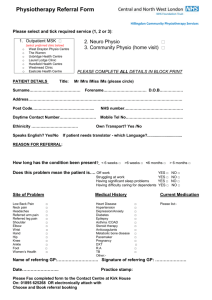
National MSK GP decision making tool
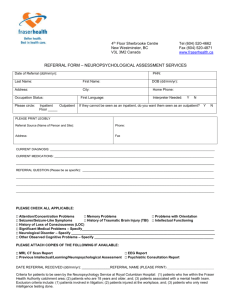
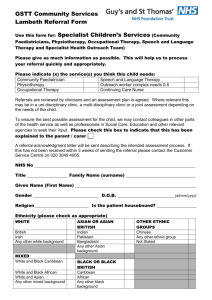
advertisement
Musculoskeletal Decision Making Tool This tool is currently in development and work is underway to refine and enhance flow and ease user interaction Musculoskeletal Decision Making Tool MSK Pathway General GP Information about Allied Health Professionals General Injection Advice Patient Information Leaflets Contact us Useful websites Click over affected area for guidelines / advice / referral guidance Alternatively click on body area below Cervical spine Thoracic Spine Shoulder Elbow Wrist and Hand Lumbar Spine Hip Knee Foot and ankle Please note these MSK orthopaedics / AHP guidelines have been produced as an aide memoire only and are not a substitute for GP / AHP knowledge about their individual patients. NB. Referral Guidelines for Rheumatology remain unchanged Key MSK PATHWAY – DRAFT National MSK programme (Blue) NHS Tayside programme (Yellow) PATHWAY ONE Self Management and Advice Simple MSK Problem * NHS 24 PATHWAY TWO 10% - 20% Referrals PATIENT GP Red Flags Severe Pain, Significantly Decreased Function OR Clear Secondary Care Referral (refer to MSK guidelines) Secondary Care Referral PATHWAY THREE 80% - 90% Referrals MSK Service AHP led MSK service (Possibly with GPwSI) Triage Diagnostics Treatment 90% 10% Referrals Orthopaedic Rheumatology Plastics Pain Clinic Neurosurgery Referrals DISCHARGE Return to home page General GP Information What can a Physiotherapist offer? How to Refer to Physiotherapy What can an Occupational Therapist offer? What can an Orthotist Offer? What can a Podiatrist offer? Musculoskeletal Pathway Physiotherapy Triage Information Onward referrals Physiotherapy Appointments Ortho post op timescales OHSAS Working Health Services Useful Websites Community Rehabilitation Team (CRT) Patients with Long Term MSK Problems Return to home page What can an Physiotherapist offer ? N.B if red flags are identified please refer to secondary carenot AHP service. • Help with any musculoskeletal condition • Diagnosis and treatment. – Simple advice (sometimes the best treatment) – A course of treatment. • Imaging requests if appropriate • Steroid injection if appropriate • Referral on to another Health Care Professional N.B. There is a high tendency for a significant number of MSK conditions to spontaneously resolve • The success of a patient’s therapy will depend on them following the treatment plan and advice given by the therapist. It would be helpful if you could ensure that the patient understands this. • Please refer to the MSK referral criteria guidelines for further information Return to General GP Information Return to home page AHP Musculoskeletal Pathway GP REFERRAL Referral received into Physiotherapy Service Click for dept details Dundee Perth & Kinross Angus Triaged By Senior Physio to mainstream or specialist therapists URGENT (SOON) Seen within 10 working days Assessment, Treatment/ Self Management Reassessment No improvement in 4 treatments ROUTINE – as per waiting times 2nd Opinion within physio service/ AHP Service (Pod, GPwSI, OT etc) Discharge/ Onward referral Self Referral Diagnostics Return to General GP Information Return to home page How to Refer to Physiotherapy • Please encourage your patient to self refer as per local agreement • Please also give out the information leaflet on self help • Patient information leaflets are available for a variety of conditions • If you would like to give us more information please use SCI gateway (RMS) • Would you like Email advice from a senior physiotherapist? Tay-uhb.mskphysio@nhs.net Return General GP Information Return to home page Physiotherapy Triage Information and Urgent criteria (1) • • • • • • • • • • • • • • • • When a patient is referred or self refers to any MSK Physiotherapy Service the referral is triaged by Senior staff. Any referral that is highlighted as being urgent by a GP will be treated as such by the physiotherapy staff. Only after discussion with the referring clinician will any change be made to the urgency of a referral. Urgency and whether the patient will be seen by mainstream or specialist physiotherapist will be determined by the information given on the referral form. Triage categories have been agreed in order that those patients who would benefit from earlier intervention are offered timely assessment and treatment. For patients referred with Orthopaedic conditions the triage categories have been agreed in partnership with local Orthopaedic Consultants and the timescales for appointments follow National Orthopaedic pathways. AHPs have the option to triage a referral as: Urgent – to be seen within 10 working days. Routine – to be seen as per local departmental waiting times. Or as per Orthopaedic post op timescales. SPINAL symptoms below will be triaged as urgent Lumbar: Below knee pain/worsening symptoms/>6 week duration Progressive neurological deficit. Patient acutely distressed or leg pain worse than back pain Bilateral below knee pain +/- altered sensation as indicated on body chart. Cervical: All as per Lumbar (below elbow pain/symptoms) If information available on referral: 1 out of 3 1.Sensory Loss* 2. Motor Weakness* 3. Reflex changes* » * In combination, in the lower limb, with a positive SLR. Immediate telephone triage (to be documented on patient referral) for all new self referrals which identify: New onset bladder or bowel dysfunction. Combination of previous cancer/unexplained weight loss/worsening symptoms. Saddle anaesthesia. Return to General GP Information Return to home page Forward to more urgent criteria Physiotherapy Triage Information Urgent Criteria (2) • • • • • • Antenatal back/pelvic pain • (Consider estimated due date.) Newly diagnosed CRPS Bells Palsy: (Consider duration since onset & medical management. Most current sources suggest spontaneous resolution for most cases. Prednisilone • within 72 hours treatment of choice (NHS Choices; http://cks.nice.org.uk/) POP removal ORIF Removal of metalwork at fracture site • Consider site of fracture (possible impact on function) & local or general anaesthetic procedure used. Acute soft tissue injuries < 6 weeks only to be categorised as urgent/soon priority in circumstances of: – – – Worsening symptoms. Significant impact on function/mobility/weight bearing e.g. Gastrocnemius tears. Significant trauma e.g. Whiplash injury if aforementioned spinal signs present. NB The service cannot offer urgent priority appointments for all acute soft tissue injuries. These should be directed toward self management strategies and prioritised as routine. Recently/currently off work & inability to care for dependants. Not to be used in isolation for priority appointment but may be considered in combination with other factors. Return to General GP Information Return to home page Forward to Ortho Post Op Timeframes Ortho Post Op Treatment Timeframes Will be seen in physio at timescales indicated Shoulder Knee Replacement for # 3 weeks TKR 2 weeks Bankhart repair 6 weeks ACL Reconstruction 10 Days Slap repair 3 weeks Arthroscopy 2 weeks Weaver dunn 6 weeks Dislocation 10 days Rot cuff repair - minor (Arthroscopic) 4 weeks (2 weeks) Hip Rot cuff repair - major (Arthroscopic) patch repair 6 weeks (4 weeks) 8 weeks Bilateral THR/BHR 2 weeks Decompression - Arthroscopic 2 weeks Arthroscopy (depends on op) 10 days – 6 weeks Decompression - open 3 weeks MUA ASAP Fractures- general Ankle Replacement 6 weeks Post op TA repair 2 weeks post ref Elbow 10 days Spine Wrist – CRPS ASAP Microdiscectomy 6 weeks # Femur – IM nail 10 days Laminectomy 6 weeks # Tibia – IM nail 3 weeks For an Orthopaedic condition/#/procedure not indicated on above list resulting in uncertainty as to treatment timescale please contact the Physiotherapy Department Return to General GP Information Return to home page AHP Appointments • • • All AHP appointments are arranged in line with NHS Scotland Access Policy. Patient focused booking allows patients to make an appointment at a suitable time. This system has shown reduced DNA rate. We aim to have all referrals triaged within one working day of receipt. URGENT - 10 working days • Patient will be contacted by phone or letter posted within 48 hours. Please include day time contact number on any SCI gateway referrals ROUTINE - as per department waiting time • Patients who are categorised as routine will be sent a letter inviting them to phone in to arrange a suitable appointment time. An appointment will normally be offered within 4 weeks of receiving the letter. When the letter is sent will vary and is dependant on the waiting time within department the patient is to be appointed to. • Patients are informed, on the invitation letter, that if they do not respond within two weeks we will assume they do not wish to make an appointment and they will be discharged from the service. Return to General GP Information Return to home page Onward Referrals Onward referral • Following assessment and treatment, patients will either be discharged from therapy or referred onward to another department. You will be copied into any onward referral letter. • Routine discharge letters will be sent as per local agreement • If there has been an intervention, which has not resulted in a successful outcome, or the AHP needs to convey any information to the GP this will be done by letter. • AHPs may occasionally require to contact a GP by telephone to discuss a patient’s care. Return to General GP Information Return to home page Community Rehabilitation Team The Community Rehab Team provides treatment for patients over 16 that require rehabilitation in their own environment to promote independence and optimise function in particular activities of daily living. The team provides Physiotherapy, Occupational Therapy and is supported by AHP support workers. • • Reduce falls risk through Multi-factorial assessment (Tinetti 2003; Chang et al 2004) Addressing some of the modifiable risk factors identified by SIGN (muscle weakness; abnormality of gait/balance; foot problems; layout of home environment) • Improve physical function, strength, balance and cardiovascular fitness Using progressive exercises (Binder et al 2002; Campbell et al 1997); and gait/function re-education • • • • • Urgent Acute exacerbation of chest conditions (aim to see patient in two working days) Sudden deterioration in physical function Recurrent falls in last 3 months impacting on ability to remain at home Fall related injuries Recent hospital admission/illness now impacting on function and independence • • • Routine Able to meet specific rehabilitation goals following a new problem and have consented to CRT assessment following explanation. Problems and goals amenable to Physiotherapy. Patient/carer advice for chronic conditions that require re-assessment Return to General GP Information Return to home page Local AHP Outpatient Depts. Return to NHS General GP Information Return to home page Working Health Services • Is your patient self employed or do they work for a small business employing less than 250 people? • The Scottish Government has funded Working Health Services to allow people who work in small businesses to access a range of specialist health services. • Please encourage your patient to self-refer by telephoning 01382 825100 for an appointment Return to General GP Information Return to home page What can a Podiatrist Offer? • Podiatrists are autonomous healthcare professionals who deal with the prevention, diagnosis, treatment and rehabilitation of medical and surgical conditions of the feet and lower limbs. We aim to improve the mobility, independence and quality of life for their patients This can include providing the following: • essential foot care • vascular and neurological assessment • ongoing monitoring of foot health, in particular of those with circulation problems and diabetes • wound management for a patient with diabetic ulcer • nail surgery using a local anaesthetic • biomechanical assessment leading to the prescription and manufacture of foot orthoses Return to General GP Information Return to home page What can an Orthotist Offer? • Assessment and provision of a range of splints, braces and special footwear to aid movement, correct deformity and relieve discomfort. Return to General GP Information Return to home page What can an Occupational Therapist Offer? • Work with people of all ages and backgrounds who are affected by accident, physical and mental illness, disability or ageing • Provide help and training in daily activities, such as bathing, dressing, eating, gardening, working and learning • Offer advice on adapting the home or workplace to meet the patients’ needs • Assess and recommend equipment, such as mobility aids, wheelchairs and artificial limbs and, if needed, advise on special devices to help around the home, school or workplace • Work with organisations to improve employees' performance Return to General GP Information Return to home page Useful Websites • www.nhs24.com • www.nhsinform.co.uk/msk • www.chronicpainscotland.org Return to General GP Information Return to home page Patients with Long Term MSK problems Re-referrals of patients with Long Term MSK problems SIGN