Blood Cells - Dr Magrann

BLOOD
Blood is not an epithelial tissue, and it’s not loose or dense connective tissue; it’s classified as a “special connective tissue”. You have about 5 liters of blood, but that is only half of the body fluid. The other half includes fluid around each cell, and joint fluids, etc.
PLASMA
EXTRACELLULAR FLUID
↑
↓
SYNOVIAL FLUIDS, ETC
Blood consists of the following:
A.
Plasma
B.
Red blood cells
C.
White blood cells
D.
Platelets
Plasma is what the blood cells float around in. If you spin a blood sample in a test tube, the red blood cells sink to the bottom, and you’ll see the yellow plasma on top. Some people who need blood just need the packed RBCs, others need the plasma, and some need whole blood, which is both plasma and RBCs. The plasma also carries around the platelets and some white blood cells.
PLASMA CONTENTS
1.
Water (90%)
2.
Dissolved substances (10%) a.
Proteins i.
Albumin (egg white). Most common protein in blood (homeostasis) ii.
Antibodies iii.
Clotting factors called fibrinogen and fibrin. iv.
Lipoproteins (move fats through blood: HDL, LDL) b.
Nutrients i.
Glucose (main energy source) ii.
Amino Acids (builds proteins) c.
Wastes (urea) d.
Gases (O2, CO2, Nitrogen) e.
Electrolytes = ions (Na + , K + , Cl , Ca ++ )
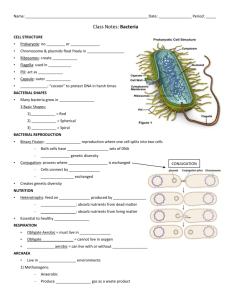
BLOOD CELLS
1
1.
ERYTHROCYTES (Red blood cells): These are among the smallest cells in the body. There are about 5 million of them in each of us. Their structure is simple; like a doughnut with the hole not fully cut out. a.
They have no nucleus b.
Filled with hemoglobin (Hgb), which carries O2 throughout the body.
Oxygenated Hgb is bright red, deoxy Hgb is a deeper red. c.
Average life span is 120 days. Old ones are destroyed in the spleen and liver, and Hgb is recycled. Every day, about 100 billion of these cells are destroyed, and 100 billion are made: where? Red marrow.
DISORDERS OF RBCs
POLYCYTHEMIA is too many red blood cells; can cause blood clots. Need to donate blood frequently.
ANEMIA: Anemia can be caused by many things:
– Too few RBC’s
–
Iron deficiency
–
Hemorrhagic anemia (person lost blood)
–
Hemolytic anemia (immune disorder, infection, blood transfusion)
G6PD deficiency
–
Hemoglobin abnormalities
Pernicious anemia (lack of vitamin B12 or intrinsic factor)
Thalassemia
Sickle cell disease
Megaloblastic anemia (pernicious anemia)
Hereditary spherocytosis
ANEMIA: Any condition of RED BLOOD CELLS in which the blood’s capacity for carrying oxygen is diminished.
HYPOXIA is lack of oxygen to tissues.
It can be caused from:
Ischemia (reduced blood flow to a tissue)
Malfunctioning hemoglobin
Increasing altitude
Characteristic sign of anemia: see reticulocytes in the blood (immature red blood cells).
Remnants of the nucleus are still in the cell.
DETAILS ABOUT SOME TYPES OF ANEMIA
Hemolytic anemia (immune disorder, infection, blood transfusion)
Hemolysis means rupture of RBC’s. Hemolytic anemia can be hereditary (born with the genes that cause the disease) or acquired. Hereditary factors include immune disorders and G6PD deficiency. Acquired causes include infections (malaria), and receiving the wrong blood type in a transfusion.
2
G6PD deficiency (hereditary, X-linked; almost all are males)
G6PDH is an enzyme which is important for RBC metabolism. G6PD is the most common human enzyme defect. A person with this would have a hard time maintaining iron in a reduced state, and they develop hereditary (NOT acquired) hemolytic anemia in response to a number of causes, most commonly infection or exposure to certain medications, chemicals, or ingestion of fava beans.
