Pain - POGOe
advertisement
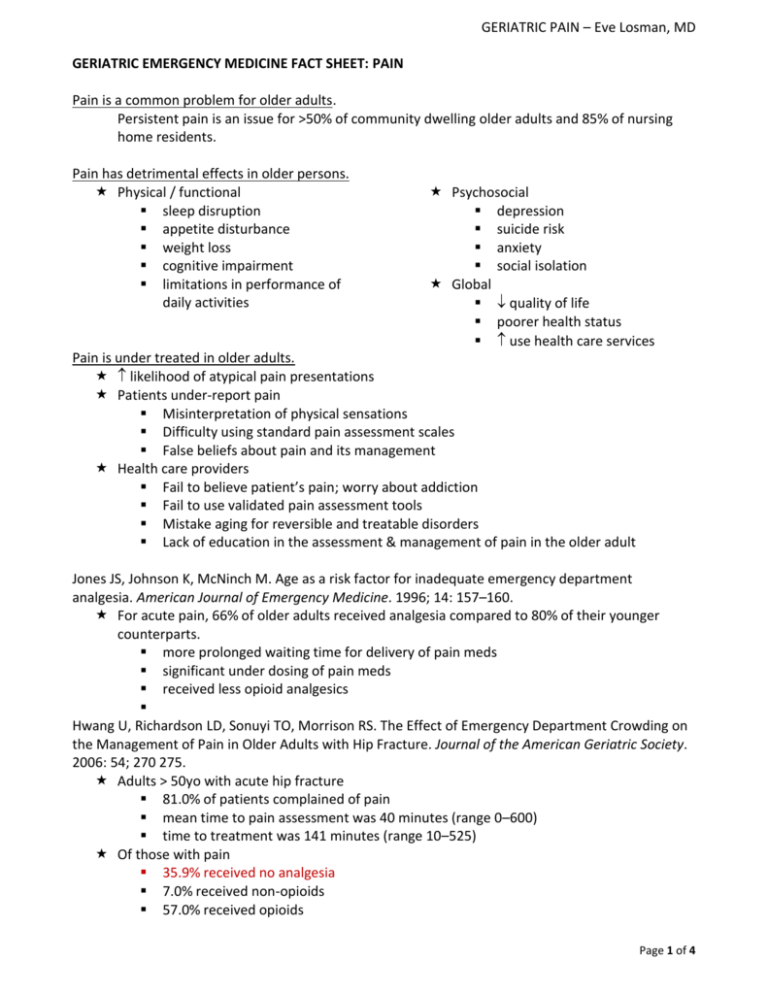
GERIATRIC PAIN – Eve Losman, MD GERIATRIC EMERGENCY MEDICINE FACT SHEET: PAIN Pain is a common problem for older adults. Persistent pain is an issue for >50% of community dwelling older adults and 85% of nursing home residents. Pain has detrimental effects in older persons. Physical / functional sleep disruption appetite disturbance weight loss cognitive impairment limitations in performance of daily activities Psychosocial depression suicide risk anxiety social isolation Global quality of life poorer health status use health care services Pain is under treated in older adults. likelihood of atypical pain presentations Patients under-report pain Misinterpretation of physical sensations Difficulty using standard pain assessment scales False beliefs about pain and its management Health care providers Fail to believe patient’s pain; worry about addiction Fail to use validated pain assessment tools Mistake aging for reversible and treatable disorders Lack of education in the assessment & management of pain in the older adult Jones JS, Johnson K, McNinch M. Age as a risk factor for inadequate emergency department analgesia. American Journal of Emergency Medicine. 1996; 14: 157–160. For acute pain, 66% of older adults received analgesia compared to 80% of their younger counterparts. more prolonged waiting time for delivery of pain meds significant under dosing of pain meds received less opioid analgesics Hwang U, Richardson LD, Sonuyi TO, Morrison RS. The Effect of Emergency Department Crowding on the Management of Pain in Older Adults with Hip Fracture. Journal of the American Geriatric Society. 2006: 54; 270 275. Adults > 50yo with acute hip fracture 81.0% of patients complained of pain mean time to pain assessment was 40 minutes (range 0–600) time to treatment was 141 minutes (range 10–525) Of those with pain 35.9% received no analgesia 7.0% received non-opioids 57.0% received opioids Page 1 of 4 GERIATRIC PAIN – Eve Losman, MD Percentage of ED pain-related visits by adults in which any analgesic or an opioid was administered by patient age in 5-year increments, NHAMCS 1999 to 2008. Platts-Mills TF, Esserman DA, Brown DL, Bortsov AV, Sloane PD, McLean SA. Older US Emergency Department Patients Are Less Likely to Receive Pain Medication Than Younger Patients: Results From a National Survey. Annals of Emergency Medicine, 2011, in press. Pain Assessment in the Older Adult: Nonspecific signs and symptoms indicating pain in the older adult Frowning, moaning, grimacing, fearful facial expressions, grinding of teeth Sighing, groaning, fearfulness, heavy breathing, withdrawal Fidgeting / restlessness / agitation Eating or sleeping poorly Mental status change / change in behavior Decreasing activity levels Depressed affect Resistance to certain movements during care Paucity of interaction or speech Loss of function & lack of adaptation skills Principles of pain management Always enquire about pain. Treat the underlying cause of the pain. Treat the pain meticulously. Treat the pain proportionately. Constantly reassess. Page 2 of 4 GERIATRIC PAIN – Eve Losman, MD http://consultgerirn.org/topics/pain/want_to_know_more http://consultgerirn.org/topics/pain/want_to_know_more Polypharmacy: In the U.S., older adults consume greater than 30% of all prescription drugs. ~90% of older adults are on at least one medication > 40% of older patients use more than 5 drugs weekly ~ 12% of older adults are using more