GUIDELINES CHRONIC PAIN • Patients who have previously attended physiotherapy, without benefit, are unlikely to benefit from further physiotherapy for the same problem. However, patients who understand that they have a long term problem and are happy to engage with self management techniques, could be offered a self-management advice session from the musculoskeletal physiotherapy service. • In all cases consideration should be given to selfmanagement strategies. In the case of chronic pain, referral to Pain Association Scotland or to the Pain Clinic may be appropriate, if not considered previously. Return to General GP Information Return to home page Low Back Pain Pathway Suspected Cauda Equina Signs and symptoms Referral information Other Red Flags Signs and symptoms Referral Criteria / information Nerve Root Pain / Spinal Stenosis Signs and symptoms Signs and symptoms Persistent Low Back Pain GP Advice Link to you tube lumbar spine examination Referral Criteria / information MRI Referral Flowchart Referral Criteria GP management advice Simple Low Back Pain Key Information Points Key Information/ Prescribing guidance Further options: MDT pain clinic Patient education Class Exercise referral scheme Patient information Referral options Return to home page LBP Patient Information leaflets Signs and Symptoms Suspected Cauda Equina Signs and Symptoms • Dysfunction of bladder, bowel or sexual function – sphincter weaknesses causing urinary retention and post-void residual incontinence, difficulty in initiating micturition – May be decreased anal sphincter tone with consequent faecal incontinence; • • Sensory changes in saddle or peri-anal area Gait disturbance – Weakness of the muscles of the lower extremities innervated by the compressed roots – Bilateral leg pain below the knee and weakness – Bilateral absence of ankle reflexes. • Pain may be wholly absent; the patient may complain only of lack of bladder control and of saddle anaesthesia Patient Primary Care Secondary Care Return to LBP Pathway Forward to Emergency Referral Information Return to home page Emergency Referral Information Suspected Cauda Equina • Discuss with on call team Neurosurgical Unit Malignant Spinal Cord Compression Hotline for those people with history of cancer + new lumbar spine referral + gait disturbance: 07960 512277 Signs and Symptoms • History of cancer • Band like, escalating trunk pain • Can be worse lying flat/at night • Gait disturbance/vague non specific lower limb symptoms /reduced mobility • Altered sensation in non-dermatomal pattern. Return to LBP Pathway Return to home page Patient Primary Care Secondary Care Red Flags part 1 Signs and Symptoms and Referral Criteria Primary care • Consider bloods- FBC, UE's, LFT's bone group, CRP/PV • X-rays not recommended unless thoracic osteoporotic fracture is suspected Secondary care Red Flags: NB: Index of suspicion only Discuss with Physiotherapy / Neurosurgical on call team • First acute onset age <20 or >55+ raised ESR or abnormal FBC or LFT’s • Non-mechanical pain • Thoracic pain • PMH -cancer, previous IV drug abuse, HIV, steroids, osteoporosis, TB • Unwell, weight loss >10 % body weight within 3-6 months • Widespread neurology – unilateral or bilateral lower limb weakness and/or numbness extending over several dermatomes • Pain worse at night/night sweats • Structural deformity (acquired and deteriorating, not congenital) • Trauma Patient Primary Care Secondary Care Upper Motor Neurone lesion Urgent referral to Neurosurgical department • Non-dermatomal sensory loss (stocking/glove) • Paraesthesia • Non myotomal muscle weakness • Hyperreflexia • Positive Lhermitte’s sign (neck flexion produces general electric shock) • Positive Hoffmans sign (flexion and sudden release of the terminal phalanx of the middle finger results in reflex flexion of all the digits) • Generalised hypertonicity or flaccidity • Positive Babinski Aortic Aneurysm Urgent referral to surgical team • Over 60 • Acute, sudden onset of back pain • Low back pain that is severe - doubled over in pain. • Severe abdominal pain • Continuous pain, not better with rest • Pain may radiate into the groin or leg • Pain may be accompanied by symptoms of internal bleeding, such as nausea, vomiting, rapid heart rate, cool or clammy skin, sweating, and/or shortness of breath. Forward to more red flags Return to LBP Pathway Return to home page Red Flags part 2 Signs and Symptoms and Referral Criteria Aortic Aneurysm Urgent referral to surgical team • Over 60 • Acute, sudden onset of back pain • Low back pain that is severe - doubled over in pain. • Severe abdominal pain • Continuous pain, not better with rest • Pain may radiate into the groin or leg • Pain may be accompanied by symptoms of internal bleeding, such as nausea, vomiting, rapid heart rate, cool or clammy skin, sweating, and/or shortness of breath. Discitis/infection symptoms: Discuss with Neurosurgical on call team • Sudden onset of acute spinal pain or suspicious change in pattern, no history of trauma • Systemic signs, fever, high pulse • Night pain • All spinal movements grossly restricted by pain & spasm Patient Primary Care Secondary Care Inflammatory Spondyloarthropathy: Urgent referral to Rheumatology department • Morning stiffness & backache, or multiple joint problems (pain/stiffness/swelling) • Generally unwell • Classic Ankylosing Spondylitis posture (insidious onset, ≤40, persisting at least 3/12, associated with morning stiffness, better with exercise) • Associated skin rash, inflammatory bowel disease, eye problems (uveitis/conjunctivitis), urethritis or sacroiliac pain/tenderness • Any of the above with or without the following: – Positive C-Reactive protein (CRP),ESR, Plasma viscosity (PV) – Positive HLA B27test in conjunction with XR changes and / or positive CT of SI joints or bone scan. – Raised ESR in conjunction with positive HLA B27 test Return to previous page Return to LBP Pathway Return to home page MRI Referral Flow Chart Nerve Root Pian Plain film lumbar spine XR is not indicated as it does not contribute to the management of leg pain Yes No Does pain radiate below the knee and a genuine straight leg raise (SLR) sign is present? (SLR test results in severe aggravation symptoms or LBP, not just hamstring tightness) No Does patient have motor deficit e.g. foot drop. NB absent ankle jerk is not motor deficit Yes MRI not indicated No Has the patient has symptoms for more than 4 weeks? No Your patient may have unexpected pathology and paediatric referral is indicated Yes Refer for urgent MRI and urgent surgical clinic review On MRI request form, write ‘urgent’ and the name of the consultant your patient has been referred to Yes MRI not indicated. Continue with conservative management, as symptoms may improve spontaneously Refer for routine MRI. Surgical discussion at referrer’s discretion. MRI request forms should state the side and dermatomal location of symptoms / signs so that informed correlation with imaging findings can be made. E.g. right side sciatica, L5 dermatomal pain/numbness. No motor signs ? R L5 nerve root entrapment Return to LBP Pathway Return to home page Forward to criteria for Acceptance GP Referrals MRI Is patient younger than 16 years Criteria for Acceptance of Direct GP Referrals for Lumbar Spine MRI (local agreement) Routine referral Sciatica • Patients over 16 with sciatica, defined as pain radiating below the knee, showing no improvement within 4 weeks of onset, with sensory deficit or genuine positive straight leg raise. Spinal Claudication • Patients with symptoms suggesting spinal claudication (stenosis). (Pain, weakness or numbness in one or both legs, present on walking, eased by sitting or bending forward, lower limb circulation normal) Urgent Referral • Patients with sciatica and a developing motor deficit should be referred simultaneously for an urgent MRI scan and a surgical opinion. This should be specified on the MRI referral form so that it will be expedited and result made available for the clinic appointment. • NB an absent ankle reflex in isolation is not a motor deficit Clinical conditions excluded from pathway • Suspected acute cauda equina syndrome should be managed as emergency • Patients with Mechanical LBP should NOT be routinely referred as most do not require or benefit from MRI scanning Return to LBP Pathway Return to home page Signs and Symptoms Simple low back pain Nerve root pain • Presentation 20-55 years • Lumbosacral buttock and thigh pain • Mechanical pain • Patient well Spinal stenosis • Referred leg pain, could be uni or bilateral • Reproduced on walking/standing • Better/disappear with sitting • May not have neuro signs • Vascular claudication should be ruled out Patient Primary Care Secondary Care • Unilateral leg pain worse than back pain • Radiates past knee • Numbness or Paraesthesia in dermatomal distributions • Segmental motor deficit • Limitation of SLR with production of pain • May have specific neurological symptoms incriminating single nerve root • May have hyporeflexia Return to NHS LBP Pathway Forward to GP management advice LBP/Nerve root Signs Forward to Physiotherapy referral criteria LBP/Nerve root Signs Return to home page GP Management and Advice Low Back Pain/Leg Pain Primary Care Management of Acute Low Back Pain • • • • Diagnostic triage: – – – – Provide reassurance, advise to stay as active as possible and to continue normal daily activities Increase their physical activities progressively over a few days or weeks, stay at work if possible or return to work as soon as possible. Address any additional yellow flag signs: – – – – – – – • • • • • • • Simple backache Nerve root pathology Serious spinal pathology Rule out Red Flags Attitudes & beliefs about back pain Behaviour Compensation issues Diagnosis & treatment Emotions Family Work Do not recommend or use bed rest as a treatment. Some patients may be confined to bed for a few days as a consequence of their pain, but this should not be considered a treatment. Issue advice sheet, Encourage self management. Advise that nerve root pain may take several months to settle. 90% of back pain should improve within 6 weeks. Symptomatic measures, local ice or heat Prescribe analgesics at regular intervals (not prn) Self referral to Physiotherapy: should be considered for patients who have not returned to ordinary activities and work 6 weeks after onset of symptoms Return to NHS LBP Pathway NB: refer to physiotherapy earlier if Prescribing Guidance – patient acutely distressed, Forward to Referral Criteria – and/or worsening leg pain, worse than back pain Return to home page Referral Criteria and Information Nerve Root Pain and Simple Low Back Pain Direct Access Physio if Not settling within 6 weeks/ADL's affected Even if previous physio no benefit still refer for current episode of LBP Off work/carer Yellow flags Patient/clinician concern Onward specialist referral to Physio Lead/Advanced Physiotherapy Practitioner will be arranged if no improvement in 4-6 sessions For Management of continuing Chronic Low Back Pain • For longstanding chronic pain with psychosocial dominance or distress indicating a multi-disciplinary team management approach is required. • Refer to Pain Management Service Physio Lead/APP for advice/ongoing management APP will • Recommend further treatment • Order further investigations as appropriate • Onward referral as appropriate Direct access Physio APP: if patient has: no improvement in sciatica leg pain, with failed conservative management, symptoms significantly affecting quality of life And only if the patient would consider surgery: order MRI scan (GP or APP) NB Patients with chronic symptoms unchanged for 2 years or more should not be considered for surgery If there is neuropathic pain with no neuro deficit present then delay MRI request for further 4 weeks (watchful waiting) to see if neuropathic pain will improve with appropriate medication as per neuropathic pain guidelines Between 6 and 12 week point for most patients Pain Management Approach Use SCI Gateway & include the following information: • Conservative management tried (and detail) • Any history of back problems or previous operations • If patient is diabetic or pregnant Discuss with Spinal Specialist If MRI shows a significant stenosis, or a disc prolapse that could account for the patients symptoms, refer to Spinal Service for assessment If MRI shows no lesion to account for the pain If holistic pain management approach is not successful and there is a clear mechanical element to the pain (and patient is psychologically ready for an operation), consideration should be given to a referral to an Orthopaedic Spinal Surgeon if patient would consider surgery. This should be discussed with the Spinal Surgeon prior to referral. Refer to Spinal Service Use • • • • SCI Gateway & include the following information: Conservative management tried (and detail) Any history of back problems or previous operations If patient is diabetic or pregnant Include report of MRI scan, where it was performed & its correlation with presenting symptoms & signs, indicating side of pain Return to LBP Pathway Return to home page Forward to secondary care management MRI lumbar spine flowchart Adapted from Scottish Government Task and Finish Group, 2011 Secondary