HEMOGLOBINOPATHIES (HEMOGLOBIN ABNORMALITIES)
Pernicious anemia (Megaloblastic anemia)
Caused by lack of vitamin B12 or intrinsic factor
When a person has gastric bypass surgery, the stomach is no longer able to produce intrinsic factor, which is needed to absorb vitamin B12, which is needed to make hemoglobin in RBC’s.
Without this vitamin, the blood cells are fewer and much larger than normal
(megaloblastic).
The surgery patient must take vitamin B12 shots or sublingual supplements for the rest of their life.
Thalassemia
A hereditary form of anemia where the RBCs have abnormal hemoglobin that deforms the cells into many types of unusual shapes, including spherocytes (small and round), target cells (looks like a target) and tear drops.
Sickle cell disease
A hereditary mutation resulting in one valine amino acid substituted for glutamic acid.
Present in African Americans more than in other groups, and is always characterized by sickled erythrocytes.
The sickle shape helps prevent malaria infections, but it also causes blood clots.
Hereditary spherocytosis
The red blood cells shrink over time due to problems with the red blood cell membrane.
Many of the RBC’s look small and round.
BLOOD TESTS FOR RBCs
RBC, Hgb, Hct
Red blood cell (RBC) count is a count of the actual number of red blood cells per volume of blood. Both increases and decreases can point to abnormal conditions.
Hemoglobin (Hgb) measures the amount of oxygen-carrying protein in the blood.
Hematocrit (Hct) measures the percentage of red blood cells in a given volume of whole blood.
3
HEMATOCRIT
A quick screening test for anemia is the hematocrit.
A drop of blood is drawn up a small glass capillary tube and the tube is centrifuged to pack the red blood cells at the bottom with the plasma on top.
Hematocrit measures the percentage of blood volume that consists of erythrocytes.
The hematocrit is the ratio of packed red blood cells to total blood volume.
Normal is about 45% (46% for men and 38% for women.)
Mean Corpuscular Volume
Mean corpuscular volume (MCV) is a measurement of the average size of your
RBCs.
The MCV is elevated when your RBCs are larger than normal (macrocytic), for example in anemia caused by vitamin B12 deficiency.
When the MCV is decreased, your RBCs are smaller than normal (microcytic) as is seen in iron deficiency anemia or thalassemias.
Mean Corpuscular Hemoglobin
Mean corpuscular hemoglobin (MCH) is a calculation of the average amount of oxygen-carrying hemoglobin inside a red blood cell.
Macrocytic RBCs are large so tend to have a higher MCH, while microcytic red cells would have a lower value.
Mean Corpuscular Hemoglobin Concentration
Mean corpuscular hemoglobin concentration (MCHC) is a calculation of the average concentration of hemoglobin inside a red cell.
Decreased MCHC values (hypochromia) are seen in conditions where the hemoglobin is abnormally diluted inside the red cells, such as in iron deficiency anemia and in thalassemia.
Increased MCHC values (hyperchromia) are seen in conditions where the hemoglobin is abnormally concentrated inside the red cells, such as in burn patients and hereditary spherocytosis, a relatively rare congenital disorder.
Red Cell Distribution Width
Red cell distribution width (RDW) is a calculation of the variation in the size of your RBCs.
Having RBC’s with various shapes is called aniscocytosis.
Having RBC’s with various shapes is called poikilocytosis.
In some anemias, such as pernicious anemia, anisocytosis and poikilocytosis causes an increase in the RDW.
4
BLOOD TYPING: The ABO SYSTEM
Blood typing is the technique for determining which specific protein type is present on
RBCs.
Only certain types of blood transfusions are safe because the outer membranes of the red blood cells carry certain types of proteins that another person’s body will think is a foreign body and reject it.
These proteins are called antigens (something that causes an allergic reaction). There are two types of blood antigens: Type A and Type B.
A person with Type A antigens on their blood cells have Type A blood.
A person with Type B antigens have Type B blood.
A person with both types has type AB blood.
A person with neither antigen has type O blood.
