitral valve prolapse may be seen with virtually any type of heart diseases most common arrhythmia seen with acute MI Causes stimulants Myocardial ischemia or infarction digitalis toxicity cardiac surgery hypoxia cardiomyopathy electrolyte imbalances Treatment search for potentially reversible causes and contributors, particularly hypoxia, hypokalemia, hypomagnesaemia and certain drug stimulant drugs 14 EKG INTERPRETATION Asystole 1. Rate-None 2. Rhythm- None 3. P-Wave- May be present but no QRS to follow 4. PRI - Unable to measure 5. QRS- Unable to measure Clinical Significance Cardiac output and a palpable pulse are absent resulting in loss of consciousness seizure Apnea Death Treatment ACLS Protocols CPR Epinephrine Atropine Determine the cause of asystole consider end of life decision 15 EKG INTERPRETATION 16 HEART BLOCKS First Degree Heart Block 1. Rate- Variable 2. Rhythm- Variable 3. P Wave- Normal shape, one P Wave for each QRS 4. PRI- Widened-greater than >0.20 5. QRS- 0.08-0.12 Clinical Significance First degree AV Block produces no signs and symptoms Because it can progress to a higher-degree AV Block under certain conditions (eg excessive administration of beta blocker or calcium channel blockers and acute inferior or right ventricular MI), the patient may require observation and ECG monitoring Causes Inferior MI ischemic acute MI digitalis toxicity hyperkalemia Increased vagal tone acute rheumatic fever myocarditis Treatment Generally does not require specific treatment treat the underlying cause Atropine observe progression to a more advanced AV Block EKG INTERPRETATION 17 Second Degree AV Block Type 1 - Mobitz 1 (Wenchebach) 1. Rate- Variable 2. Rhythm- Regular 3. P Wave- Normal Morphology with regular P to P interval 4. PRI- The PRI is progressively longer until the impulse from the AV node is completely blocked resulting in an absent QRS complex (longer, longer, longer Drop is a Wenckenback block) 5. QRS- 0.08-0.12 Seconds P wave occurs at regular interval, the PR interval progressively lengthen from beat to beat until a P wave that is not followed by a QRS complex occur. Mobitz I is usually asymptomatic because the ventricular rate remains nearly normal and cardiac output is not usually affected Causes increased parasympathetic (Vagal) tone effects of medications eg (Digitalis, Beta-blockers, Calcium Channel Blockers and Hyperkalemia acute inferior MI digitalis Toxicity Treatment if ventricular rate slows and patient is symptomatic, protocol for symptomatic bradycardia is initiated Atropine, external or transvenous pacing, dopamine or epinephrine given to increase blood pressure Temporary and resolves spontaneous normal variant in athletes because of physiological increase in vagal tone EKG INTERPRETATION 18 Second Degree AV Block (Mobitz Type II) 1. Rate- Variable 2. Rhythm- Usually Regular 3. P Wave- Normal Morphology with constant P-P interval 4. PRI - The PRI interval may be normal or prolonged, but is constant until one P wave is not conducted to the ventricles 5. QRS- Normal or widened (Because this is usually associated with a bundle branch block) Clinical Significance It is more serious than type 1. Mobitz II is usually associated with an anterior wall MI. It is not associated with increased vagal tone or drug toxicity. It is less common but more severe than Mobitz I. It has the potential to progress suddenly to 3rd degree with little or no warning. Causes it can occur after an acute anterior MI not associated with increased vagal tone or drug toxicity Treatment external pacemaker while preparations are made for insertion of a temporary or transvenous pacemaker Third Degree AV Block 1. Rate- Atrial rate is usually normal, ventricular rate is usually less than 70bpm. The atrial rate is always faster than the ventricular rate 2. Rhythm- Irregular 3. P Wave- Normal Morphology with constant P to P interval, but have no identifiable relationship to the QRS complexes EKG INTERPRETATION 19 4. PRI-The PRI may be normal or prolonged 5. QRS- Normal or widened Clinical Significance If ventricular rate is within normal limits, patient may be symptomatic of minor symptoms such as weakness, fatigue, dizziness and exercise intolerance If ventricular rate is extremely slow, cardiac output is decreased and symptoms such as hypotension, dyspnea, heart failure and chest pain seen. Atrial and ventricular contractions are unrelated due to complete blocking of the atrial impulses to the ventricles. (The atria and the ventricles are not talking with one another). Can progress to asystole. Causes Digitalis toxicity acute infection MI degeneration of the conductive tissue Treatment External pacing and atropine for acute permanent pacing for chronic complete heart block EKG INTERPRETATION 20 References Beasley, B. (2003). Understanding EKGs: A Practical Approach (3rd Ed.). Prentice Hall: Upper Saddle River, NJ. Brosche, T., A. (2009). The EKG Handbook. Jones and Bartlett Publishers: Sudbury, MA