Open Enrollment - Wake Employees
advertisement
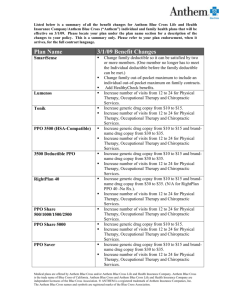
2015 Annual Enrollment: Questions and Answers Inside this Q&A, you’ll find answers to general questions you might have about the changes to our benefits for 2015. For answers to specific questions, attend one of the two informational meetings during Open Enrollment. Open Enrollment Q. When will Open Enrollment take place? A. Open enrollment for 2015 will take place from Monday, October 20 to Friday, October 31. Remember to mark these dates on your calendar and keep the October 31 deadline in mind! Q. If I like my plans I have right now, do I need to do anything during Open Enrollment? A. Yes! This year, we are making several changes to your health benefits for 2015. Due to the changes, we are requiring that you must make an election for the health plan to continue to be enrolled in coverage. *Take time to review your benefits and make sure you enroll. If you DO NOT make an election and DO NOT enroll in either the PPO75 or PPO85 plans, you and your family WILL NOT have health coverage as of January 1, 2015. Changes to Your 2015 Benefits Q. Are my health benefits changing next year? A. Yes. Wake County is making changes including several enhancements to your benefits coverage for next year. These changes will become effective January 1, 2015. Q. Why are my benefits changing? A. Before recommending changes for next year’s benefits, we carefully reviewed our current plan design. The changes made are based on analysis of claims data and the County’s philosophy of wellness with respect to charges for health care. The changes are based on: 1) Cost shift (strategically and targeted) to drive desired behaviors and that those who use the benefit more pay more through the plan design instead of raising premiums across the board for everyone and 2) encourage health and wellness behaviors that positively impact overall health and thereby control claims utilization. Health Plan Q. What changes are being made to the Health Plan? A. Blue Cross Blue Shield will continue to administer the PPO75 and PPO85 plans. The following changes are being made: Employee and retiree health insurance premiums will remain constant for the third year in a row, for both the PPO75 and PPO85 plans. Copays for office visits and coinsurance will remain the same as well. Affordable Care Act (“ACA”) new requirement: Currently, only your medical deductibles, copays and coinsurance amounts apply toward the out-of-pocket maximum. Once you reach your out-of-pocket maximum, the County pays 100% of your services for the rest of the year. The ACA now requires that payments for pharmacy must now apply to the out-of-pocket maximum as well. To address this change, out-of-pocket maximums under the Medical Plan will be increased to a level that maintains the same relative benefit while taking into accounts the amounts paid for pharmacy that had not previously applied to the out-ofpocket maximum. There will be an increase in the emergency room copay (from $100 to $300) to encourage urgent care for situations that could be handled outside of the emergency room. Copay is waived if admitted. We have established a hospital inpatient admission copay of $200. Bariatric surgery is being added to both the PPO75 and 85 Plans and will be covered at Blue Cross Blue Shield Blue Distinction Centers only. ER Copay Individual Deductible Out-of-pocket Maximum Inpatient Bariatric HEALTH COVERAGE PLAN DESIGN CHANGES PPO 75 PPO 75 PPO 85 PPO 85 Change Current Change Current $100 $300 $100 $300 $1250 /$2500 +$250 /+$500 $750/$1500 No Change $3500 / $7000 + $900 / $1800 $2500 / $5000 + $1200 / $2400 None N/A $200 Copay None $200 Copay Covered at N/A Covered at Blue Blue Distinction Distinction Center Center Only Only No changes to: Office (primary or specialty) or urgent co-pays and coinsurance. Q. Will I get a new member ID card? A. If you enroll in the PPO75 or PPO85 plans, you and other eligible participants will get a new member ID card from BCBSNC. Cards will be mailed to your homes before January 1, 2015. Prescription Drug Plan Q. What changes are being made to the Prescription Drug Plan? A. OptumRx will continue to administer the Prescription Drug Plan. The new changes are: The maximum cost for generic drugs is being reduced from $100 to $50. Important Reminder: Between now and the end of the year, you may want to ask your doctor to switch your prescriptions to generics to save money for you and your family. The maximum cost for non-preferred drugs will increase for both 30-day retail and 90-day supply (as shown in the following chart). Pre-authorization will now be required for compounded drugs. Note: Compounding is the combination of different ingredients of a drug to create a medication tailored to the needs of an individual patient. Generic Preferred Brand Non-Preferred Brand Compounding PRESCRIPTION DRUG PLAN DESIGN CHANGES Retail (30 day) Retail (30 day) 90-Day Supply 90-Day Supply (2014) Current (2015) Change (2014) Current (2015) Change 20% up to 20% up to $50 20% up to 20% up to $125 $100 maximum maximum $250 maximum maximum 35% up to No change 35% up to No change $100 maximum $250 maximum 50% up to 50% up to $150 50% up to 50% up to $300 $100 maximum maximum $250 maximum maximum None Preauthorization None required for $150 maximum or more* *Bulk chemical products are excluded for compounded drugs Preauthorization required for $150 maximum or more*