If a person with type A blood gets a transfusion of type B antigens (from Type B or Type
AB, the donated blood will clump in masses (coagulation), and the person will die.
The same is true for a type B person getting type A or AB blood.
Type O negative blood is called the universal donor, because there are no antigens, so that blood can be donated to anyone. Type AB positive blood is considered the universal acceptor, because they can use any other type of blood. This blood type is fairly rare.
The rarest blood type is AB negative.
RH FACTOR
There is another term that follows the blood type. The term is “positive” or “negative”.
This refers to the presence of another type of protein, called the Rh factor. A person with type B blood and has the Rh factor is called B-positive.
A person with type B blood and no Rh factor is called B-negative.
5
The reason this is so important is that if an Rh- mother has an Rh+ fetus in her womb
(from an Rh+ father), her antibodies will attack the red blood cells of the fetus because her body detects the Rh protein on the baby’s red blood cells and thinks they are foreign objects. This is called Hemolytic Disease of the Newborn (HDN).
This can be prevented if the doctor knows the mother is Rh- and the father is Rh+, because that means the baby has a 50% chance of being Rh+ like the father.
Therefore, anytime a mother is Rh-, even if the mother says the father is Rh-, you can’t be sure who the father is, so they will proceed as though the baby may be Rh +.
They will give her an injection of a medicine (rhogam) that will prevent her immune system from attacking the baby.
Rhogam
Rhogam is given at 18 weeks into the pregnancy and again within 72 hours after giving birth.
It is usually given within 2 hours after giving birth since you can’t trust the patient to return after they leave the hospital.
The first baby is not at risk; during the first birth, the placenta tears away and that’s when the baby’s blood cells get into the mother’s bloodstream.
She then forms antibodies against the Rh factor, which are ready to attack the second fetus.
The baby does not make the Rh factor until about 18 weeks into the pregnancy.
Kell Proteins
The Kell protein is another antigen on some people’s RBC’s, similar to the Rh factor. People either have big K or little k proteins. Most people have little kk. If one parent has big K (either Kk or KK), the child can get Hemolytic Disease of the Newborn.
This is probably the disease that was in the genes of Henry VIII (probably had
Kk), which caused most of his children to become weak and die in infancy. He could only safely have children with those women who were either Kk or KK
(about 9% of the population).
6
Microbiology
To understand the function of white blood cells, you will need to learn some general concepts and terminology from Microbiology:
–
Pathogen
–
General size of bacteria and viruses
– Antigen
Pathogen “Path” = disease “ogen” = generating
A pathogen is something that causes disease.
A biological pathogen is a bacterium, virus, fungi, yeast, protozoa, worms, etc.
A non-biological pathogen can be a toxic chemical, asbestos, etc.
Usually, the term “pathogen” refers to a biological pathogen.
Sizes of Pathogens
Bacteria are so small that hundreds of them can fit inside one white blood cell. However, bacteria usually do not invade body cells. They live between the cells of the body, using up nutrients in the area, and they cause harm by secreting toxins. Viruses are so small that thousands of them can fit inside the NUCLEUS of one white blood cell. They always try to invade body cells because they need a piece of our DNA or RNA in order to replicate. When a body cell has been invaded by a virus, the entire cell must be killed by a white blood cell.
Antigen
An antigen is anything that causes an immune response, which isn't necessarily a biological pathogen (disease-causing organism).
A non-biological antigen can be pollen, dust, grass, or anything that a person is allergic to.
Pollen can be an antigen to a person with allergies, but it is not an antigen to a person without allergies, because no immune response was launched.
LEUKOCYTES (White blood cells): There are different kinds; all fight infection.
1) BASOPHILS: Few in body. Their blue granules are filled with histamines, which help fight infection by vasodilation, increasing the number of WBCs to the infection site.
Antihistamines interfere with the function of basophils. When a basophile leaves the circulation to enter the tissues, it becomes a MAST CELL .
2) EOSINOPHILS: Function to fight allergies and parasitic infections. During these conditions, their numbers increase.
