Humber Community Pain Service Referral Form.doc
advertisement

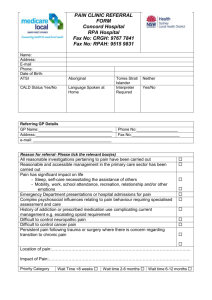
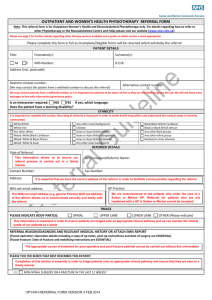
Humber Community Pain Service Referral Form NHS no.: ……………………………….............. Date of birth: ……………………...................... Surname: ……………………………………….. Hospital no.: ……………………………………. Forename: ……………………………………… Patient’s telephone no: ……………………….. Address: ………………………………………… Patient’s mobile no: ......................................... ……………………………………………………. Patient consent to text message: Yes/No ……………………………………………………. Postcode: ……………… Date of referral: .............................................. Referring GP/ health professional: ………………………………………… Practice stamp/address: Registered GP: ………………………………………… GP’s Telephone no.: ………………………………………… GP’s Fax no.: ………………………………………… Signature of Referrer: ……………………………. Is the patient willing to engage in a pain management, as opposed to pain relief, approach? Yes/No Has the patient agreed to be referred to the community pain team? Yes/No Full history of persistent pain problem and reason for referral Have all investigations regarding the persistent pain problem been completed? Yes/No MSK Pain? Has the patient had assessment (and treatment if necessary) via level one physiotherapy? If No, please do not consider referral until these have been completed. Yes/No Please list or include a printout with information on all relevant investigations & treatments e.g. blood test results, x-rays, scans, treatment discharge summaries etc. Past medical history (please list or include printout) All present medications and allergies (please list or include printout) Has the patient been seen by any other speciality or clinic for persistent pain problems? (if so please give full details) NB referrals not accepted if still receiving care from another pain management service Psychiatric/psychological problems (including current counselling/psychiatric support if any) Has the patient been prescribed red drugs e.g. Ketamine? Red Flag Checklist 1. Is the pain as a result of injury or trauma? 2. Do they have a history of cancer? 3. Do they have a fever, a sensation of being cold, wake up sweating, or have temperature changes during the night which could indicate a joint infection? 4. Have they ever had a transplant of any kind or experienced intravenous drug use or prolonged steroid use? 5. Have they experienced any unexplained weight loss (10lbs + in 3 months) not directly related to a change in activity or diet? 6. Recent bacterial infection (e.g.) urinary tract infection for more than 3 months? 7. Are they experiencing altered sensation/numbness around their genitals/back passage? 8. Do they experience any bladder or bowel problems/irregularities, such as urinary retention, changes in frequency of urination or incontinence? 9. Are they experiencing progressive or severe weakness in their legs? 10. Do they experience, for no reason any tripping or catching of their feet when walking? 11. Do they have a “band like” pain radiating into their chest or abdomen? 12. Is the pain worse when they lie down? 13. Does the pain keep them awake at night, unrelated to movement or positioning? 14. Does the patient have widespread neurological symptoms? Yes/No Yes/No Yes/No Yes/No Yes/No Yes/No Yes/No Yes/No Yes/No Yes/No Yes/No Yes/No Yes/No Yes/No Yes/No If you answered “yes to any of the red flag questions, please provide more information Please return this form with all supporting information to: Humber Community Pain Service, c/o The Physiotherapy Department, East Riding Community Hospital, Swinemoor Lane, Beverley HU17 0FA Tel. 01482 478886/0800 731 4483 Fax. 01482 478887