BIO 580 - Medical Microbiology - Unit 3
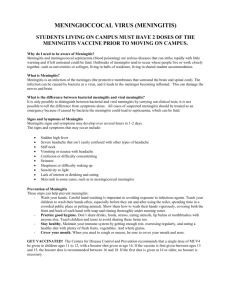
advertisement
Nervous System = peripheral nerves + central nervous system (CNS) I. Generalities: A. Structure of B. Protection of C. How do microbes get to the central nervous system (CNS)? **1. from the bloodstream - cross the Blood-Brain-Barrier (ex. bacterial meningitis, polio) *2. from the peripheral nerves (ex. herpes, VZV, rabies) 3. invasion from: bone sinuses middle ear 4. trauma II. Clinical Syndromes A. meningitis - of meninges Characterized by high fever, headache, stiff neck (classic triad) Pathology due to acute inflammation: Vascular permeability ↑WBC, ↑fluids Fluids swelling Swelling ↑pressure headache Inflammation affects muscles stiff neck Inflammation fever Causes: clogging of blood vessels (DIC) necrosis of tissue ↓ CSF flow impaired CNS function In bacterial meningitis, death occurs from shock & other serious complications within hours as a result of release of peptidoglycan + endotoxins (GN) or teichoic acid (GP) B. encephalitis - of the brain Characterized by acute febrile illness + changes in mental state, consciousness, behavior C. myelitis - of spinal cord Symptoms vary depending on where damage to cord occurs III. Infections of the Meninges A. Bacterial meningitis Acute - nearly always fatal Strong correlation of microbe with age of patient – influences the top R/O: Neonates – E. coli, Group B streptococci 1 month to 5 yrs - Haemophilus influenzae type B (Hib) 5 to 40 - Neisseria meningitidis 30 and over - Streptococcus pneumoniae Pathogenesis 1. colonization and invasion of nasopharynx 2. nasopharynx bloodstream BBB to subarachnoid 3. replicate and induce inflammation in subarachnoid space increased permeability of BBB, cerebral edema, increased intracranial pressure, decreased cerebral blood flow. Pathology Subarachnoid space purulent exudates, vein distension, focal necrosis Diagnosis CSF examination – elevated opening pressure, very ↑neutrophils, very ↑ protein, ↓glucose Prognosis Serious to grave Mortality rates Hib N. meningitides S. pneumoniae without txt = near 100% without txt = near 100% without txt = near 100% All can be present in humans in an asymptomatic carrier state with txt = 5% with txt = 7-10% with txt = 20-30% 1. Haemophilus influenzae type B (Hib) (1 month – 5) 2,895U.S./ 24 MI GNR Normal upper RT microbiota Inactivate IgA using IgA protease Colonize the nasopharynx using common pili Penetrate submucosa (invasive) bloodstream (capsule to avoid phagocytosis) Incubation - 5-6 days Symptoms develop over 1-2 days Endotoxin: 1. inflammation 2. DIC Complications – hearing loss, delayed language development, mental retardation Prevention – Vaccination 2. Neisseria meningitidis (5-40) 887 U.S./ 20 MI GNdC Person-person in respiratory droplets; 20% carriers (as high as 60-80%) Inactivate IgA using IgA protease Colonize the nasopharynx using pili sore throat Endocytized bloodstream (capsule to avoid phagocytosis) Incubation 1-3 days Symptoms develop over 6-24 hours Endotoxin: 1. affects blood vessel permeability cross BBB (attach to dura mater w/ pili) 2. drop in blood pressure shock 3. clotting of blood hemorrhage (rash = petichiae and purpura), also DIC Complications – amputations, permanent hearing loss Prevention - Vaccination 3. Streptococcus pneumoniae (30+) 4,591 U.S./ 98 MI GPC Normal upper RT microbiota sinuses or middle ear brain or pneumonia in lungs bloodstream brain Capsule Teichoic acid inflammation Prevention - Vaccination B. Viral meningitis = aseptic meningitis Most common Self-limiting, non-fatal Many different viruses: 1. Enteroviruses - 40% (primarily Coxsackievirus and Echovirus) 2. Arboviruses 3. HIV 4. HSV-2 Several considerations affect differential: Summer, fall + geographic clustering Arboviruses Late fall, winter + history of exposure to mice LCMV Late winter, early spring + male mumps virus With genital lesions HSV-2 With atypical lymphocytes EBV With chickenpox or shingles VZV Diagnosis CSF examination – ↑ lymphocytes, moderately ↑ protein, normal glucose Prognosis - In adults, excellent C. Fungal meningitis Chronic presentation – symptoms develop over days to weeks 1. Coccidioides immitis – 12,729 U.S./ 19 MI cases of coccidiodomycoses 2. Cryptococcus neoformans - AIDS IV. Infection of the Brain (Encephalon) – involvement of brain parenchyma A. Viral encephalitis Same viruses as for aseptic meningitis but relative frequency varies 1. Arboviruses (Arthropod-borne) Ex. Equine encephalitis, (West Nile virus) neuroinvasive – 361 U.S./ 0 MI Bird Mosquito Mosquito Bird Horse (human) Epidemics, geographic clustering 2. HSV-1 no insect sporadic, not epidemic 3. Enteroviruses, mumps – 982 U.S. 4.Rabies - Rhabodovirus – in animals 3,581 U.S./ 66 MI Bite Multiplies at site Travels to local nerves Peripheral nerves spinal cord brain Long incubation Prodromal phase - flulike symptoms, tingling, burning, depression Excitation phase - muscle function, speech, vision, anxiety, hydrophobia Paralytic phase - muscles weaken, consciousness fades, death Mortality - 100% with best treatment Post exposure prophylaxis (PEP) - has never failed in US B. Protozoan encephalitis 1. Primary amebic encephalitis - Naegleria fowleri Mortality = 100% 2. African Sleeping Sickness - Trypanosoma Misc. 1. Tetanus – 14 U.S. Clostridium tetani – exotoxin tetanospasmin (mimics strychnine poisoning) 2. Botulism – foodborne - 12; infant - 57; wound – 23 U.S. Clostridium botulinum Genes for toxin are carried on a bacteriophage Exotoxin botulinum prevents release of acetylcholine Produces a limp, flaccid, paralysis Eyes blurry, double vision Throat slurring speech, difficulty swallowing Difficulty breathing Cardiac problems