than 10 medications Increased risk of adverse drug reactions due to these multiple medications, greater severity of illness, multiple co-morbidities, sarcopenia, and changes in hepatic and renal metabolism. Patient 65 years and older comprise over 25% of all ED adverse drug events (ADE) visits, and are 2.4 times more likely to sustain ADEs when compared to their younger counterparts Page 3 of 4 GERIATRIC PAIN – Eve Losman, MD From Ula Hwang, MD MPH – “GERIATRIC ANALGESIA” Optimal analgesic management for the geriatric patient requires the delicate balance of avoiding oligoanalgesia (inadequate analgesia) while taking into consideration aging-related changes with regards to medication metabolism, polypharmacy increased risk of adverse drug events, and drugs to avoid. First “do no harm”, initiating analgesia for mild pain with non-opioid analgesia (acetaminophen). For moderate to severe pain, progress to milder and then stronger opioids (hydrocodone, morphine, hydromorphone). Always start low and go slow with routine re-assessment of pain severity and titration of medications with a preference for shorter-acting drugs and lower doses. If using opioids, always remember to also use laxatives and stool softners to curtail the adverse effect of constipation. Analgesics NOT recommended and considered inappropriate (per Beers Criteria) Codeine Indomethacin (Indocin) Toradol (Ketorolac) Meperidine (Demerol) muscle-relaxants Pentazocine (Talwin) long-acting benzodizaepines Propoxyphene (Darvon) high-doses of short-acting benzodiazepines Bibliography / Resources: AGS Clinical Practice Guideline: Pharmacological Management of Persistent Pain in Older Persons. http://www.americangeriatrics.org/education/2009_Guideline.pdf Barkin RL, Barkin SJ, Barkin DS. Pharmacotheraputic Management of Pain with a Focus Directed at the Geriatric Patient. Rheumatic Disease Clinics of North America. 2007; 33: 1-31. Beers MH. Explicit criteria for determining potentially in appropriate medication use by the elderly. An update. Archives of Internal Medicine. 1997; 157: 1531-1536. Fick DM, Cooper JW, Wade WE, Waller JL, Maclean JR, Beers MH. Updating the Beers Criteria for Potentially Inappropriate Medication Use in Older Adults: Results of a US Consensus Panel of Experts. Archives of Internal Medicine. 2003; 163: 2716-2724. Hohl CM, Dankoff J, Colacone A, Afilalo M. Polypharmacy, adverse drug-related events, and potential adverse drug interactions in elderly patients presenting to an emergency department. Annals of Emergency Medicine. 2001;38(6):666-671. Hwang U, Richardson LD, Harris B. Morrison RS. The Quality of Emergency Department Pain Care for Older Adult Patients. Journal of the American Geriatrics Society. 2010; 58: 2122–2128. Hwang U, Richardson LD, Sonuyi TO, Morrison RS. The Effect of Emergency Department Crowding on the Management of Pain in Older Adults with Hip Fracture. Journal of the American Geriatric Society. 2006: 54; 270 275. Jones JS, Johnson K, McNinch M. Age as a risk factor for inadequate emergency department analgesia. American Journal of Emergency Medicine. 1996; 14:157–160. Platts-Mills TF, Esserman DA, Brown DL, Bortsov AV, Sloane PD, McLean SA. Older US Emergency Department Patients Are Less Likely to Receive Pain Medication Than Younger Patients: Results From a National Survey. Annals of Emergency Medicine, 2011, in press. Terrell KM, Heard K, Miller DK. Prescribing to older ED patients. The American Journal of Emergency Medicine. 2006;24(4):468-478. Page 4 of 4