3) NEUTROPHILS: The most abundant type of WBC. They are the first to respond to infection. They phagocytize (eat) bacteria and also destroy bacterial toxins in body fluids. Nucleus – has two to six lobes
Neutrophils are the white blood cells that contribute to immunity mainly by engulfing BACTERIA and foreign bodies (thorns, dirt, etc) in a process called phagocytosis.
They release the contents of their lysosomes onto the invader, dissolving it.
When a bacterium has a capsule, it makes it hard to phagocytize, so the neutrophil requires opsonization by antibodies.
7
Some bacteria have evolved a slippery capsule around them as a defense against phagocytosis. The neutrophil cannot engulf this type of bacteria. Neither can a macrophage.
When an antibody attaches to this type of bacteria, the neutrophil can now grab onto the antibody like a handle, enabling it to phagocytize the bacteria.
This process of facilitation of phagocytosis is called OPSONIZATION .
When the invader has the antibody attached to it, it is called an ANTIGEN-
ANTIBODY COMPLEX.
If a bacterium does not have a capsule, the neutrophil can destroy it without opsonization. The antibody can also destroy the bacterium by itself by popping the cell membrane.
But when a capsule is present, the neutrophil and antibody work best together.
Neutrophils are also the ones that primarily destroy the dissolved toxins that bacteria secrete into body fluids.
4) MONOCYTES: Like neutrophils, they phagocytize (eat) bacteria, old cells, and foreign bodies.
They have more types of lysosome enzymes than neutrophils so they are better at killing difficult pathogens.
They also use antibodies for opsonization.
When they leave the bloodstream and enter the tissues, they are called
MACROPHAGES.
What’s the Difference between Neutrophils and Monocytes/Macrophages?
There are 10x more neutrophils in the bloodstream than monocytes/Macrophages. Consider neutrophils to be the most numerous white blood cell.
However, there are more macrophages in the tissues of the body. They are everywhere!
Neutrophils live only a few days. Monocytes/Macrophages live a few months.
Lymphocytes live for years.
Monocytes/Macrophages are larger and slower than neutrophils, but they can phagocytize larger organisms and more of them.
Neutrophils usually just phagocytize bacteria until they die. Macrophages phagocytize and then take pieces of the dead bacteria and present them to lymphocytes so a larger immune response can occur.
There are two types of phagocytes: Neutrophils and macrophages.
Neutrophils and macrophages both mainly function by phagocytizing bacteria (not viruses).
Neutrophils and macrophages eat bacteria more easily after an antibody attaches to the bacteria. This is called an antigen-antibody complex. The antibody enables the neutrophil or macrophage to grab onto the bacteria more easily.
Lymphocytes are mostly needed to kill off body cells infected by viruses.
Neutrophils just phagocytize bacteria and secrete chemicals to recruit more white blood cells to the site.
Unlike neutrophils, macrophages have surface receptors ; these "recognize" the surface of the pathogen’s cell membrane.
8
Macrophages phagocytize the bacteria, pop their lysosomes onto it, and dissolve it, except for some pieces of the bacteria’s cell membrane.
The macrophage places these pieces of bacteria on its own cell membrane, and finds a lymphocyte to present it to.
Macrophages present these pieces to T cell lymphocytes and to B cells lymphocytes.
The lymphocyte feels the shape of the bacteria pieces on top of the macrophage,
(this is called “antigen presentation”) and the lymphocyte can then launch an attack on the rest of the bacteria still alive in the body.
In this way, the macrophage recruits even more lymphocytes to join the war.
So, what is a lymphocyte?
5) LYMPHOCYTES : Effective in fighting infectious organisms like body cells infected with viruses They act against a specific foreign molecule (antigen)
Two main classes of lymphocyte
–
B cells – Originate in the bone marrow, mature into plasma cells. A mature plasma cell fights infection by producing antibodies
–
T cells – Originate in the thymus gland. They attack foreign cells directly
(including organ transplants!)
B CELLS : – mature into plasma cells
PLASMA CELLS secrete antibodies; the antibodies are what kill the attacking cell. Antibodies attack in two ways:
–
They attach to bacteria and pop the cell membrane
–
They attach to encapulated bacteria to help neutrophils phagocytize them.
