NEP/1 (P) COMPARATIVE STUDY OF CHANGES IN LIPID
advertisement

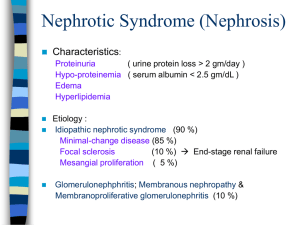
NEP/1 (P) COMPARATIVE STUDY OF CHANGES IN LIPID PROFILE IN INITIAL EPISODE AND IN RELAPSE CASES OF NEPHROTIC SYNDROME Prabhat Kumar, Kanai Lal Barik, Anindya Dasgupta Post Graduate Student, Department of Pediatric Medicine, Burdwan Medical College And Hospital, Burdwan Email: prabhatbmch@live.com Hyperlipidemia is a common findings in Nephrotic syndrome. There is increase in total Cholesterol, LDL cholesterol, VLDL cholesterol, TG and low or normal HDL cholesterol (1) .There are only few studies on derangement of serum lipid with nephrotic syndrome in Indian children. Hyperlipidemia is usually observed during the active phase of disease and disappears with resolution of proteinuria. But in relapsing cases, it may persist and may increase risk of atherosclerosis in later life (2). Hence serial monitoring of lipids is required to predict atherosclerosis risk in future . There are also only few studies on serial estimation of lipids in children with nephritic syndrome. Our study is an attempt to know derangement of serum lipids in Indian children with nephrotic syndrome and to study serial estimation of lipids to assess, when these levels return to normal. Review Of Literature: - Nephrotic syndrome is primarily a pediatric disorder, Incidence is 2 – 3 / 100,000 chidren per year ( 3 ). Majority of affected chidren have steroid sensitive minimal change disease. The characteristic features of nephritic syndrome are heavy proteinuria ( > 40 mg/m2/ hr ) , hypoalbuminemia ( <2.5 g/dl ), edema and hyperlipidemia. Cause of the increase permeability is not well understood. In minimal change disease T cell dysfunction may alter level of cytokines, leads to loss of negatively charged glycoproteins within glomerular capillary wall. Serum lipid levels are elevated for two reasons. Hypoalbuminemia stimulates generalized hepatic protein synthesis, including synthesis of lipoproteins. Lipid catabolism is decreased, as a result of reduced plasma levels of lipoprotein lipase, related to increased urinary losses of this enzyme. In children with the Nephrotic syndrome, there is an inverse relationship between the rate of urinary excretion of protein & the degree of hypoalbuminemia. The rate of albumin synthesis in nephrotic syndrome in a steady state is not decreased, it is either increased or normal. In general there is inverse correlation between conc. Of serum albumin and that of cholesterol. The level of TG is more variable and may even be normal in patients with mild hypoalbuminemia. The conc. Of VLDL chol & LDL chol are increased ( 4). HDL chol are usually normal or decreased (1) in child with nephrotic syndrome , although the ratio of HDL chol to Total chol may still be low.(5,6,7,8) Some children with lesions other than minimal change may have decreased HDL chol. Complications due to hyperlipidemia..risk of cardiovascular disease AIMS AND OBJECTIVES:- Lipoprotein play an important role in the transport of plasma lipids; Their elevation or alteration in various fractions may be responsible for hypercholesterolemia in nephrotic syndrome .There is increased total cholesterol, LDL cholesterol, VLDL cholesterol, and Triglycerides and normal or low HDL(4). However in Indian children the degree of hyperlipidemia is not as high as in western children. Our study is designed to study the derangement of serum lipids in nephritic syndrome, and to know whether any correlation exist between serum lipid & serum albumin. Specific Objectives: - To analyse pattern of change in the serum lipid profile in nephrotic syndrome in Indian children. To evaluate whether any correlation exists between serum lipid level & serum albumin in nephrotic syndrome. To assess when the serum lipids returns to normal. Materials And Methods:- A)Study Area :- Department of pediatric medicine and Department of Biochemistry , Burdwan medical college and hospital b)STUDY POPULATION :- patients with nephrotic syndrome admitted in pediatric ward and attending pediatric OPD. Inclusion Criteria: - Children aged upto 7 yrs with typical features of nephritic syndrome. Patients were studied at onset of Nephrotic syndrome, during remission, and relapses. Exclusion Criteria :- Unwilling of patient Associated Known cardiac disease Associated Known liver disease Associated Known other kidney disease Associated Malnutrition Associated Protein losing enteropathy H/o – Diabetes mellitus H/oHypothyroidism H/o – Familial hypercholesterolemia c)Study Period :- March 2011 To February 2012 d)Sample Size :- Approximately 50 patients with nephrotic syndrome. e) Sample Design :- A prospective observational study which include approx 50 children with Nephrotic