Care Management Out Patient Appointment with Spinal Service The Spinal Specialist should use a recognised assessment tool to review the patient for surgical treatment Lumbar Disc Prolapse with Uncomplicated Sciatica • • The majority of patients who are suitable to be operated on by a Spinal Specialist should have their surgery by 26 weeks after onset of pain (depending on specific clinical circumstances) Patients with chronic symptoms unchanged for 2 years or more should not be considered for surgery Lumbar Spinal Stenosis • • For patients whose scan demonstrates Central Canal Stenosis or Lateral Recess Stenosis – consider surgical decompression with or without fusion as required. Foraminal Stenosis or Canal Stenosis – For patients with significant symptoms of spinal claudication with positive imaging results showing Central Canal (with or without lateral recess) Stenosis, and associated Degenerative Spondylolisthesis – consider surgical decompression with or without fusion as required. Mechanical Back Pain • Surgery should not be routinely offered for mechanical back pain • Spinal Surgeons may offer a surgical service in very selective circumstances where a holistic pain clinic/conservative management approach has not been successful. • Implants must only be used where national audit data is being kept on longer-term outcomes, which should include patient selection and the need for further surgery Adapted from Scottish Government Task and Finish Group, 2011 Return to LBP Pathway Return to home page Key Information / Prescribing Guidance Key Messages Needs a specific definition of neuropathic/neurogenic pain and recommendations on suitable medications • • • • • • • Low back pain is a common problem. Simple backache: give positive messages. Advise exercise, to be physically active and to carry on with normal activities as far as possible Avoid opioids if possible. At 6 weeks, 90% of patients are much improved, if not symptom-free Red flags point to serious underlying conditions or complications Yellow flags point to possible barriers to recovery Prescribing Guidance Prescribe analgesics at regular intervals, not when required • Start with paracetamol. • If inadequate, substitute NSAIDs and then paracetamol-weak opioid compound • Finally, consider adding a short course (3-4 days) of muscle relaxant • Avoid strong opioids if possible and never more than 2 weeks • For further information refer to: Report of CSAG Committee on back pain RCGP Primary Care Management of Simple Back Pain Return to LBP Pathway Return to home page Prescribing Guidance Patient Information Nerve Root Pain and Simple Low Back Pain • www.nhs24.com • www.nhsinform.co.uk/msk • www.chronicpainscotland.org • • • • NHS Inform Back in Control NHS Inform Back Problems NHS Inform Back (PhysioTools) NHS Inform Back (Video Physio) • helpline@backcare.org.uk • BackCare iphone app- free from app store • MSK app • BackCare helpline 08451302704 Return to LBP Pathway Return to home page Further options Nerve Root Pain and Simple Low Back Pain Pain association groups information: Angus: Board Room, Arbroath Infirmary, 11-1pm, 3rd Monday of the month Dundee: Conference Centre, Kings cross Hospital, 24pm, 3rd Monday of month Perth & Kinross: Seminar Room 5, Steele Memorial Lecture Theatre, PRI. Times vary, phone for information Phone no for information: 0800 7836059 Web: www.painassociation.com Return to LBP Pathway Return to home page Persistent Low Back Pain • Lower back pain persisting over 6 months – more likely to be persistent among people who previously required time off from work because of low back pain – those who expect passive treatments to help – those who believe that back pain is harmful or disabling or fear that any movement whatever will increase their pain – people who have depression or anxiety • Consider “yellow flags” • Consider diagnosis/investigations/treatment to date • Consider compliance with any exercise programmes and/ or Physiotherapy Persistent LBP referral options Return to LBP Pathway Return to home page Referral options Persistent Low Back Pain • Consider referral to LTC management classes/local authority classes/on line courses • Consider referral to secondary care (incl MDT pain clinic) where felt clinically appropriate • Pain association groups • Psychological referrals Self Help • www.nhsinform.co.uk/msk • BackCare iphone app • BackCare helpline 08451302704 • helpline@backcare.org.uk • Surgery will not be routinely offered for mechanical back pain Return to LBP Pathway Return to home page Knee Pain Information Osteoarthritis General advice/ Red Flags Anterior Knee Pain (AKP) Bursitis Meniscal Problems Ligament Sprains MRI Criteria Patient Information Leaflets Injection advice Link to You Tube Knee Examination Return to home page Red Flags General Advice Red Flags: Indications of Possible General Advice Serious Knee Pathology (NB: some provide a warning rather than dictate a need for referral) • • • • • • • • • • • • • • Non mechanical pain Raised temperature at knee joint(s) Joint erythema Fever Lumps or bumps present around knee Past medical history of carcinoma Unwell – Unexplained weight loss Joint effusion with no obvious cause Joint effusions > 1 Joint Suspected fracture, dislocation or neurovascular compromise Unable to weight-bear Significant injury? (feeling of pop/snap, rapid swelling, inability to complete activity?) Suspected fracture, extensor mechanism failure? (Test - Can’t straight leg raise?) Patient Primary Care Secondary Care • • • • • Mechanism and duration of symptoms are important to document in knee referrals; Knee arthroscopy is usually not indicated in patients > 50 years with radiographic changes of degenerative disease; Knee arthroplasty is usually not appropriate in patients with BMI > 40; Knee effusion with no history of trauma should be referred to Rheumatology; Ongoing pain and history of previous knee arthroplasty refer to Orthopaedic Department; Mechanical patellofemoral problems should have at least 6 months trial of conservative treatment before orthopaedic referral. (refer to physiotherapy) Return to Knee Pain Information Return to home page Anterior Knee Pain (AKP) Signs and Symptoms Common 16-40 years • Often no history of injury • Retropatellar ache may also lateralize to the joint lines or all over the knee • Often bilateral • Pain with stairs, hills, sitting for long time and start up pain • Pain on squatting/kneeling • Pain also associated with active patients who do jumping activities • Pseudo-mechanical symptoms (regular but transient) • Chronic presentation • Pain on patella compression or Osmond Clark test (apply an inferior glide to the patella while the patient actively contracts quads) • Weakness on static quads contraction through range • Patient otherwise well • Effusion uncommon Adolescent knee pain • Onset usually at the beginning of the growth spurt either insidiously, or with overuse (Osgood Schlatters) • Often pain eliminates the ability to do physical activity • May continue throughout adolescence AKP Referral Criteria Primary care • Analgesia, NSAIDS • Physiotherapy (+/-podiatry/ biomechanical assessment) management only • Advice on weight loss if appropriate Imaging: XR/MRI not indicated Secondary care • Not indicated - Primary Care management only AKP Patient Information leaflet Anterior Knee Pain Patient Primary Care Secondary Care Return to Knee Pain Information Return to home page Osteoarthritis Knee (OA) Signs and Symptoms • Commonly >50 years (previous history of knee surgery reduces age range) • Pain (particularly on moving, weight bearing or at the end of the day) • Reduced range of flexion/extension with stiffness (especially after rest, or at start of day ) • Crepitus • Hard swelling (caused by osteophytes) or Soft swelling (synovial thickening/effusion/bursitis) • Reduced walking distance/Limp/Use of walking aid/ADL OA Referral Criteria Primary care • Analgesics/NSAIDs, • Walking aid, advise patient to stay as active as possible and to continue normal daily activities, • Weight loss if appropriate, ( 1:8 failure rate for surgery with BMI over 35) • Steroid injection can be done by appropriately trained GP or Physiotherapist • Physiotherapy assessment/treatment •Imaging Weight bearing XR to confirm diagnosis or if meaningful change in management would be facilitate Secondary care Significant persistent pain/disabling symptoms/decrease in function Significant OA changes on XR (Tri-compartment) that is clinically relevant NB: imaging changes correlate poorly with clinical findings and pain - changes on their own should not trigger referral for a surgical opinion. Surgical candidate :Appropriate age range/BMI Significant sleep disturbance Previous attempt at weight reduction and rehabilitation All of the above despite appropriate analgaesics • Document on referral Pain duration and Severity (night pain) Conservative treatment to date Functional limitation BMI Use of walking aid XR findings Injection Advice OA Patient Information leaflet– OA Knee Patient Primary Care Secondary Care Return to Knee Pain Information Return to home page Meniscal Problems Signs and Symptoms History of significant injury Commonly 16-50 years Feeling of a pop with twisting injury Episodes true locking (block to full extension). Episodes true giving way (associated with effusion, which gradually develops over 8 hours) Worse on WB/ twisting Localised joint line pain Positive McMurray Positive Steinman Positive Thessaly Asking patients to squat and/or duck-walk will frequently reproduce symptoms NB: No test is specific and, therefore, a combination of provocative manoeuvres should be performed Degenerative meniscal tears. Cartilage weakens and wears thin over time. • Pain • Stiffness and swelling • Catching or locking of knee • The sensation of knee "giving way" • Reduced range of motion Meniscal Problems Referral Criteria Primary care • Analgesia • Degenerate meniscal tears or acute meniscal tears with no true locking– Refer to Physiotherapy Secondary care Locked knee - Refer to MRI protocol Meniscal Problems Patient Information leaflet– Meniscal problems Patient Primary Care Secondary Care Return to Knee Pain Information Return to home page Ligament tears/sprains Signs and Symptoms Soft Tissue Injury • Any age but commonly 16-50 Tears: • Valgus / varus stress or a twist • Feeling of a pop or a snap at injury • Rapid developing effusion • Pain • Instability/ knee giving way • Inability to complete physical activity. • If ACL or PCL usually severe trauma, with laxity on Anterior drawer and Lachman’s test Sprains: • History suggestive of valgus/varus stress • Pain on movement and palpation • Absence of effusion Ligament sprains - Referral Criteria Primary care • • • • • Mechanism of injury suggestive of ligament damage Failure of initial PRICE treatment Consider impact on professional or physical activity Analgesia & NSAIDs as appropriate Refer to physiotherapy Secondary care • • Rapid haemarthrosis with knee instability Phone on call orthopaedic registrar XR prior to referral Ligament sprains Patient Information leaflet- Ligament Sprains/Strains Patient Primary Care Secondary Care Return to Knee Pain Information Return to home page Bursitis Signs and Symptoms • Swelling, tenderness, in the overlying area of the knee. • Can be associated with warmth and erythema • Usually only mildly painful. • Pain when kneeling (prepatellar bursa) or on full knee extension (Baker’s cyst) • Can cause stiffness and pain with walking. • Range of movement of the knee frequently preserved. Bursitis Referral Criteria Primary care Rest Analgesia & NSAIDs as appropriate Non infected- refer to physiotherapy Secondary care • Infected- refer to orthopaedics - Phone on call orthopaedic registrar Bursitis Patient Information leaflet– Bursitis Patient Primary Care Secondary Care Return to Knee Pain Information Return to home page MRI Criteria (Barry Oliver Consultant Radiologist, Graeme Foubister Petros Boscainos and Richard Buckley Consultant Orthopaedic Surgeons) • • MRI not indicated MRI indicated Patients under 15 or over 60 Locked knee • A knee XR must have been obtained within 6 months of MRI request • Suspected meniscal tear – – – • • (OA is very common in obese people – MRI in knees with OA often shows meniscal damage that is not treatable by arthroscopy) Any previous meniscal surgery – • • (post-operative menisci simulate meniscal tears on MRI – direct orthopaedic clinic referral is appropriate in such patients) Active knee inflammatory arthritis, unless symptoms relate to a recent injury Anterior knee pain – • (such patients are orthopaedic emergencies and should be dealt with by secondary care) Any osteoarthritis (OA) on an x-ray Obese patients with any clinical or radiographic evidence of OA – – (not to be confused with locking, this is momentary stiffness following a period of immobility – typically in obese people with patellofemoral OA) Knee dislocation or other severe acute injury – • • previous injury with Pseudolocking – • symptoms are continuous, not momentary or intermittent a locked knee lacks at least 15 degrees of extension and cannot flex to 90 degrees (such patients need urgent orthopaedic referral with a view to arthroscopy – MRI is unnecessary and delays treatment) (usually