Common Neurological Disease Dr. Abdul-Monim Batiha,
advertisement

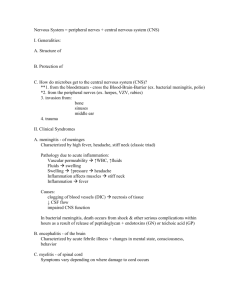
Common Neurological Disease Dr. Abdul-Monim Batiha, Status epileptics is a life-threatening condition in which the brain is in a state of persistent seizure. Definitions vary, but traditionally it is defined as one continuous unremitting seizure lasting longer than 30 minutes , or recurrent seizures without regaining consciousness between seizures for greater than 30 minutes (or shorter with medical intervention). • The symptoms may be associated with tonicclonic, complexpartial, or absence seizures • It is always considered a medical emergency. • The mortality rate of status epilepticus is very high (at least 20%), especially if treatment is not initiated quickly. • However, with optimal neurological care and a good prognosis, the patient (even some epileptics) in otherwise good health can survive with minimal or no brain damage, and can even avoid future seizures Causes • Only 25 percent of people who experience seizures or status epilepticus have epilepsy. • Stroke • Intoxicants or adverse reactions to drugs. • Insufficient dosage of a medication already prescribed to the patient. • Sudden withdrawal from a seizure medication • Consumption of alcoholic beverages while on an anticonvulsant. • Dieting or fasting while on an anticonvulsant. Causes Common causes of newonset status epilepticus are: Brain disorders, such as: ◦ ◦ ◦ ◦ ◦ Meningitis Encephalitis Brain tumors Abscess Traumatic brain injury Sepsis Some autoimmune disorders Extremely high fever, especially in children Low glucose levels Eating disorders Classification of Seizures 1. Generalized Involve both hemispheres; loss of consciousness; ■ Classification of Seizures 2. Partial Focal; involve one hemisphere Classification of Seizures Complex partial—altered level of consciousness; with or without automatisms: lip-smacking, swallowing, aimless walking, verbalizations diagnosis • • • • • History taking CT-scan MRI EEG Epilepsy Monitoring Unit Clinical management • • • • • Benzodiazepines Phenytoin Carbamazepine and valproate Barbiturates General anesthetics Nursing Management The nurse initiates ongoing assessment and monitoring of respiratory and cardiac function because of the risk for delayed depression of respiration and blood pressure secondary to administration of antiseizure medications and sedatives to halt the seizures. Nursing assessment also includes monitoring and documenting the seizure activity and the patient’s responsiveness. The patient is turned to a side-lying position if possible to assist in draining pharyngeal secretions. Suction equipment must be available because of the risk for aspiration. The intravenous line is closely monitored because it may become dislodged during seizures. A person who has received long-term antiseizure therapy has a significant risk for fractures resulting from bone disease (osteoporosis, osteomalacia, and hyperparathyroidism), a side effect of therapy. Thus, during seizures, the patient should be protected from injury using seizure precautions and monitored closely. No effort should be made to restrain movements. The patient having seizures can unintentionally injure nearby people, so nurses should protect themselves. PATIENT EDUCATION AND DISCHARGE PLANNING ■ Make the home environment safe, particularly in the case of tonic-clonic epilepsy. ■ Assess for injury after each seizure. ■ Keep a log to record a description of the seizure and postictal period, duration, time of day, severity, and any new characteristics. • Wear a Medic Alert bracelet. • ■ Monitor serum antiepileptic drug levels when appropriate. • ■ Be aware of circumstances when emergency treatment Encephalitis Encephalitis is an acute inflammation of the brain. A common cause of viral encephalitis in humans is herpes (HSE). It can be caused by a bacterial infection such as bacterial meningitis spreading directly to the brain (primary encephalitis), or may be a complication of a current infectious disease syphilis (secondary encephalitis) Symptoms Patients with encephalitis suffer from fever, headache and photophobia with weakness and seizures also common. Less commonly, stiffness of the neck can occur with rare cases of patients also suffering from stiffness of the limbs, slowness in movement and clumsiness depending on which specific part of the brain is involved. Neck rigidity may lead to a misdiagnosis of meningitis, but treatment is the same. Other symptoms can include drowsiness and coughing. Diagnosis Examination of the cerebrospinal fluid obtained by a lumbar puncture procedure usually reveals increased amounts of protein and white blood cells with normal glucose, (though in a significant percentage of patients, the cerebrospinal fluid may be normal). CT scan often is not helpful, as cerebral abscess is uncommon. Cerebral abscess is more common in patients with meningitis than encephalitis. Bleeding is also uncommon except in patients with herpes simplex type 1 encephalitis. Magnetic resonance imaging offers better resolution. EEG Treatment Treatment is usually symptomatic. Antiviral or antibiotic In patients who are very sick, supportive treatment, such as mechanical ventilation, is equally important. Corticosteroids (e.g. methylprednisolone) are used to reduce brain swelling and inflammation. Sedatives may be needed for irritability or restlessness. Anticonvulsants are used to prevent seizures. Meningitis Meningitis is inflammation of the protective membranes covering the brain and spinal cord, known collectively as the meninges. The inflammation may be caused by infection with viruses, bacteria, or other microorganisms, and less commonly by certain drugs. Meningitis can be life-threatening because of the inflammation's proximity to the brain and spinal cord; therefore the condition is classified as a medical emergency. Signs and Symptoms The most common symptoms of meningitis are headache and neck stiffness associated with fever, confusion or altered consciousness, vomiting, and an inability to tolerate light (photophobia) or loud noises (phonophobia). Sometimes, especially in small children, only nonspecific symptoms may be present, such as irritability and drowsiness. If a rash is present, it may indicate a particular cause of meningitis; for instance, meningitis caused by meningococcal bacteria may be accompanied by a characteristic rash Diagnosis • lumbar puncture may be used to diagnose or exclude meningitis. • This involves inserting a needle into the spinal canal to extract a sample ofcerebrospinal fluid (CSF), the fluid that envelops the brain and spinal cord. • The CSF is then examined in a medical laboratory. Treatment • The usual treatment for meningitis is the prompt application of antibiotics and sometimes antiviral drugs. • In some situations, corticosteroid drugs can also be used to prevent complications from overactive inflammation. Complications and Prevention • Meningitis can lead to serious long-term consequences such as deafness, epilepsy, hydrocephalus and cognitive deficits, especially if not treated quickly. • Some forms of meningitis (such as those associated with meningococci, Haemophilus influenzaetype B, pneumococci or mumps virus infections) may be prevented by immunization