CNS_Infection
advertisement

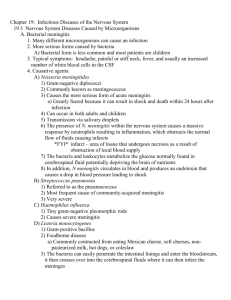
Meningitis, Encephalitis & Rabies Overview • Meningitis – The most board relevant topic • Encephalitis • A few brief words about Rabies Definitions • Meningitis is an inflammation of the membranes that cover the brain and spinal cord. • Encephalitis is an inflammation of the brain Meningitis • Typical pathogens depend on the age of the host and the presence of comorbidities • Impaired cellular immunity (HIV, steroid use, transplant, cytotoxic chemotherapy) increases risk of Listeria monocytogenes • Impaired humoral immunity (splenectomy, hypogammaglobulinemia, multiple myeloma) increase risk of S. pneumoniae • Differential diagnosis of acute meningitis includes infectious and noninfectious causes Differential Diagnosis of Infectious Causes of Acute Meningitis Viruses Nonpolio enteroviruses Arboviruses Herpesviruses (HSV, VZV, CMV, EBV and HHV-6) Lymphocytic choriomeningitis virus HIV Adenovirus Parainfluenza virus type 3 Influenza virus Measles virus Rickettsiae Rickettsia rickettsii Rickettsia conorii Rickettsia prowazekii Rickettsia typhi Orientia tsutsugamushi Ehrlichia and Anaplasma spp. Bacteria Haemophilus influenzae Neisseria meningitidis Streptococcus pneumoniae Listeria monocytogenes Escherichia coli Streptococcus agalactiae Propionibacterium acnes Staphylococcus aureus Staphylococcus epidermidis Bacteria continued Coxiella burnetii Mycoplasma pneumoniae Enterococcus spp. Klebsiella pneumoniae Pseudomonas aeruginosa Salmonella Acinetobacter Viridans streptococci Fusobacterium necrophorum Stenotrophomonas maltophilia Streptococcus pyogenes Pasteurella multocida Bacillus anthracis Capnocytophaga canimorsus Nocardia spp. Mycobacterium tuberculosis Spirochetes Treponema pallidum Borrelia burgdorferi Leptospira Protozoa and helminths Naegleria fowleri Angiostrongylus cantonensis Baylisascaris procynonis Strongyloides stercoralis Expanded from PPID 7th ed. Noninfectious Etiologies of Acute Meningitis Other infectious syndromes Parameningeal foci of infection Infective endocarditis Viral postinfectious syndromes Postvaccination (mumps, measles, polio, pertussis, rabies, vaccinia) Noninfectious etiologies and diseases of unknown etiology Intracranial tumors and cysts Craniopharyngioma Dermoid/epidermoid cyst Teratoma Systemic illness Systemic lupus erythematosus Vogt-Koyanagi-Harada syndrome Medications Antimicrobials Trimethoprim Sulfamethoxazole Ciprofloxacin Penicillin Isoniazid Metronidazole Cephalosporins Pyrazinamide NSAIDs Muromonab-CD3 (OKT3) Azathioprine Cytosine arabinoside (high dose) Carbamazepine Immune globulin Ranitidine Phenazopyridine Miscellaneous Procedure-related Postneurosurgery Spinal anesthesia Intrathecal injections Chymopapain injection Seizures Migraine or migraine-like syndromes Mollaret’s meningitis PPID 7th ed Acute Bacterial Meningitis PPID 7th edition Clinical Presentation • • • • • • • • Headache (>90%) ABM can be excluded in a patient with none of these Fever (>90%) symptoms Meningismus (>85%) Altered sensorium (>80%) Vomiting (35%) Seizures (30%) Focal neurologic findings (10-20%) Papilledema (<5%) JAMA 282 (2): 175-181, 1999 PPID 7th ed Chapter 84 Clinical Presentation • Kernig’s sign and Brudzinski’s sign both classically described but poor diagnostic sensitivity JAMA 282 (2): 175-181, 1999 Pop Quiz • Which physical exam maneuver has the highest sensitivity for meningitis? Jolt Accentuation of Headache • Asking the patient to move their head side to side at a rate of 2-3x/min • Sensitivity of 97% and Specificity of 60% • Very High negative predictive value Uchihara, T. Headache. 1991 Clinical Presentation • N. meningitidis is present in 73% of patients with ABM who have a rash (petechial) • Differential diagnosis includes RMSF, echovirus type 9, S. pneumoniae, H. influenzae, Acinetobacter and Staphylococcus aureus meningitis with sepsis Diagnosis & Treatment Who needs a head CT prior to lumbar puncture? Characteristics of Cerebrospinal Fluid Analysis in Meningitis Normal CSF Opening pressure (cm H2O) 5-20 Bloody Tap Normal WBC count (cells/mm3) <10 monocytes < 1 PMN WBC:RBC 1:700 RBC count (cells/mm3) <2 WBC:RBC 1:700 Protein (mg/dl) <45 Glucose (mg/dl) >50% serum levels Viral Meningitis Bacterial meningitis Normal to mildly elevated 10-1000 lymphocyte predominance >18 1000-5000 PMN predominance Normal Normal 15-45 Normal 100-500 Normal Normal <40 10% of ABM presents with lymphocyte predominance Up to 