due to patellofemoral OA, chondromalacia patellae or tendon problem which may benefit from physiotherapy) Or – • medial joint line tenderness and pain worsened by external rotation at 90 degrees knee flexion lateral joint line tenderness and pain worsened by internal rotation at 90 degrees knee flexion Instability – – previous injury subsequently, knee gives way during rotation or pivoting Forward to MRI knee flowchart Return to Knee Pain Information Return to home page Flowchart For Knee GP MRI Direct Access (local agreement) Is the patient aged 15-60 years? No patient > 60 will be accepted for knee MRI YES Is the knee locked? Is this a severe acute injury? NO Consider Children's Orthopaedic or Paediatric clinic referral for children. OA is very common in those over 60 years – consider trial of symptomatic treatment. YES Urgent orthopaedic referral is indicated. MRI may delay treatment NO A knee XR must have been obtained within 6 months of MRI request Is there: Any evidence of OA on x-ray? Pseudolocking? Predominantly anterior knee pain? NO YES OA is likely cause of symptoms. Consider symptomatic treatment or physiotherapy. YES Rheumatology clinic referral may be more appropriate in the absence of a relevant injury. Is there an active inflammatory arthritis and no recent injury? NO Has there been previous meniscal surgery? NO Do clinical features indicate: instability or meniscal tear YES YES Consider Orthopaedic referral. MRI referral may be beneficial to this patient NO Consider symptomatic treatment or physiotherapy Return to Knee Pain Information Return to home page Knee Joint Injection Technique • Patient sits with knee supported in extension • Identify medial edge patella, lift up slightly by applying pressure to lateral edge. (Can also go from lateral side- Idea is to get the needle into the retropatellar pouch) • Clean area with sterets/chloroprep • Insert needle and angle laterally and slightly upwards under patella • No resistance should be felt to delivering solution • 40 mg Kenalog/5mls 1% Lidocaine or 10 mls 0.5% Chirocaine • Green or blue needle depending on size of patient • Deliver as Bolus or aspirate then inject as required • Aftercare advice: avoid undue weight bearing 1 week, then return to mobilising and strengthening exercises • NB: Physiotherapists must comply with PGD Return to Knee Pain Information Return to Injection Advice Return to home page Hip Pain Information Red Flags Hip joint pain/ Osteoarthritis Trochanteric Bursitis Patient Information Leaflets Tendinopathy Injection Advice Youtube Hip Examination Return to home page Hip Pain Red Flags Serious Pathology Urgent referral to A & E • Suspected/known hip fracture • Violent trauma (RTA/fall from height) • Inability to WB Possible Serious Hip Pathology (NB: some provide a warning rather than dictate a need for referral to orthopaedics) • • • • • • • • • Suspected Joint infection (immediate referral) Avascular Necrosis Sudden/rapid deterioration causing severe disability Constant/progressive non mechanical pain Severe unremitting night pain PMH cancer Systemically unwell Structural deformity Gross loss of movement (mobility with severe pain) Patient Primary Care Secondary Care Return to Hip Pain Information Return to home page Hip Joint Pain/Osteoarthritis (OA) Signs and Symptoms • • • • • • • • • • • • • • • • Pain localized to the groin area and the front or side of the thigh. Morning stiffness Limited range of movement of the hip (Medial (internal) rotation, flexion, abduction, extension) Pain during movement Pain on weight-bearing Difficulty putting on shoes/socks Beware of knee pain as referred pain can be associated with OA hip Labral tears Two types of hip labral tears: degenerative tears and traumatic injuries. Degenerative labral tears can be seen in the early stages of OA Traumatic labral tear: History of twisting on a weight bearing hip during activity common or participation in multi-directional high acceleration/deceleration sports. Causes immediate pain in the hip Usually located at the front of the hip joint in the groin Pinching sensation on hip flexion , ‘Snapping’ sensation Limited ROM Can be seen in association with episodes of hip dislocation or subluxation OA Hip patient information leaflet: OA Hip Patient Primary Care Secondary Care Forward to Hip Pain Referral Criteria Return to Hip Pain Information Return to home page Hip Joint Pain/Osteoarthritis (OA) Hip joint pain Referral Criteria Primary care • Analgesics/NSAIDs, Analgesia taken regularly can aid comfort with pain/ reduced ROM • Walking aid, advise patient to stay as active as possible and to continue normal daily activities • Weight loss advice if appropriate • AP pelvis X-Ray beneficial to aid diagnosis • Ensure pain not referred from lumbar spine pathologies • Physiotherapy assessment/treatment Secondary care • Disabling symptoms, • Gross OA changes on XR, • Surgical candidate (BMI over 35 consider weight loss strategies) • Document on referral – – – – – – – – Duration of symptoms and any cause of onset Pain spread and severity (constant/ intermittent/ night pain) Conservative treatment to date Use of walking aid Functional limitation XR findings Restriction of internal rotation BMI OA Hip patient information leaflet: OA Hip Patient Primary Care Secondary Care Return to Signs and Symptoms Return to Hip Pain Information Return to home page Trochanteric Bursitis Signs and Symptoms • Pain lateral aspect hip on walking • Inability or difficulty lying in comfort on the affected side. • Tenderness on palpation of greater trochanter • Chronic nature most common • Rarely presents with swelling/warmth or erythema • ?Tight Ilio Tibial Band (Obers manoeuvre) • Self limiting condition, However a small but likely significant sub-population appear to continue to have ongoing difficulties despite management. Attests to stubborn nature of condition Trochanteric Bursitis Referral Criteria Primary care • • • • Should be managed in primary care only Analgesia & NSAIDs as appropriate Physiotherapy Steroid injection Secondary care • Not required Trochanteric Bursitis Patient Information leaflet– Trochanteric Bursitis Patient Primary Care Secondary Care Injection advice Return to Hip Pain Information Return to home page Tendinopathy Signs and Symptoms • Pain on origin or proximal few centimetres of major tendons • Common adductors into groin that can radiate down the leg • Common flexors arising anteriorly • Common hamstring origin deep into buttocks off tuberosities • Pain on resisted movements at tendon origin • Difficulty in running especially sprinting or changing direction. • Injury suggestive of muscle/tendon injury Beware of other pathologies such as • Inguinal hernia • Femoral hernia • Hip pathology (OA/Labral tear) • Pain due to tendinopathy is usually worse during and after activity, and the tendon and joint area can become stiffer the following day as swelling impinges on the movement of the tendon. Recurrence of injury in the damaged region of tendon is common. Tendinopathy Referral Criteria Primary care • Eccentric loading exercises currently advocated. • Analgesia & NSAIDs as appropriate • Steroid injection • Physiotherapy referral: Patients who fail to respond to 10-14 days relative rest/avoidance of aggravating exercise coupled with appropriate analgesia • Chronic presentation: The potential for chronicity is high as well as resistance to treatment. . Secondary care Rarely needed Tendinopathy Patient Information leaflet Patient Primary Care Secondary Care Injection advice Return to Hip Pain Information Injection Advice Tendinopathies • Identify origin of tendon Adductor • Patient lies supine with leg slightly abducted and laterally rotated Hamstring • Patient lies on unaffected side with upper leg flexed Trochanteric Bursa • Patient lies on unaffected side • Identify tender area over greater trochanter • Clean area with sterets/chloroprep • Insert needle perpendicularly at centre of tender area and touch bone of greater trochanter • 40 mg Kenalog/5mls 1% Lidocaine or 10 mls 0.5% Chirocaine • Green or blue needle depending on size of patient • Deliver as bolus when no resistance felt • • • • • • 40 mg Kenalog/2 mls lidocaine Green needle Clean area with sterets/chloroprep Insert needle into mid point of tendon and angle upwards towards bone Pepper solution into teno-osseous junction of tendon Aftercare advice: avoid overuse 1 week then gradually return to stretching and strengthening programme and normal activity NB: Physiotherapists must comply with PGD Return to Hip Pain Information Return to Injection Advice Return to home page Wrist and Hand Pain Information Carpal Tunnel Syndrome De Quervain’s Cubital tunnel syndrome Ganglion Red flags Trigger finger/ thumb OA CMC joint Dupuytren’s Non Specific hand pain Patient Information Leaflets Youtube Wrist & Hand examination Return to home page Red Flags Wrist and Hand Immediate referral to Secondary Care • • • • Sepsis/infection Fracture Tendon rupture Acute ischaemia (not Raynaud’s) Return to Wrist and Hand Pain Information Return to home page Patient Primary Care Secondary Care Carpal Tunnel Syndrome (CTS) Signs and Symptoms (Median Nerve entrapment) Tingling and numbness in lateral (radial) 3 1/2 digits- median nerve distribution May be associated with hand/ wrist/ forearm pain Dropping items/clumsiness/weakness of pinch grip +/- Weakness in abductor pollicis brevis, +/- Wasting in abductor pollicis brevis Wake up at night & relieved with movement for 15-20 minutes Positive Tinel’s: (i.e. produces symptoms) Positive Phalen’s: (i.e. produces symptoms) CTS Referral Criteria Primary care • • • • • Exclude cervical radiculopathy Wrist/ night splints - can be bought from Boots/Allardyce/PhysioMed (cock up splint) or supplied by orthotics May resolve or significantly improve in up to 49% of cases (Padua 2001). Physiotherapy referral May respond to steroid injection (by appropriately trained practitioner) Secondary care • • • If symptoms persistent, severe, especially if associated with weakness / muscle wasting: Refer for nerve conduction studies prior to secondary care referral for surgical decompression (hand service) Include the following information: – – – – – – – • Duration of symptoms Conservative management tried (e.g. any relief through splintage?) Any history of neck problems If patient is diabetic, pregnant or has a thyroid disorder If symptoms are unilateral or bilateral If motor weakness is present Results of Nerve Conduction Study should be attached CTS Patient Information leaflet– Carpal Tunnel Patient Primary Care Secondary Care Forward to referral criteria Return to Wrist and Hand Pain Information Cubital Tunnel Syndrome Signs and Symptoms (ulnar nerve entrapment) • • • • • • • Pain, tingling and numbness in ulnar 1 1/2 digits (small and ring finger) Can be provoked by leaning on elbow or keeping elbow bent (e.g. on telephone) +/-Weakness in thumb and finger adduction +/-Wasting in hypothenar eminence, interossei Wake up at night & relieved with movement for 15-20 minutes Dropping items Positive Tinel’s medial elbow (May be positive anywhere along the course of the peripheral nerve that is compromised) Cubital tunnel syndrome Referral Criteria Primary care • • Advise avoidance or modification any provocative activity where appropriate .e.g, wear headset for using telephone; avoid leaning on elbows or wear protective pads. Advise sleeping with arms straight if possible. Resting night splint (towel splint)/possibly referral to Occupational therapy for bespoke elbow extension splint.. Physiotherapy referral Secondary care referral • • • If symptoms persistent, severe, especially if associated with weakness / muscle wasting: Refer for nerve conduction studies before referral (hand service) Include the following information: – – – – – – Duration of symptoms and any cause of onset Conservative management tried (e.g. any relief through activity avoidance?) Any history of neck problems If symptoms are unilateral or bilateral If any motor weakness is present Results of Nerve Conduction Study should be attached Cubital tunnel syndrome Patient Information leaflet– Cubital Tunnel Patient Primary Care Secondary Care Return to Wrist and Hand Pain Information Return to home page Trigger Finger/Thumb Signs and Symptoms • Typical nodule at base of thumb or finger • Wake up with flexed finger or thumb which can be straightened with a click • Triggering or locking • Pain base finger/thumb • Progresses to triggering/locking on flexion activity • HOWEVER - Spontaneous recovery may occur in up to 29% of patients Trigger finger Referral Criteria Primary care • Modification of activity to avoid pressure on this area (e.g. adjust grip) • Analgesia & NSAIDs as appropriate • Refer to Hand Therapist for splint • Steroid injection into flexor tendon sheath usually successful (70%, less if diabetic) – Can be done by appropriately trained practitioner – May be repeated once if initial injection gives only temporary relief Secondary care • Refer to hand service for release trigger finger/thumb if failure to respond to first line treatment Trigger Finger Patient Information Leaflet: Trigger Finger Patient Primary Care Secondary Care Injection Advice Return to Wrist and Hand Pain Information Return to home page OA