Mononucleosis : Epstein Barr virus attacks B lymphocytes. It is characterized by inflammation of lymph vessels (lymphangitis). Lymphangitis : lymph vessel inflammation; usually from infection. Infected lymphocytes have a characteristic scalloped edge where they touch RBC’s
T CELLS
1.
C oordinate the immune response by recruiting other white blood cells
2.They can directly destroy bacteria by popping their cell membrane.
3.They can also destroy body cells infected with viruses.
4.
T cells attack foreign cells directly by popping the cell membrane.
5.They do not need to phagocytize the invading cell. They do not need the assistance of antibodies.
6.T-cells can therefore kill a body cell that has become infected with viruses.
7.T cells are the cells that attack organ transplants!
8.Immunosuppression drugs are designed to inhibit the action of T cells.
9.T cells are attacked by the HIV (AIDS) virus.
10.The thymus gland secrets certain hormones which can cause T cells to become immunocompetent (makes the cells mature and start to work)
9
There are several types of T cells. The main types are
Cytotoxic (Killer) T cells
– Go out and directly kill bacteria or infected host cells
Helper T cells
– Release chemicals called “cytokines” to stimulate the B cells to produce antibodies against the bacteria. Cytokines also call in more white blood cells of all types to join in the war.
Suppressor T cells
Stop the immune process when it is over, and also "tell" some B-Cells to "remember" how to destroy that specific pathogen. Those B-cells then become Memory B-Cells. They can react to the same pathogen faster, the next time it invades. Memory B-cells already have the proper antibodies stored up for that pathogen.
Summary
A pathogen somehow gets past the body's physical and chemical barriers and the inflammation response.
The pathogen is engulfed by a macrophage (or neutrophil).
The macrophage releases the contents of its lysosomes onto the bacterium and dissolves most of it. There are still some pieces of the bacterium’s cell membrane left. The macrophage then forces the surface proteins of the bacterium (antigens) to it's own cell surface.
Helper T-Cells touch these surface antigens, make a copy of their shape, and present them to B-cells to make antibodies against them.
These Helper T-Cells begin to multiply and have two main roles.
The first is to activate B-Cells and "tell" them how to neutralize the pathogen by presenting the pieces of the bacterium cell membrane so the B-cells can make antibodies.
The B-Cells (now called Plasma cells because they have been activated) begin to multiply and produce the antibodies to neutralize this specific pathogen.
The second role of Helper T-Cells is to activate the Killer T-Cells.
Killer T-Cells can either destroy the pathogen itself (bacteria), or destroy the entire body cell which is infected (viruses).
When the immune response is over, Suppressor T-Cells stop the process and also
"tell" some B-Cells to "remember" how to destroy that specific pathogen. Those
B-cells now become Memory B-Cells.
DISORDERS OF WBCs
LEUKEMIA : Cancer of the blood is called leukemia. It actually only involves the white blood cells. Something goes wrong in one stem cell, and it starts making huge amounts of clones of itself which don’t work right and not enough normal white blood cells are made. Therefore, the body cannot fight infection. It’s better to send a young cell with no weapons to the war than to send nothing at all!
10
There are many types of leukemias.
Think of Leukemia as too few mature white blood cells.
–
Classified as lymphoblastic (too many immature lymphocytes) or
– myeloblastic (too many immature neutrophils)
People with severe leukemia may need a bone marrow transplant.
First, all of their WBC’s have to be killed off with a medicine because they are mostly malfunctioning anyway.
A donor has a small cylinder of bone removed from their hip. This is ground up and given by i.v. to the recipient.
The new WBC’s may kill the patient or it may save their life. It is done as a last resort.
WBC Count
White blood cell (WBC) count is a count of the actual number of white blood cells per volume of blood. Both increases and decreases can be significant.
White blood cell differential looks at the types of white blood cells present. There are five different types of white blood cells, each with its own function in protecting us from infection. The differential classifies a person's white blood cells into each type: neutrophils (also known as segs, PMNs, granulocytes, grans), lymphocytes, monocytes, eosinophils, and basophils.