50% of West Nile virus patients have neutrophil predominance Modified from Bartlett JG, Pocket book of infectious disease therapy, 10th ed, Baltimore, 1999 CSF Gram staining • Sensitivity correlates with bacterial load – 25% of pts with < 103 CFUs/ml have + gs – 97% of pts with > 105 CFUs/ml have + gs • Sensitivity also correlates with pathogen – S. pneumoniae – H. flu – N. meningitidis – GNR – Listeria 90% 86% 75% 50% 30% PPID 7th ed. Ch 84 Gram positive lancet-shaped diplococci of Streptococcus pneumoniae Listeria monocytogenes Infections. Cerebrospinal fluid shows characteristic gram-positive rods (Gram stain). Listeriosis is much more common among patients with human immunodeficiency virus infection or acquired immunodeficiency syndrome compared with the general population. Neisseria meningitidis: Gram negative diplococci on CSF Gram stain CSF culture • Positive in 70-85% of patients who have not received prior antimicrobial therapy • Cultures may take up to 48 hrs for identification Steroids in Adults with Bacterial Meningitis • Routine use of dexamethasone is warranted in most adults with suspected pneumococcal meningitis • If the meningitis is found not to be caused by S. pneumoniae, dexamethasone should be discontinued • Should be given before or with first dose of abx • If the strain is highly resistant to PCN or cephalosporins “careful observation and followup are critical” MKSAP 14 Item 16 Gram Positive Diplococci MKSAP 14 Item 14 Viral Meningitis/Encephalitis Nonpolio enteroviruses Echoviruses Coxsackieviruses Enterovirus-71 Herpesviruses HSV, VZV, CMV, EBV and HHV-6 Lymphocytic choriomeningitis virus Mumps virus HIV Adenovirus Parainfluenza virus type 3 Influenza virus Measles virus Arboviruses Mosquito-borne California St. Louis Eastern equine Western equine Venezuelan equine West Nile virus Tick-borne Colorado tick fever Powassan Enteroviruses • Leading recognizable cause of aseptic meningitis • 30,000 – 75,000 U.S. meningitis cases/yr • Marked summer/fall seasonality in temperate climates • Periods of warm weather and wearing sparse clothing facilitate fecal-oral spread • PCR on CSF and supportive therapy • Newly described Enterovirus-71 can cause anterior myelitis Arboviruses • • • • • • • California (La Crosse) St. Louis Eastern Equine -- 50-70% mortality Western Equine Venezuelan Equine West Nile Colorado tick fever West Nile Neuroinvasive Disease • WNV is now the most common cause of epidemic viral encephalitis in U.S. • WNV infection – Asymptomatic 80% – West Nile Fever 20% – Neuroinvasive disease <1% • Meningitis 40% • Encephalitis 60% • Acute flaccid paralysis/poliomyelitis – 5-10% of all patients with neuroinvasive disease – 4 cases/100,000 population during a WNV epidemic Ann Neurol 2006; 60:286-300 www.cdc.gov www.cdc.gov West Nile Virus Screening of Blood Donations and Transfusion-Associated Transmission --- United States, 2003 • In 2002, transfusion-associated transmission of WNV recognized • In June 2003, nucleic acid amplification tests (NATs) for WNV applied to screen all blood donations • 6 million units screened – 818 positive viremia – 6 cases negative screen by NAT that transmitted WNV MMWR April 9, 2004 / 53(13);281-2 Distinguishing WNV, Enterovirus-71, Poliomyelitis and Guillain-Barre Syndrome Coastal marshes June, July, August Age <10, >55 yrs Unique clinical features CSF WBC >1000 Mortality 50-70% Sequelae 80% (esp children <10yrs) West, midwest Infants and adults >50 years old 5-15% mortality Sequelae: moderate in infants and low in others Mostly LaCrosse Virus Woodlands; June-September Children <20 Unique clinical feature: seizures Mortality <1% Sequelae rare <2% US, Canada, Caribbean (urban and rural) June, July, August Unique clinical feature: dysuria Mortality 2 – 20% Sequelae 25% HSV meningitis • Can be complication of primary genital infection (more common with HSV-2) – 36% of women and 13% of women with primary genital HSV-2 infection had stiff neck, headache and photophobia – Hospitalization was required in 6.4% of women and 1.6% of men for aseptic meningitis in association with primary HSV-2 infections • Meningeal symptoms start 3-12 days after onset of genital lesions • Use of antiviral therapy early for genital lesions decreases subsequent development of aseptic meningitis • Association with recurrent aseptic meningitis HSV Encephalitis • • • • • • Biphasic age distribution Temporal lobe disease Focal neurologic findings Diagnosis CSF PCR (culture) and MRI