CMC joint Signs and Symptoms • Pain at base of thumb on movement of CMC joint • Reduced range of movement (abduction and extension) • Pain on grinding CMC joint OA CMC joint Referral Criteria Primary care • Non steroidal anti-inflammatory drugs/analgesia • Modify activity/ Consider hand therapy referral • Splint – (wrap around thumb splint) can be bought from Boots/Allardyce/PhysioMed • Hand therapy to aid with pain relief/ ROM • Steroid injection can be done by appropriately trained GP/Physio Secondary care Consider referring for opinion on surgery if • Gross OA changes on XR and symptoms increase despite conservative treatment • Significant problem with function • Refer to hand service • Include the following information: – – – – – – Duration of symptoms Conservative management tried (e.g. any relief through activity avoidance/ splintage/ physiotherapy/ steroid injection?) Movement loss Functional limitations Pain severity (constant/ intermittent/ waking at night) XR findings OA CMC joint Patient Information leaflet OA CMC joint Patient Primary Care Secondary Care Injection Advice Return to Wrist and Hand Pain Information Return to home page De Quervain’s Signs and Symptoms • • • • • Pain, tenderness, and swelling over the radial aspect of the wrist Maybe associated with ganglion Pain on extension/abduction of thumb, may be associated with crepitus on movement Difficulty lifting/gripping Positive Finklestein’s test (test by wrapping patient’s fingers around thumb then pull wrist into ulnar deviation) De Quervain’s Referral Criteria Primary care • Conservative management: • Analgesia & NSAIDs as appropriate • Splints (wrap around thumb splint) can be bought from Boots/Allardyce/PhysioMed • Steroid injection into 1st dorsal compartment can be done by appropriately trained GP/Physiotherapist • Refer to physiotherapy Secondary care • Failure to respond to injection/conservative treatment • Include the following information: – – – – – – Duration of symptoms and any cause of onset Conservative management tried (e.g. any relief through activity avoidance/ splintage/ physiotherapy/ steroid injection?) Movement loss Functional limitations Pain severity (constant/ intermittent/ waking at night) Any associated crepitus on thumb movements/ ganglion De Quervain’s Patient Information leaflet– De Quervain's Patient Primary Care Secondary Care Injection advice Return to Wrist and Hand Pain Information Return to home page Ganglion Signs and Symptoms • Harmless and can safely be left alone • Often there are no symptoms other than noticeable cystic swelling. • Occasionally can cause pain and limited joint movement. Ganglion Referral Criteria • Common • If it is not painful, no treatment is required. • Analgesia as appropriate if painful- simple wrist wrap around splints may help if appropriate (Allardyce/ Boots/Physiomed) • About 50 % disappear without any treatment • Aspiration (50% recurrence) Do not repeat aspiration if ganglion recurs • Concern about cosmetic appearance is not an indication for referral. Further information to consider and discuss with patient prior to secondary care referral • Dorsal Ganglion cyst. Typically occurs in young adults and often disappears without treatment. Draining it can reduce the swelling but it often returns. Risk of recurrence after surgery around 10%, problems post op include persistent pain, loss of wrist movement and painful trapping of nerve branches in the scar. • Volar Ganglion cyst. May occur in young adults, but also seen in association with arthritis in older individuals. Aspiration may be useful, but care needed as the cyst is often close to radial artery. Risk of recurrence after surgery is around 30%, problems post op include persistent pain, loss of wrist movement and trapping of nerve branches in the scar. For these reasons, many surgeons advise against operation for these cysts. • Ganglion cyst at the base of volar surface finger (Flexor tendon sheath). Typically occurs in young adults, causing pain when gripping and feeling like a dried pea sitting on the tendon sheath at the base of the finger. Persistent cysts can be removed surgically - risk of recurrence is small. • Mucous cyst. Usually in middle-aged or older people, associated with wearing out of DIP joint. Pressure from the cyst may cause a furrow in the fingernail. Occasionally the cyst fluid leaks through the thin overlying skin from time to time. Risk of recurrence post op around 10%, problems after surgery include infection, stiffness and pain from the worn out joint. Ganglion Patient Information leaflet – Ganglia Patient Primary Care Secondary Care Return to Wrist and Hand Pain Information Return to home page Dupuytren’s Contracture Signs and Symptoms • Common • Usually arises in middle age or later • More common in men than women. • Characterised by cords and nodules in palmar aponeurosis • Finger flexion develops over months/years • Nodules over back of the PIP joints (Garrod's pads) • Not usually painful Dupuytren’s Contracture Referral Criteria Primary care • No cure. • Palmar nodule only: no active treatment required Secondary care • If patient can get hand flat on the table top there is no indication for referral • If fixed contracture 15° at PIP joint, or 15-30 ° MCP joint refer for surgery (either Plastic surgery or Orthopaedics) • Xiapex (collagenase injections) or needle fasciotomy are only indicated for similar levels of contracture Dupuytren’s Contracture Information leaflet– Dupuytren's Return to Wrist and Hand Pain Information Return to home page Patient Primary Care Secondary Care De Quervain's • Injection Advice • • • • • Rest patient’s hand on edge of pillow so it lies in slight ulnar deviation Identify gap between APL and EPB Clean area with sterets/chloroprep Blue/orange needle Insert needle into gap between the two tendons Inject as bolus • Up to 40 mg Kenalog/2 ml lidocaine Trigger finger/thumb • • • • • Patient places palm up, hand supported Identify nodule at A1 pulley Clean area with sterets/chloroprep Insert needle approx 45°distally or proximally into nodule Avoid injecting into tendon by withdrawing needle slightly until no resistance felt to delivering solution • Up to 40 mg Kenalog/1ml Lidocaine into nodule or flexor sheath Orange or blue needle • • Aftercare advice: relative rest 2 weeks. i.e. Avoid strong gripping, heavy lifting • NB Physiotherapists must comply with PGD Return to Wrist and Hand Pain Information Return to Injection Advice Return to home page Injection Advice OA CMC joint OA CMC joint • • • Patient rests hand in mid position (thumb up) Apply traction to open up joint space Identify gap of joint space at apex of snuff box • Clean area with sterets/chloroprep • • • Blue/orange needle Insert needle perpendicularly into gap Inject as bolus • Up to 40 mg Kenalog/1-2 ml lidocaine • Aftercare advice: relative rest 2 weeks i.e. Avoid strong gripping, heavy lifting • NB Physiotherapists must comply with PGD Return to Wrist and Hand Pain Information Return to Injection Advice Return to home page Elbow pain Information Tennis/Golfers Elbow Post traumatic elbow stiffness Injection Advice Patient Information Leaflets Youtube Elbow examination Return to home page Tennis/Golfers elbow Signs and Symptoms Tennis • Recurring pain on the lateral aspect elbow; occasionally, pain radiates down the arm toward the wrist. • Localised tenderness extensor origin • Increased pain on wrist dorsiflexion • Pain caused by lifting or bending the arm or grasping light objects. Golfers • Recurring pain on the medial aspect elbow; occasionally, pain radiates down the arm toward the wrist. • Localised tenderness flexor origin • Increased pain on wrist palmar flexion • Pain caused by lifting or bending the arm or grasping light objects. Both Tennis/Golfers Elbow • Difficulty extending or flexing the forearm fully • Benign Self limiting conditions: Pain typically lasts for 6 to 12 weeks; the discomfort can continue for as little as 3 weeks or as long as several years. Tennis/Golfers Elbow Referral Criteria Primary care • Advice / reassurance / Analgesia & NSAIDs as appropriate • Benign self limiting condition • Modify loading • Symptomatic measures (steroid injection / physio / splints) • Epicondylitis clasp can be bought from Boots/ Allardyce/PhysioMed • Eccentric loading exercises advocated- refer Physiotherapy Secondary care • Surgery if failure to respond to physiotherapy and at least 2 steroid injections • Information to include when referring – – – Duration of symptoms Indicate site/spread of pain and if constant or intermittent, and/or waking at night Include treatment to date (injections/ physiotherapy) Tennis/Golfers elbow Patient Information leaflet– Tennis Elbow Patient Primary Care Golfers Elbow Secondary Care Injection Advice Return to Elbow Pain Information Return to home page Post Traumatic Elbow Stiffness Signs and Symptoms • Common • Usually improves with time and use • Functional arc usually achieved 30-130º extension/ flexion Post traumatic elbow stiffness Referral Criteria Primary care • Reassure and advise to mobilise (active movements only, no passive stretching) • Analgesia & NSAIDs as appropriate • Refer to physiotherapy Secondary care • If significant stiffness (greater than 45º loss of extension or 115º flexion or less) and functional problem with no improvement after 6 months • Refer for consideration of surgical release • XR prior to referral • Information to include when referring – – – – – Duration of symptoms and any cause of onset Indicate site/ spread of pain and if pain constant or intermittent, and/or waking at night Indicate ROM and any crepitus on movement Include treatment to date XR results/Dominance Post traumatic elbow stiffness Patient Information leaflet – General Elbow Stiffness Patient Primary Care Secondary Care Return to Elbow Pain Information Return to home page Injection Advice Tennis elbow - common extensor origin • • • • Lateral side right arm • Patient sits with forearm supported 90° elbow flexion and supinated Identify lateral epicondyle then move anteriorly on to facet Clean area with sterets/chloroprep Insert needle in line with cubital crease perpendicular to facet to touch bone Pepper solution into tendon insertion Golfer’s Elbow - common flexor origin • • • • • Medial side left arm Patient sits with forearm extended Identify facet lying anteriorly on medial epicondyle Clean area with sterets/chloroprep Insert needle perpendicular to facet and touch bone Pepper solution into tendon insertion Up to 40 mg Kenalog/2 ml Lidocaine into common flexor or extensor origin Blue or orange needle Peppering technique Aftercare: relative rest for a week, then stretching and strengthening exercises • NB Physiotherapists must comply with PGD Return to Elbow Pain Information Return to Injection Advice Return to home page Cervical Spine, Shoulder & Arm Pain Information Red Flags Shoulder Impingement Red Flags Cervical Spine Adhesive capsulitis Rotator cuff tears Instability/ Recurrent dislocation Neck/Arm Pain Patient Information Leaflets Cervical Spine Patient Information Leaflets Shoulder You tube Shoulder Assessment Return to home page Red Flags Shoulder Possible Serious Shoulder Pathology (NB: some provide a warning rather than dictate a need for referral to orthopaedics) • • • • Unexplained soft tissue mass/swelling Constant/progressive non mechanical pain Severe unremitting night pain PMH cancer – • Erythema/fever/systemically unwell – • • • • tumours: 7% of bony metastases occur in the proximal humerus Septic arthritis: rare in the shoulder (less than 0.01%) Inflammatory arthropathy: e.g. rheumatoid arthritis, gout and psoriatic arthropathy. Consider polymyalgia rheumatica in patients over 60 years of age Fracture/dislocation: usually history of trauma and sudden onset of pain. NB osteoporotic patients. Unexplained significant sensory or motor deficit Rule out non MSK issues – Patient visceral disease: any condition that irritates the mediastinal pleura, pericardium or diaphragm can cause shoulder pain. Consider myocardial ischaemia Primary Care Secondary Care Return to Neck, Shoulder and Arm Pain Information Return to home page Impingement Signs and Symptoms Subacromial Impingement Injection Advice • Pain on overhead activities and/or abduction. • Pain is more likely anterior shoulder and may radiate to the side of the arm. • A painful arc of movement- less pain on passive movement • Weakness due to pain usually in abduction and/or lateral rotation • Loss of movement at the affected shoulder • Shoulder pain at night AC • • • • joint Impingement Injection Advice Localised tenderness over AC joint End range pain passively in all directions Possible painful arc 150-180º NB: Surgery rarely performed for AC joint dislocation Impingement Referral Criteria Primary care • Pain control Analgesia & NSAIDs as appropriate • Physiotherapy • Subacromial / AC joint steroid injection by appropriately trained GP or physiotherapist Secondary care • Symptoms for 6-12 months. • Failure of conservative treatment (at least 2 steroid injections) and protracted course of physiotherapy. • X-Ray prior to referral +/- dynamic USS • Information to include when referring – – – – – Duration and any cause of symptoms Indicate site/ spread of pain and if pain constant or