Terms
Excess neutrophils: neutrophilia
Few neutrophils: neutropenia
Excess platelets: thrombocytophilia
Few platelets: thrombocytopenia
Antibodies
Antibodies (also known as immunoglobulins, abbreviated Ig) are proteins made by plasma cells.
They are used to identify and neutralize foreign objects, such as bacteria and viruses.
They are typically made of basic structural units—each with two large heavy chains and two small light chains—to form a unit shaped like the letter “Y”
The tips of the “Y” have receptors that are specific for a particular antigen.
The stem of the “Y” can be grasped by a phagocyte.
The small region at the tip of the protein is extremely variable, allowing millions of antibodies with slightly different tip structures, or antigen binding sites, to exist.
This region is known as the hypervariable region. Each of these variants can bind to a different target, known as an antigen.
This huge diversity of antibodies allows the immune system to recognize an equally wide diversity of antigens.
11
Some of these “Y” shaped units exist by themselves (monomers)
Some are in pairs (dimers)
Some are in a cluster of five (pentamers)
There are five different antibody types , which perform different roles, and help direct the appropriate immune response for each different type of foreign object they encounter.
IMMUNITY : B Cells that have matured into plasma cells which have made antibodies are now called Memory lymphocytes, after their first war.
Most people are sick more often as children than as adults in their 20s through 30s because we build up many varieties of MEMORY LYMPHOCYTES during childhood, providing immunity from more and more antigens during adulthood.
Myasthenia gravis
Myasthenia gravis (MG): autoimmune disease where antibodies destroy or block receptors for acetylcholine, a neurotransmitter.
Causes muscle paralysis.
First attacks small muscles especially those that keep eyes open; will spread to diaphragm
death. To stave off effects, do thymectomy.
12
PLATELETS (very small compared to all other blood cells). These are pieces of another cell found in the red marrow called a MEGAKARYOCYTE.
Pieces break off of a megakaryocte and are known as platelets. When a platelet encounters a broken blood vessel it releases a substance that clots blood. Platelets are responsible for clot formation.
Platelets need certain proteins in the plasma called CLOTTING FACTORS in order for them to become activated and form a clot.
Two main clotting factors are called FIBRIN and FIBRINOGEN .
VITAMIN K
Found in green, leafy vegetables
Needed for blood clotting factors.
Some types of rat poisons work by eliminating the blood clotting ability.
In case of accidental ingestion of rat poison, a child needs an I.V. of vitamin K.
It works for accidental poisoning in dogs, too!
Aspirin
One baby aspirin a day can help prevent blood clots.
It blocks the ability of an enzyme called COX (cyclo-oxidase) to cleave arachidonic acid into a molecule called a prostaglandin.
Prostaglandins are needed for inflammatory reactions and for making clotting factors.
COX inhibitors, such as aspirin, block pain from inflammation, but they also
INCREASE blood clotting time.
DISORDERS OF PLATELETS
Thrombocytopenia: too few platelets, and blood doesn’t clot properly (hemophilia).
HEMOPHILIA is a hereditary disease of males, where they are unable to clot properly because they are missing some clotting factors.
When they get even a slight bump or bruise they have to have an intravenous infusion of clotting factors or they will bleed to death.
A thrombus is a blood clot in a vessel.
An embolism is a thrombus that broke away and travels in the blood stream. It usually lodges in a smaller blood vessel and blocks circulation distal to that point.
Platelet Count and MPV
The platelet count is the number of platelets in a given volume of blood.
Both increases (thrombocytophilia) and decreases (thrombocytopenia) can point to abnormal conditions of excess bleeding or clotting.
Mean platelet volume (MPV) is a machine-calculated measurement of the average size of your platelets. New platelets are larger, and an increased MPV occurs when increased numbers of platelets are being produced.