Therapy IV Acyclovir Outcome – Mortality 15% – Morbidity 50% MKSAP 14 Item 120 Diseases which mimic HSE • • • • • • • • • St. Louis encephalitis Western equine encephalitis California encephalitis Eastern equine encephalitis EBV CMV West Nile Encephalitis does not appear Echovirus to mimic Herpes Simplex Encephalitis PML SSPE HHV-6 • Infects nearly all humans by age 2 years • Exanthem subitum (roseola, Sixth dz) • Immunocompromised hosts – Reactivation in 1/3 of solid organ transplant pts and 1/2 of BMT pts by 4 weeks posttransplant – GVHD, delayed bone marrow engraftment, encephalitis, hepatitis, interstitial pneumonitis – Epiphenomen of immunocompromise? – Promotes CMV or other pathogens? – Quantitative PCR needed on CSF to invoke as etiologic agent of meningitis/encephalitis Eosinophilic Meningitis Nematodes • Angiostrongylus cantonensis • Gnathostoma spinigerum • Baylisascaris procyonis • Toxocara canis Cestodes • Taenia solium Trematodes • Paragonimus westermani • Schistosomiasis • Fascioliasis Eosinophilic Meningitis Nonparasitic • Coccidiomycosis • Cryptococcosis • Myiasis Noninfectious • Idiopathic hypereosinophilic syndrome • Leukemia/lymphoma • Cipro/Bactrim • Intraventricular gentamicin/vanc • NSAIDS • Myelography contrast Angiostrongylus cantonensis • Adults reside in pulmonary arteries of rats • Eggs hatch in the lungs, the larvae are swallowed, expelled in feces and seek an appropriate molluscan intermediate host • Develops into infective larvae in: – Slugs, land snails – Freshwater prawns, land and coconut crabs, frogs Angiostrongylus cantonensis • Epidemics and sporadic infections reported in – – – – South Pacific Southeast Asia Tawain Jamaica, Cuba, Egypt • Recognized sources of human infection – Raw or undercooked snails, prawns, crabs – Contamination of leafy vegetables by larvae deposited by slugs or snails – Caesar salad recognized in one epidemic Angiostrongylus infection • Disease self-limited • Rare fatal cases (massive inoculum) • Incubation period 1-6 days after ingestion of infected snails • HA, stiff neck, fever, rash, pruritus, abdominal pain, nausea, vomiting • Paresthesias – chest wall, face, limbs • Cranial nerve palsies (fourth and sixth most common) Angiostrongylus treatment • Supportive care • Killing larvae in and around the brain may be detrimental • Repeated lumbar punctures helpful in treating headaches • Recovery usually complete by 2 months • Corticosteroids decrease duration of headaches CID 2000; 31: 660-2 Baylisascaris procyonis • Ascarid of raccoons • Visceral larval migrans in humans • Severe and commonly fatal eosinophilic meningoencephalitis occurs in more than half the cases • Eye involvement is common • Diagnosed by detecting larvae in tissue • Experimental serology • Albendazole and steroids are commonly tried Bayliscariasis • Severity of disease – Number of eggs ingested – Extent/location of larval migration – Severity of ensuing inflammation and necrosis Treatment • Laser photocoagulation in ocular dz • No cure for clinical disease • Albendazole and dexamethasone used with good CNS and ocular penetration • Prophylaxis with albendazole on days 1-10 or days 3-10 after exposure offers 95-100% protection • No children receiving albendazole after eating raccoon feces have developed baylisascariasis CID 2004: 39 (15 November) Rabies • Highest case fatality rate of any infectious disease • Let me say it again… • 2-3 cases annually in USA • Recent death in a returned OEF soldier • Transmitted most often by bite from rabid animal • Transmission from tissue donors has also been described Source: Centers for Disease Control and Prevention, November 2010 Rabies • Virus amplifies at inoculation site and reaches CNS via motor/sensory nerves • Moves centrally at a rate of 5-10cm/day • Clinical Latency period 3-6 mos (7d-1yr) • Nonspecific prodrome – “flu like symptoms” – Paresthesia or pain at site Rabies • Encephalitic Rabies (80%) – Hydrophobia, aerophobia, pharyngeal spasms • Paralytic Rabies (20%) • Clinically similar to Guillan-Barre Syndrome • Coma, paralysis and cardio/pulmonary collapse with 2 weeks Diagnosis/Treatment • • • • • Sample of saliva, skin for PCR Antibody from serum or CSF Treatment is RIG and Vaccine after exposure 1 patient has survived (17 yo F from Wisconsin) The “Milwaukee Protocol” – Ketamine, Ribavirin, Amantadine • Has not been successful in subsequent patients Pre/Post Exposure • Prior to exposure in high risk individuals Questions/Comments?