intermittent, and/or waking at night Indicate ROM (+/- painful arc) Include treatment to date XR results Impingement Patient Information leaflet–Impingement Patient Primary Care Secondary Care Return to Neck, Shoulder and Arm Pain Information Adhesive Capsulitis Signs and Symptoms • Active and passive reduced ROM, specifically loss of external (lateral) rotation, with normal XR (can be stiff in all directions) • Pain can radiate to elbow/wrist Self-limiting condition: highly variable in terms of presentation and duration • “Freezing" or painful stage, may last from six weeks to nine months, and in which the patient has a slow onset of pain. As the pain worsens, the shoulder loses movement. • “Frozen" or adhesive stage is marked by a slow improvement in pain but the stiffness remains- can last from four to nine months. • “Thawing" or recovery, when shoulder motion slowly returns towards normal- can last from 5 to 26 months Adhesive Capsulitis Referral Criteria Primary care • Reassure and advise to mobilise. • Pain control - Analgesia & NSAIDs as appropriate • Physiotherapy • Glenohumeral joint steroid injection by appropriately trained GP or physiotherapist (Up to three injections). • Self limiting condition Secondary care Only if failure to improve for 6-9 months. • Refer for distension arthrography / manipulation under anaesthetic/surgical release. (Consider referral sooner if patient diabetic or has association with Dupuytren's and failure to respond to initial interventions) • Information to include when referring – – – – – Duration and any cause of symptoms Indicate site/spread of pain and if pain constant or intermittent, and/or waking at night Indicate ROM Include treatment to date (injections/ physiotherapy) XR results Adhesive Capsulitis Patient Information leaflet– Adhesive Capsulitis Patient Primary Care Secondary Care Injection Advice Return to Neck, Shoulder and Arm Pain Information Return to home page Rotator Cuff Tears Signs and Symptoms • • • • • • Limited active range of movement, specifically during abduction Sporadic worsening of pain, debilitation Weakness, that is not due to pain, usually in abduction or lateral rotation Atrophy of rotator cuff on looking at scapula musculature Noticeable pain during rest Crackling sensations or soft tissue crepitus when moving the shoulder Rotator Cuff tears Referral Criteria Primary care • • • Pain control - Analgesia & NSAIDs as appropriate Subacromial steroid injection by appropriately trained GP or physiotherapist (Up to three) Refer to physiotherapy Secondary care Consider referral for Surgical opinion if: • Younger patient with traumatic tear • Failure to improve with conservative treatment • USS prior to referral to confirm extent of tear/other pathology • Information to include when referring – – – – – Duration and any cause of symptoms Indicate site/spread of pain and if pain constant or intermittent, and/or waking at night Indicate ROM (active and passive) Include treatment to date (injections/ physiotherapy) XR /USS results (NB: RC tears findings on USS may be coincidental rather than causative) Rotator Cuff tears Patient Information leaflet– Rotator Cuff Tears Patient Primary Care Secondary Care Injection Advice Return to Neck, Shoulder and Arm Pain Information Return to home page Instability/Recurrent Dislocation Signs and Symptoms • • • • History of dislocation / subluxation Multi directional instability Hypermobility Pain Instability/recurrent dislocation Referral Criteria Primary care • • Physiotherapy Pain relief - Analgesia & NSAIDs as appropriate Secondary care • • • Continuing shoulder instability despite prolonged course of Physiotherapy. XR changes Information to include when referring – – – – – – Duration and any cause of symptoms If recurrent dislocations – rough amount and frequency Indicate site/spread of pain and if pain constant or intermittent, and/or waking at night Indicate ROM loss/ excessive range Include treatment to date (physiotherapy) XR results Instability/recurrent dislocation Patient Information leaflet– Instability/Recurrent Dislocation Return to Neck, Shoulder and Arm Pain Information Return to home page Patient Primary Care Secondary Care Injection Advice Sub Acromial bursa SAB injection used for impingement or rotator cuff tears posterolateral • • • • • • Patient sits with arm hanging to distract joint Identify lateral edge acromion Aim for space under the acromion Clean area with sterets/chloroprep Can be given posteriorly, laterally or anteriorly No more than 3 injections • 40 mg Kenalog/5ml 1% lidocaine or up to 10 ml 0.5% Chirocaine into Sub Acromial Bursa Blue, green or white needle depending on size of patient Deliver as bolus when no resistance felt (may have to withdraw needle slightly) • anterior • anterolateral • NB: Physiotherapists must comply with PGD Aftercare advice: relative rest 2 weeks- Pendular exercises only, Avoid heavy lifting, repetitive activities. Then commence mobilising and strengthening exercises. Return to Neck, Shoulder and Arm Pain Information Return to Injection Advice Return to home page Injection Advice – GH Joint Glenohumeral joint for adhesive capsulitis • • • • • • Patient sits with arm folded across waist to open up posterior aspect GH joint space Identify posterior angle acromion with thumb, and coracoid process with index finger Clean area with sterets/chloroprep Insert needle below angle of acromion and push obliquely anterior toward coracoid process No more than 3 injections • • Inject as bolus. No resistance to delivering solution should be felt 40 mg (up to 80) Kenalog, 5 ml Lidocaine / 10 ml (up to 20 ml) Chirocaine into GH joint Blue or green needle depending on size of patient Aftercare advice: relative rest 2 weeks- Pendular exercises only, Avoid heavy lifting, repetitive activities. Then commence mobilising and strengthening exercises. • NB: Physiotherapists must comply with PGD • Return to Neck, Shoulder and Arm Pain Information Return to Injection Advice Return to home page Injection Advice – AC Joint AC joint impingement/pain • • • • • Patient sits supported with arm hanging to distract joint Identify edge of acromion, move medially to identify AC joint. Clean area with sterets/chloroprep Insert needle angling medially at mid point of joint line. No more than 3 injections • • • • Inject as bolus Up to 40 mg Kenalog/ 1 ml Lidocaine Orange/blue needle Aftercare advice: relative rest 2 weeks- Pendular exercises only, Avoid heavy lifting, repetitive activities. Then commence mobilising and strengthening exercises NB: Physiotherapists must comply with PGD Worthwhile tip: variability in obliquity of the AC joint, therefore have x-ray on the screen to know how obliquely to aim needle. Return to Neck, Shoulder and Arm Pain Information Return to Injection Advice Return to home page Neck Pain / Neck with Arm Pain Signs and Symptoms • • • Neck pain Common: two-thirds of the population have neck pain at some point in their lives. More frequently seen in women than men. Can range from mild discomfort to severe, burning pain with arm referral Symptoms • • • • • • • General pain located in the neck area, as well as stiffness in the neck muscles. May radiate to the shoulder or between the scapulae. May radiate out into the arm, the hand or up into the head, causing a one-sided or double-sided headache. Acute pain can give rise to torticollis. May be weakness in the shoulders and arms. May be altered sensation in the arms and fingers. May have altered reflexes Neck (and Arm) Pain Referral Guidelines Primary care • • • • • GP treatment advice if no red flags present Analgesia, NSAIDS Muscle relaxant may be prescribed on a short-term basis of up to 1 to 2 weeks depending on progress. Advise to keep moving Refer to physiotherapy if symptoms persist Secondary care: red flags Neck pain Patient Information Leaflet- Neck pain Patient Primary Care Secondary Care Return to Neck, Shoulder and Arm Pain Information Return to home page Click for Red Flags Red Flags for Neck Pain – Immediate Referral to Neurosurgery Serious underlying cause is more likely in people presenting with: • New symptoms before the age of 20 years or after the age of 55 years. • Weakness involving more than one myotome or loss of sensation involving more than one dermatome. • Intractable or increasing pain. NB Index of suspicion as many patients will say pain is increasing Red flags suggesting possible malignancy, infection or inflammation: • Fever • Unexplained loss of weight • History of inflammatory arthritis • History of malignancy, drug abuse, TB, AIDS,or other infection • Immunosuppression • Pain that is increasing, unremitting and/or disturbs sleep NB Index of suspicion as many patients will say this • Lymphadenopathy • Exquisite localised tenderness over a vertebral body • Dizziness, drop attacks Patient Primary Care Secondary Care Red flags suggesting myelopathy (compression of the spinal cord): • Insidious progression • Gait disturbance; clumsy or weak hands; loss of sexual/bladder/bowel function • Lhermitte's sign (flexing the neck causes electric shock-like sensations that extend down the spine and shoot into the limbs) • Upper motor neurone signs in the upper limbs (hyperreflexia, Hoffman’s sign) and lower limbs (hyperreflexia, clonus, spasticity, or positive Babinski's sign - up-going plantar reflex) • Lower motor neurone signs in the upper limbs (atrophy, hyporeflexia, hyperrflexia) • Variable sensory changes (loss of vibration and joint position sense more evident in the hands than in the feet) Red flags suggesting severe trauma/skeletal injury: • History of trauma • Previous neck surgery • Osteoporosis or risk factors for • Increasing and/or unremitting pain Red flags suggesting vascular insufficiency: • Dizziness and blackouts (restriction of vertebral artery) on movement, especially on extension of the neck with upward gaze • Dizziness, drop attacks Return to Neck, Shoulder and Arm Pain Information Return to home page Ankle & Foot Pain Information Ankle Osteochondral lesion Metatarsalgia Differential Diagnosis Possible Serious Pathology Indicators History and Examination Ankle Osteoarthritis Morton’s Neuroma Plantarfasciitis Ligament Sprains Tibialis Posterior Dysfunction Impingement Peroneal Tendinitis Patient Information Leaflets Ankle examination Hallux Rigidus Hallux Valgus Achilles Tendinopathy/ Posterior heel pain Return to home page Musculoskeletal – Foot and Ankle Patient Pathway In all cases: analgesia & NSAIDs as appropriate Patient Presentation Hallux valgus (Bunions) • Lateral deviation of hallux • Become symptomatic with ill-fitting shoes • Bursitis forms over medial prominence, may ulcerate • Secondary corns and callous Primary Care Orthopaedic Consultant Referral • Education on footwear/ extra-width shoes • Care of secondary lesions. Refer? • • • • Refer? • Pain either due to pressure effects of the dorsal osteophytes or degenerate joint • Failure of conservative treatment Refer? • Failure of conservative treatment • Fixed toe deformities • Morton’s neuroma not responded to steroid injection Refer? Mainstay of treatment is conservative: if unsuccessful, should be referred for surgical excision of bursa / decompression of Achilles tendon Refer? • 80% self-limiting, resolving within 12-18 months • Surgery is rarely indicated Evidence base does not support use of orthoses to limit progression Hallux rigidus • Inshoe orthoses/ rigid insoles/ rocker sole • Intra-articular steroid injections and/or mobilisation • Degenerative osteo- arthritis of 1st MTP joint • Pain during and following activities • Restriction of movement in joint • Dorsal exostosis • Transfer metatarsalgia due to a stiff 1st MTJP Metatarsalgia General pain under metatarsals • MTP joint synovitis/instability • Intermetatarsal bursitis • MTP joint arthritis • Painful plantar callosities Morton’s Neuroma • Paroxysmal neuralgia affecting web spaces and 2/3/4 toes • Mainly a clinical diagnosis and further investigations are done as indicated. April 2005 • Advice re footwear (avoid heels and tight fitting shoes) • Custom made orthoses • Injection of steroid into the affected interspace or MTP joint(s) Pain should be the primary indication for surgery Difficulty obtaining suitable shoes Recurrent ulcers Infection Posterior Heel Pain (i) Pump bumps • Prominent posterior aspect of calcaneum (illustrated) (ii) Achilles Tendinosis • Tenderness/swelling proximal to insertion of tendon to posterior calcaneum (i) Simple padding and foot wear advice (ii) - Stretching programme - Heel raises/ inshoe orthoses Plantar Heel Pain (i) Plantar pad • Fat pad atrophy with non-specific pain under heel (ii) Plantar fasciitis • Pain is worse on taking first steps in morning • Tenderness at attachment of PF to medial calcaneal tubercle (illustrated) • Spurs are not significant and therefore X-rays are not indicated Midfoot arthritis (i) Heel cushions (ii) - Regular calf/ plantar fascia stretching - In shoe orthoses - Steroid injection - Night splints • Footwear modification • Pain and stiffness • Local tenderness • Loss of medial longitudinal arch • Acute injury – Rest, Ice, Compression and Elevation (RICE) • X-ray if fracture suspected • Taping • Proprioceptive/ balance exercises • Semi rigid ankle orthoses reduce reoccurrence Lateral