13
Prothrombin Time (PT) and
Partial Thromboplastin Time (PTT)
The PTT test is used to investigate unexplained bleeding or clotting. It may be ordered along with a PT (Prothrombin Time) test to evaluate hemostasis (the process of clot formation). The PTT evaluates the coagulation factors XII, XI, IX,
VIII, X, V, II (prothrombin), and I (fibrinogen). A PT test evaluates the coagulation factors VII, X, V, II, and I (fibrinogen). By evaluating the results of the two tests together, a doctor can gain clues as to what bleeding or clotting disorder may be present.
These tests are used to monitor heparin anticoagulant therapy. Heparin is a drug that is given intravenously (IV) or by injection to prevent and to treat blood clots.
IV’s are also flushed with heparin to prevent clot formation. When it is administered for therapeutic purposes, it must be closely monitored. If too much is given, the treated person may bleed excessively; with too little, the treated person may continue to clot.
HOW TO READ A BLOOD TEST
Complete Blood Count (CBC)
The complete blood count or CBC test is used as a broad screening test to check for such disorders as anemia, infection, and many other diseases. It is actually a panel of tests that examines different parts of the blood and includes the following:
White blood cell (WBC) count
White blood cell differential
Red blood cell (RBC) count
Hemoglobin
Hematocrit
platelet count , PT, PTT
Mean corpuscular volume (MCV)
Mean corpuscular hemoglobin (MCH)
Mean corpuscular hemoglobin concentration (MCHC)
Red cell distribution width (RDW)
Life span, from longest-lived to shortest-lived: lymphocytes, erythrocytes, platelets, neutrophils.
Septicemia
Septicemia (aka bacteremia) is the condition when bacteria invade the body and circulate in the blood.
Bacteria can enter the bloodstream as a severe complication of infections (like pneumonia or meningitis), during surgery (especially when involving mucous
14
membranes such as the gastrointestinal tract), or due to catheters and other foreign bodies entering the arteries or veins (including intravenous drug abuse).
Bacteremia can have several consequences. The immune response to the bacteria can cause sepsis and septic shock, which has a relatively high mortality rate (kills
1 person in 5). Bacteria can also use the blood to spread to other parts of the body
(which is called hematogenous spread), causing infections away from the original site of infection. Examples include endocarditis or osteomyelitis.
Treatment is with antibiotics, and prevention with antibiotic prophylaxis can be given in situations where problems are to be expected.
HEMATOPOIESIS : The making of blood.
The plasma proteins are made in the liver.
The blood cells are made in the red marrow.
STEM CELLS IN THE RED MARROW
STEM CELLS : A cell that has not matured and differentiated yet.
An embryo has lots of stem cells which have not decided to become a nerve cell, muscle cell, liver cell, etc. Stem cells become the type of cell the body needs. The placenta of a newborn infant has many of these stem cells, too, but not as many as an embryo. That’s why people want to research stem cells on embryos; there are more stem cells there.
The first step for a stem cell is to DIFFERENTIATE , which is to decide what system of cells it will belong to. A stem cell that matures in the bone marrow will become a blood cell. Adults don’t have too many stem cells that are so immature that they have not yet decided what system of cells to belong to. Most of our stem cells have matured to the next step, which is that they have decided what system to evolve into. An adult has stem cells that will ONLY become blood, nerve tissue, organs, etc.
Blood Cell Formation
Hematopoiesis – process by which blood cells are formed
100 billion new blood cells formed each day
The plasma proteins are made in the liver.
The blood cells are made in the red marrow.
Bone Marrow as the Site of Hematopoiesis
Bone marrow – located within all bones
–
Red marrow – actively generates new blood cells
Contains immature erythrocytes
Remains in epiphyses, girdles, and axial skeleton
–
Yellow marrow – dormant
Contains many fat cells
Located in the long bones of adults
RED BONE MARROW
Most blood cells mature in the red bone marrow. When they are mature, they are released into the bloodstream. When they are old, they are destroyed in the spleen.
15
Cell Lines in Blood Cell Formation
All blood cells originate in bone marrow
All originate from one cell type – blood stem cell
–
Erythroblasts – give rise to red blood cells
–
Lymphoblasts – give rise to lymphocytes
–
Myeloblasts – give rise to all other white blood cells
1.