ankle sprains • Lateral ankle pain, swelling and giving way Patient Primary Care Secondary Care Refer? • Surgical fusion is necessary if the orthotic management is unsuccessful Refer? • No indication for surgery after acute ligament injuries • Chronic pain and instability need further imaging and may require surgical reconstruction www.cci.scot.nhs.uk Useful Information for Patients www.patient.co.uk Ankle and Foot Possible Serious Pathology Indicators Possible Serious Pathology Unusual deformity or effusion Signs of septic arthritis, fever, chills, hot, swollen joints Inability to weight bear due to pain Previous history of cancer or suspected malignancy Unremitting night pain Achilles tendon rupture - unable to calf raise, palpable gap in tendon, positive Thomson’s test Indicators that a more in depth history, clinical examination and investigations may be required: Sudden onset of reduced range of motion, sensory or motor deficit without pain Neurovascular conditions, referral from the spine Inability to weight bear due to pain Management As appropriate Return to home page Ankle & Foot Pain Informati Return to Ankle and Foot Pain Information Ankle and Foot Differential Diagnosis Presentation Referral from the lumbar spine RA, tumour, septic arthritis, inflammatory condition Infection, coalition, neuropathy, stress fractures Features Inflammatory arthritis Consider previous episodes (Gout) If other peripheral joints or spine affected: consider sero-negative arthritis Spontaneous ankle or foot joint effusion, no history of trauma: refer to rheumatology Specific Investigations: FBC, CRP, PV; if acute attack: urate level Management As appropriate Return to home page Return to Ankle and Foot Pain Information Ankle and Foot Pain History and Examination History Age of patient, occupation and hobbies Symptoms, pain location, foot and ankle range of motion, weakness, numbness or altered sensation, giving way or instability, locking, swelling, Onset of symptoms, injury, trauma, Pain location, intensity, duration, aggravating and easing factors, night pain, effect on ADLs/work History, PMH, systemic symptoms (fever, abdominal, cardiovascular), previous treatments/surgery, medication Examination Investigations as indicated Observation Radiographs Posture, lower limb alignment, foot position, deformity, swelling, Radiographs (foot and ankle) New onset of pain older than 50 years Serious injury, osteoporosis, sensory or motor loss, rheumatological disease Painful foot deformity Weight loss, past medical history of cancer, night pain, fever longer than 48 hrs. Foot and/or ankle joint effusion. Palpation Local areas of pain, medial and lateral ligaments, ankle joint line, Achilles tendon Range of Movement Active and passive motion foot ankle dorsiflexion, plantarflexion, inversion, eversion Functional tests i.e. heel raise, squat, instability tests, Neurovascular assessment if indicated Consider when symptomatic measures have been insufficient for patient’s symptoms: Blood investigations: C-reactive protein, plasma viscosity, FBC, U&Es, Liver function urate acid tests Return to home page Return to Ankle and Foot Pain Information Ankle Impingement Signs and Symptoms • • • • Can be anterior or posterior impingement. Bone spurs can either form on the end of the tibia, on the talus, or on both. Local pain, usually following repetitive microtrauma, infection. ? Locking, giving way or catching at ankle. Referral Criteria Primary Care • • • • • Footwear modification. Inshoe orthoses, (heel wedges) accommodation and padding Pain medication Analgesia & NSAIDs as appropriate Refer to podiatry or physiotherapy service Steroid injection by appropriately trained GP/Physiotherapist and/or mobilisation Primary Care Diagnostics Radiographs: Ankle AP standing and lateral views, blood tests if inflammatory arthropathy suspected Secondary care Failure of conservative treatment Patient Primary Care Secondary Care Return to home page Return to Ankle and Foot Pain Information Ankle Osteoarthritis Signs and symptoms •Can be talocrural, subtalar or midfoot •Complain of swelling, catching, locking, Pain and stiffness •Local tenderness •Loss of medial longitudinal arch •Reduced ability or increased pain on moving or weight bearing Referral Criteria Primary Care Management •Advice regarding footwear, weight loss if appropriate, walking aids •Analgesia & NSAIDs as appropriate •Refer to podiatry/physiotherapy Secondary Care Management •Refer if no improvement in long term with persistent pain -?Surgical fusion required •Radiographs prior to referral: Ankle AP standing and lateral views Patient Primary Care Secondary Care Return to home page Return to Ankle and Foot Pain Information Ankle Osteochondral Lesion Sometimes called osteochondritis dessicans or osteochondral fractures Signs and Symptoms •Usually have a history of injury, single or repeated •Pain may be diffuse or local and prolonged felt primarily at the lateral or medial aspect of the ankle joint. Severe •Swelling, catching and/or instability of the ankle joint. •After an injury such as an ankle sprain, the initial pain and swelling should decrease with appropriate recovery (PRICE). •Persistent pain despite appropriate treatment after several months may raise concern for an OLT. Diagnosis is one of suspicion, after ruling out other pathologies Referral Criteria Primary Care • Immobilisation- Splinting/bracing- and restricted weight bearing • Analgesia & NSAIDs as appropriate • Refer Podiatry, Physiotherapy Secondary Care • • Refer if no improvement after 3 months (MRI or CT scan may be required) XR prior to referral: Ankle AP standing and lateral views Patient Primary Care Secondary Care Return to home page Return to Ankle and Foot Pain Information Hallux Rigidus Signs and Symptoms • Degenerative osteoarthritis of 1st MTP joint • Local tenderness and pain during and following activities • Restriction of movement in great toe • Dorsal exostosis • Transfer metatarsalgia due to a stiff 1st MTP Joint • Midfoot arthritis • Loss of medial longitudinal arch Referral Criteria Primary Care • Footwear modification: wear shoe with rigid sole, wide toe, avoid heels • Inshoe orthoses/ rigid insoles/ rocker sole: refer orthotics service • Analgesia & NSAIDs as appropriate • Refer to podiatry, physiotherapy service • Intra-articular steroid injections by appropriately trained GP/Podiatrist/Physiotherapist and/or mobilisation Secondary care • Pain either due to pressure effects of the dorsal osteophytes or degenerate joint • Failure of conservative treatment • Surgical joint replacement/fusion may be necessary if conservative management is unsuccessful Hallux Rigidus Patient Information leaflet- Hallux Rigidus Patient Primary Care Secondary Care Injection Advice Return to Ankle and Foot Pain Information Return to home page Hallux Valgus Signs and Symptoms • • • • • • • • • • 33 per cent of people will develop hallux valgus at some stage in their lives - more common in females Not all bunions are painful- can have large bunions without significant pain. Becomes symptomatic with ill-fitting shoes Deviating great toe can cause pressure on the second toe, resulting in the second hammer toe. Irritated skin around the bunion – may ulcerate Joint redness and pain – secondary corns and callous Blisters may form more easily around the site of the bunion- sometimes becomes infected Pain during walking and following activities Restriction of movement in great toe joint Can lead to mechanical function problem of the forefoot Referral Criteria Primary Care • • • • • • Footwear modification: avoid high heels, pointed or tight fitting shoes. Advise extra width shoes with laces or straps, as can be adjusted to the width of the foot. Inshoe orthoses, accommodation and padding Pain medication Analgesia & NSAIDs as appropriate Intra-articular steroid injection by appropriately trained GP/Physiotherapist and/or mobilisation Refer to podiatry or physiotherapy service Secondary care • • • • • • Pain either due to pressure effects or degenerate joint Failure of conservative treatment Surgical joint replacement/fusion may be necessary if conservative management is unsuccessful Recurrent ulcers Difficulty obtaining suitable shoes (orthotics) Infection Hallux Valgus Patient Information leaflet– Hallux Valgus Patient Primary Care Secondary Care Injection Advice Return to Ankle and Foot Pain Information Return to home page Ligament Sprains Signs and Symptoms • Lateral ankle pain - Can be acute or chronic, usually following an inversion injury • May complain of giving way, recurrent sprains, pain, stiffness, locking or swelling if chronic Ligament sprains Referral Criteria Primary care • Acute injury – Protect, Rest, Ice, Compression and Elevation (PRICE) • Analgesia & NSAIDs as appropriate • Refer to Podiatry/ physiotherapy • Taping • Proprioceptive/ balance exercises • Semi rigid ankle orthoses may reduce recurrence • Imaging if appropriate: X-ray according to Ottawa rules Ankle AP standing and lateral views Secondary care • No indication for surgery after acute ligament injuries • Chronic pain and instability may need further imaging and may require surgical reconstruction • Refer if unable to weight bear Ligament Sprains Patient Information leaflet – Ankle Ligament Sprain Patient Primary Care Secondary Care Return to Ankle and Foot Pain Information Return to home page Tibialis Posterior Dysfunction Signs and Symptoms •Adult acquired flat foot deformity, gradual onset. •Can cause of mobility problems in older people. •Medial foot and ankle pain, swelling around the medial hind foot. •Lack of rear foot inversion on heel raise, flat longitudinal arch •Pain that is worse with activity. High-intensity or high-impact activities, such as running, can be very difficult. Some patients can have trouble walking or standing for a long time. •Pain lateral ankle as foot collapses. Referral Criteria Primary Care • In the acute stage PRICE treatment should be followed • Most patients can be treated without surgery, using orthotics • Analgesia or NSAIDS if appropriate • Podiatry in stages 1 and 2 (see guide) Primary Care Diagnostics • XR/Ultrasound scan Secondary Care • Refer in stages 3 and 4 or if no improvement in stages 1 and 2 (see guide) Patient Primary Care Secondary Care Return to Ankle and Foot Pain Information Return to home page Classification Tibialis Posterior Dysfunction Deformity Physical Exam Radiographs Stage 1A • Tenosynovitis • No deformity • Tendon normal length • Symptoms are usually mild to moderate. • Pain and swelling are present on the medial aspect of the foot. • Mild weakness • (+) single-leg toe raise • Normal Stage 11A • Elongation or tearing of the tendon • Flatfoot deformity • Flexible hindfoot - subtalar joint remains mobile. • Normal forefoot • (-) single-leg heel raise • Mild sinus tarsi pain • Arch collapse deformity Stage 11B • Flatfoot deformity • Flexible hindfoot - subtalar joint remains mobile. • Secondary deformity as the midfoot pronates and the forefoot abducts at the transverse tarsal joint. • Forefoot abduction ("too many toes", >40% talonavicular uncoverage) • (-) single-leg heel raise • Severe sinus tarsi pain • Arch collapse deformity • Subtalar arthritis Stage 111 • Flatfoot deformity • Rigid forefoot abduction • Rigid hindfoot valgus • (-) single-leg heel raise • Severe sinus tarsi pain • Arch collapse deformity • Subtalar arthritis Stage 1V • • • • • (-) single-leg heel raise • Severe sinus tarsi pain • Ankle pain • Arch collapse deformity • Talar tilt in ankle mortise • Early degenerative changes of the ankle - Subtalar arthritis Flatfoot deformity Rigid forefoot abduction Rigid hindfoot valgus Deltoid ligament compromise Return to Ankle and Foot Pain Information Return to home page Back to Tibialis Posterior Dysfunction Peroneal tendinitis Signs and symptoms • • • • • Common in runners or after repeated inversion injuries Pain/swelling around the lateral malleolus, probably from a non-resolving sprain or overuse. May see the tendons subluxing behind the lateral malleolus. Symptoms increase with activity and improve with rest. May complain of instability. Referral criteria Primary Care • Advise PRICE if acute injury • Analgesia & NSAIDs as appropriate •If tendon not subluxing conservative management with podiatry or physiotherapy Secondary Care • • • No indication for surgery Chronic pain and instability may need further imaging: ultrasound scan Refer if unable to weight bear Patient Primary Care Secondary Care Return to home page Return to Ankle and Foot Pain Information Plantar Heel Pain (Plantar Faciitis) Signs and Symptoms Plantar pad • Fat pad atrophy with non-specific pain under heel • • • Plantar fasciitis Usually worse on initial weight bearing in the morning, better throughout the day and increasing in the evening. Electric shock pain, reduced sensation or pain at rest indicated possible neural entrapment or lumbar spine referral. Tenderness at attachment of PF to medial calcaneal tubercle Plantar Heel Pain Referral Criteria Primary care • Spurs are not significant and therefore X-rays are not indicated • Analgesia & NSAIDs as appropriate • Heel cushions • Regular calf/ plantar fascia stretching • - Off the shelf In shoe orthosis (From Boots/Allardyce/PhysioMed) • - Steroid injection by appropriately trained GP/Podiatrist/Physiotherapist • - Prescribed orthosis/Night splints: refer Orthotics • Refer podiatry, physiotherapy clinic Secondary care • Not indicated • 80% self-limiting, resolving within 12-18 months • Surgery is rarely indicated Plantar Fasciitis Patient Information leaflet – Plantar Fasciitis Injection Advice Return to Ankle and Foot Pain Information Secondary Care Primary Care Patient Return to home page Metatarsalgia Signs and Symptoms Metatarsalgia • General pain under metatarsals • MTP joint synovitis/ instability • Intermetatarsal bursitis • MTP joint arthritis • Painful plantar callosities Metatarsalgia Referral Criteria • Primary care • Advice re footwear (avoid heels and tight fitting shoes) • Analgesia & NSAIDs as appropriate • Refer to podiatry or physiotherapy • Custom made orthosis • ?Morton’s neuroma Primary care diagnostics • Radiographs if not settling. Foot AP standing, lateral and oblique views Secondary care • Failure of conservative treatment. Refer if no improvement in long term with persistent pain and deformity • Fixed toe deformities • No surgery indicated for cosmesis Metatarsalgia Patient Information leaflet– Metatarsalgia Patient Primary Care Secondary Care Return to Ankle and Foot Pain Information Return to home page Morton’s Neuroma Signs and Symptoms • Paroxysmal neuralgia affecting web spaces and 2/3/4 toes • Pain and/or ‘clunk on Mulder’s test (squeeze midfoot joint) • Mainly a clinical diagnosis and further investigations are done as indicated. Morton’s neuroma Referral Criteria Primary care • Advice re footwear (avoid heels and tight fitting shoes) • Analgesia & NSAIDs as appropriate • Refer to podiatry or physiotherapy • USS to establish size of neuroma and confirm diagnosis • Injection of steroid into the affected interspace or MTP joint(s) by appropriately trained GP/Podiatrist/Physiotherapist - palpate for painful area Secondary care • Failure of conservative treatment • Morton’s neuroma not responded to steroid injection • USS shows neuroma greater than 8 mm Morton’s Neuroma Patient Information Leaflet– Morton’s Neuroma Injection Advice Patient Primary Care Secondary Care Return to Ankle and Foot Pain Information Return to home page Achilles Tendinopathy/Posterior Heel Pain Signs and Symptoms • Pump bumps Prominent posterior aspect of calcaneum • • • Achilles Tendinosis Tenderness/swelling proximal to insertion of tendon to posterior calcaneum Pain on activity, easing during activity or with rest May be related to change of activity, footwear or orthotics Achilles Tendinosis/Posterior Heel Pain Referral Criteria Primary care • Simple padding and foot wear advice (Avoid low heeled footwear. Avoid boots or sports shoes which may impinge on the painful area during activity ) • Analgesia & NSAIDs as appropriate • Stretching programme • Off the shelf heel raises/ inshoe orthoses (From Boots/Allardyce/PhysioMed) • Refer podiatry or physiotherapy Mainstay of treatment is conservative • USS to determine tendinosis stage if considering steroid injection • Injection (should not be offered without USS to determine tendon state) NB: Steroid to be used under caution and no more than 2-3 Secondary care • Usually not indicated. Surgery rarely indicated. Achilles Tendinosis/Posterior Heel Pain Patient Information leaflet– Achilles tendinosis Patient Primary Care Secondary Care Injection Advice Return to Ankle and Foot Pain Information Return to home page Injection Advice Hallux Rigidus/Valgus Hallux Rigidus / Hallux Valgus • • • • • • • • NB: Physiotherapists must comply with PGD Patient lies with foot supported Identify joint line and distract toe Insert needle perpendicularly avoiding extensor tendons Up to 3 injections Up to 40mg Kenalog/2ml Lidocaine into painful area. Blue/orange needle Delivered as bolus Aftercare advice: avoid excessive WB 1-2 weeks Return to Ankle and Foot Pain Information Return to Injection Advice Return to home page Injection Advice Plantar Fasciitis Plantar Fasciitis • Patient lies prone with foot in dorsiflexion • Identity tender area on heel • Clean area with sterets/chloroprep • Insert needle perpendicularly into medial sole distal to heel pad. Advance at 45° toward medial tubercle on the calcaneus until touching bone • Up to 3 injections • Up to 40 mg Kenalog 2ml Lidocaine • Green needle • Peppering technique into fascia at medial bony origin • Aftercare advice: relative rest 2 weeks, then fascial stretching exercises • Address causative factors including weight loss if appropriate NB: Physiotherapists must comply with PGD Return to Ankle and Foot Pain Information Return to Injection Advice Return to home page Injection Advice Achilles Tendinopathy Achilles Tendinopathy NB: local agreement- some health boards do not inject Achilles tendinopathy NB steroid to be used under caution • NB Must USS first!!!! To determine tendon state • Patient lies prone with foot in dorsiflexion over end of bed. • Identify area of tenderness • Bend needle slightly using needle sheath • Clean area with sterets/chloroprep • Insert needle on medial side, angle parallel to tendon, deposit half solution while withdrawing needle • Change needle • Repeat procedure on lateral side • • • • • Up to 20 mg Kenalog, 1.5 ml Lidocaine each side of tendon Green needle Deliver as Bolus No resistance should be felt - DO NOT inject into body of tendon Aftercare advice: Absolute avoidance of overuse 10-14 days (WB tendon, predisposed to rupture) NB: Physiotherapists must comply with PGD Return to Ankle and Foot Pain Information Return to Injection Advice Return to home page Injection Advice Morton’s Neuroma Morton’s Neuroma Technique • Patient lies with knees bent and foot supported • Identify painful area • Clean area with sterets/chloroprep • Insert needle 45° angle • Up to 2 injections • • • • Up to 40mg Kenalog/4ml Lidocaine into painful area. Blue/Green needle Delivered as bolus Aftercare advice: relative rest 1-2 weeks • NB: Physiotherapists must comply with PGD Return to Ankle and Foot Pain Information Return to Injection Advice Return to home page General Injection Advice Elbow Tennis Elbow Golfer’s Elbow Shoulder Glenohumeral joint AC joint Subacromial bursa Hip Trochanteric Bursa Tendinopathies Hand De Quervains Trigger finger OA 1ST CMC joint Foot Hallux problems Morton's Neuroma Plantar Fasciitis Achilles Tendinosis Injection Handout March 2012 Knee Knee Joint Injection Patient Information Leaflet Ref: Kesson, Atkins and Davies,2003: Musculoskeletal Injection Skills. Butterworth Heinmann Injection Techniques in Orthopaedic Medicine, Saunders and Longworth. Churchill Livingstone 2006 Please note: these are guidelines for GPs. AHPs must comply with PGD Return to home page Patient Information Leaflets Shoulder Elbow Hand Hip Knee Ankle/Foot Cervical Spine Lumbar Spine Return to home page Shoulder • • • • • • NHS Inform: General advice acute pain PRICE Guidelines Impingement Adhesive Capsulitis Rotator Cuff Tears Instability/Recurrent Dislocation Return to home page Return to Patient Information Leaflets Return to Shoulder Pain Information Elbow • • • • • • NHS Inform: General advice acute pain PRICE Guidelines NHS Inform Elbow (PhysioTools) Tennis Elbow Golfers Elbow General Elbow Stiffness Return to home page Return to Patient Information Leaflets Return to Elbow Pain Information Hand • NHS Inform: Acute Wrist/Hand/Finger Pain Advice • PRICE Guidelines • Trigger Finger • De Quervain's • Dupuytren's • Ganglia • OA CMC joint • Carpal Tunnel Return to home page • Cubital Tunnel Return to Patient Information Leaflets Return to Hand Pain Information Hip • • • • • • NHS Inform: Acute Hip Pain Advice NHS Inform: Acute Thigh Problem Advice PRICE Guidelines Trochanteric Bursitis OA Hip Tendonopathy Return to home page Return to Patient Information Leaflets Return to Hip Pain Information Knee • • • • • • • • NHS Inform: Acute Knee Pain Advice NHS Inform: Acute Calf Pain Advice PRICE Guidelines Anterior Knee Pain OA Knee Meniscal problems Ligament Sprains/Strains Bursitis Return to home page Return to Patient Information Leaflets Return to Knee Pain Information Ankle/Foot • • • • • • • • • • NHS Inform: Acute Ankle Pain Advice NHS Inform: Acute Foot Pain Advice PRICE Guidelines Ankle Ligament Sprain Metatarsalgia Morton’s Neuroma Achilles tendinosis Hallux Valgus Hallux Rigidus Plantar Fasciitis Return to home page Return to Patient Information Leaflets Return to Ankle/Foot Pain Guidelines Cervical Spine • NHS Inform: Acute Neck Pain advice • NHS Inform: Whiplash • Hints and Tips to Help you Manage your Neck (NHS Tayside) • NHS Inform Neck (PhysioTools) • NHS Inform Neck (Video Physio) Return to home page Return to Patient Information Leaflets Return to Neck Pain Information Lumbar Spine • NHS Inform Back in Control • NHS Inform Back Problems • Hints and Tips to Help you Manage your Back (NHS Tayside) Return to home page Return to Patient Information Leaflets Return to LBP Pathway Glossary/Description tests • • • • • • Lhermitte’s sign: suggests a lesion of the dorsal columns of the cervical cord or MS. Neck flexion produces sudden general electric shock feelings down arms/spine/legs. Return to red flags LBP or neck pain Hoffman's sign: indicates presence upper motor neuron lesion from spinal cord compression. Flexion and sudden release of the terminal phalanx of the middle finger results in reflex flexion of the thumb and index (Possibly all digits) Return to red flags LBP or neck pain - positioning the neck in extension (sometimes flexion) may worsen reflex Babinski reflex: can indicate upper motor neuron lesion. Stroke lateral side of sole of foot from heel up to base 5th metatarsal, then across metatarsal heads firmly. Positive if great toe extends and other toes fan out. Return to red flags LBP or neck pain Tinel’s test: detects irritated nerves. Tap over nerve (Positive if produces tingling/pain) Return to CTS or Cubital Tunnel Phalen’s test: Patient pushes the dorsal surfaces of both hands together for 30–60 seconds (Positive if produces tingling/pain). Return to CTS Finklestein’s test: indicates De Quervain’s. Wrap patient’s fingers around thumb then pull wrist into ulnar deviation. Positive if produces pain Return to De Quervain’s Return to home page Glossary/Description tests • Osmond Clark test: apply an inferior glide to the patella while the patient actively contracts quads. Pain could indicate patellofemoral joint dysfunction • Anterior drawer test: used to assess ACL laxity. Patient lies supine with the hip flexed to 45° and knee to 90°. The examiner sits on the plinth at patient’s foot to prevent foot slipping. Grasp the tibia just below knee joint line. The thumbs are placed in the ‘eyes of the knee’ on either side of the patellar tendon. The index fingers should palpate hamstring tendons to ensure that they are relaxed. The tibia is then drawn forward anteriorly. An ACL-deficient knee will demonstrate increased forward translation of the tibia at the conclusion of the movement • Lachman’s test: used to assess ACL laxity. Flex knee to 30°, one hand above joint line, preventing forward movement of femur, one hand behind knee. Examiner pulls tibia assess the amount of anterior motion of the tibia in comparison to the femur. An ACLdeficient knee will demonstrate increased forward translation of the tibia at end of movement. • Ober’s manoeuvre: patient lies on side with hips and knees flexed. The upper leg is passively extended then lowered to the plinth. Lateral hip pain or considerable tightness may indicate iliotibial band syndrome. • Thomson test: patient should lie face-down, feet extended farther than end of the bed. The examiner squeezes the calf muscle. in normal patient this should cause the toes to point downward as the Achilles pulls the foot. In a patient with a ruptured Achilles tendon, the foot will not move. That is a positive Thompson test. Return to home page Glossary/Description Meniscal tests • McMurray’s test: used to evaluate for meniscal injury. The patient is supine, and the knee flexed fully. One hand holds ankle, other hand holds knee, with thumb on the lateral joint line and index finger on the medial joint line to palpate crepitus/click. Positive if ‘pop’ or ‘snap’ felt at the joint line – – Medial meniscus assessment: Apply valgus stress to flexed knee. Externally rotate leg (toes point outward) Slowly extend the knee while still in valgus. If pain or a "click" is felt, this constitutes a "positive McMurray test" for a tear in the medial meniscus. Lateral meniscus: Repeat above with varus stress and internal rotation • Steinman's test: used to evaluate for meniscal injury. Patient sits on the edge of the plinth, with knee hanging at 90° flexion, or the patient is supine with the knee at 90° flexion. Rotate tibia laterally then medially. Test is positive if lateral pain is elicited on medial rotation and medial pain is elicited on lateral rotation. Repeat test in various degrees of knee flexion. • Thessaly test: used to evaluate for meniscal injury. Patient stands flatfooted on the floor. Support the patient by holding outstretched hands. The patient rotates knee and body, internally and externally, three times, keeping the knee in slight (5°) flexion. Repeat with the knee flexed to 20°. Return to home page