ERYTHROBLASTS , which mature into RETICULOCYTES , a RBC with bits of nucleus material,which later resolves to make more room for hgb. It is now called an ERYTHROCYTES . If the body makes too few erythrocytes it can lead to one form of ANEMIA.
2.
LYMPHOBLASTS give rise to lymphocytes
3.
MYELOBLASTS : These are the stem cells that mature into the specific leukocytes:
Neutrophil, macrophage, eosinophil, basophil, platelets. Leukemia is cancer of the stem cells. See all these different types of stem cells? That’s about how many types of leukemia there are.
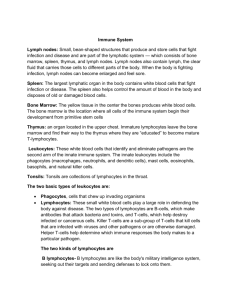
IMMUNE SYSTEM
INFLAMMATORY REACTION : When you get stuck by a thorn or inhale a cold virus, the body goes through a series of events called an inflammatory reaction.
Four outward signs:
1.
Redness
2.
Heat
3.
Swelling
4.
Pain
Redness is caused from the blood vessels dilating to allow more blood flow to the area.
Within the blood are platelets to clot the blood, proteins to repair the damage, and macrophages, which are white blood cells that eat up the foreign body, bacteria, or the dead cells.
Heat is caused because of the extra amount of warm blood flow to the area.
Swelling is caused from the plasma that leaks out of the swollen blood vessels.
Pain is caused from the pressure of the extra fluid pressing on nerves in the area.
ADAPTIVE IMMUNITY
Two types of Adaptive Immunity
– ACTIVE immunity
Naturally Acquired
Artificially Acquired
–
PASSIVE immunity
Naturally Acquired
Artificially Acquired
ACTIVE IMMUNITY
Naturally Acquired
– The body is naturally exposed to an infectious agent and launches an immune reaction
Artificially Acquired
– The person is injected with a weakened (attenuated) or killed organism, as found in a vaccination
16
Naturally acquired active immunity
This is when the body is exposed to an infectious agent and produces antibodies which specifically attack that infectious agent so the person never gets that disease again. The plasma cells secrete these antibodies which will continue to circulate sometimes for years, ready to attack that type of bacteria and cause them to pop like a balloon before the body can become sick.
–
You catch a cold and eventually get better. You can never get the same cold virus twice because you will have become immune to it. Your next cold is from a different virus. There are hundreds of thousands of cold viruses; that’s why there is no cure for the common cold.
–
Another example is when an unvaccinated child is exposed to the measles at school and gets the disease, but never gets the disease again.
However, there are some diseases that you don’t want to get, even once, such as polio, diphtheria, tetanus, and influenza, because the first exposure could kill or disable you.
For these diseases, we have vaccines which are made of those organisms which have been altered (attenuated) so that the body recognizes them as foreign, but they can’t cause disease. That way, if the person is exposed to the real organism later, the antibodies are already there to kill it off without the body getting sick.
Artificially acquired active immunity
–
An example is when a child is vaccinated against measles as a baby, so when he gets to school and is exposed to the disease, he doesn’t get sick.
PASSIVE IMMUNITY
Naturally Acquired
–
Example is the passing of antibodies from mother to infant in breast milk
Artificially Acquired
–
Example is when a person receives an infusion of antibodies from someone else.
ALLERGIES are from a hypersensitivity to substances such as pollen or animal hair that would not ordinarily cause a reaction. There are two types of allergic responses:
1.
Immediate allergic response occurs within seconds of contact with the thing causing the allergy. This is the case with anaphylactic allergies, where someone who is allergic to seafood or peanuts can actually die within minutes because the allergic reaction is so severe the throat swells shut and they can’t breathe . They need an injection immediately of something that will stop the reaction.
2.
Delayed allergic response is when the body’s first exposure to the substance will not cause a reaction, but all exposures afterward will trigger the response. An example is poison ivy. You won’t itch the first time you touch it.
AUTOIMMUNE DISEASE is a hereditary problem where the body thinks its own tissues are foreign bodies, and it constantly tries to kill off its own tissues.
17