syndrome, selected by inclusion and exclusion criteria. They were clinically examined and lipid profile was done in each case before steroid therapy, after one month of therapy and at the end of therapy. f)STUDY DESIGN :- Institutional based prospective study. g)Parameters To Be Studied :- History & clinical examination. Biochemical test of serum - Total cholesterol By ; CHOD/PAP method. LDL cholesterol By; Friedwald equation. VLDL cholesterol By ; Calculation HDL cholesterol By ; Phosphotungstic Acid method By ; GPO/PAP method Albumin By ; BCG method. Urine for Total protein By; Sulphosalicylic acid method. h) Study Tools: - Patient proforma Case record form, OPD ticket, & BHT. Weighing machine Laboratory equipments & chemical reagentsRelated articles, books, journals.Consent form. i) Study Techniques: - Consents should be taken from the parents of the cases Record of history & clinical examination. Relevant laboratory investigations J) Plan For Analysis Of Data:-Data will be compiled, tabulated, & analysed with appropriate statistical methods, and subsequently P value is to be measured . P value < 0.05 will be taken as significant. NEP/2 (P) CLINICAL SPECTRUM AND OUTCOME OF CHILDREN WITH ACUTE PIGN-A DEVELOPING COUNTRY EXPERIENCE Prince Parakh, Mishra OP, Prabhakar R , Shah GS, Bhatta NK, Singh RR Dept.of Pediatrics,BPKIHS,Dharan Email: drprinceparakh@gmail.com Introduction-Acute Postinfectious glomerulonephritis(APIGN) is the commonest cause of severe acute glomerulonephritis in children. Children with PIGN present in different ways and with different lab pictures. Aims and Objectives: 1) To study various clinical presentation (symptoms &signs) and laboratory profile of Acute Post Infectious Glomerulonephritis. 2) To know the prognosis and outcome of the children suffering from APIGN. Materials and Methods: This Retrospective study was conducted studying the case reports of 54 children admitted to BPKIHS Pediatric Ward over a period of one year with features suggestive of APSGN. The information relating to the children included age, sex and presenting complaints, complete physical examination, investigation, treatment and outcome of the disease. Results - Acute PIGN constituted 22% of all renal cases admitted. Edema(85%), Hematuria(gross-74%,microscopic-6%),hypertension(83%),Abdominal pain (46%) ,Acute kidney injury(stage1-33%,stage 2-11.11%,stage3-1.86%) ,Fever(37%),Skin infections(40%),Fluid overload(47%) and Hypertensive encephalopathy(7.4%) were the chief presentations.94.4% patients required diuretics and 72.2% required antihypertensives.87% patients were discharged within 10 days whereas 13% patients required hospital stay > 10 days. There was no mortality. Conclusions- Prompt diagnosis in patient with mild renal compromise, hypertension, and urinary abnormalities is vital, as these patients could lose kidney function without urgent treatment. PIGN frequently presents with Acute kidney Injury and fluid overload which should be promptly recognized and treated to have better outcomes. Key Words-APIGN,Children,AKI. NEP/3 (O) MEMBRANO PROLIFERATIVE GLOMERULONEPHRITIS (MPGN): A PREDICTABLE MYSTERY? Rameshwar Gore, Santosh Kondekar, Surbhi Rathi, Shruti Hule, Priti Tamhankar, Sahebrao Ahire. Pediatric Resident, Department of Pediatrics, 1st Floor, College Building, TNMC & BYL Nair Hospital, Mumbai Central, Mumbai-400008 Email id: drrameshwargore@gmail.com Abstract- Introduction-MPGN commonly occurs in older children and young adults and presents with nephrotic or nephritic syndrome. Unlike any other nephritic or nephrotic conditions, MPGN may not be predictable from clinical history and examination. Hereby we present a series of 4 cases of type I MPGN that presented with totally different clinical history and some related complications. Case History- Case 1- A 4 1/2 year old girl case of frequently relapsing steroid responsive nephrotic syndrome admitted with 7th relapse. Screening for secondary causes of nephrotic syndrome was negative. Renal biopsy was done due to age of onset being 1 year age , Electron microscopy(EM) and immunoflorescence (IF)was suggestive of type I MPGN. Case 2 –A 10 yr old boy presented as chronic glomerulonephritis (Nephritic features along with hypertension for 8 months), serum C3 being low, ASLO titer-normal, secondary workup was negative. Renal biopsy EM&IF performed in view of CGN was suggestive of type I MPGN. Case 3-A 5yr old girl presented as acute glomerulonephritis with hypertensive encephalopathy. on investigation urine albumin 3+,serum C3 was low, other secondary workup negative. Biopsy was performed in view of presentation with a complication. Renal biopsy finding was suggestive of type I MPGN. Case 4 –An 8 yr old girl presented with features of acute glomerulonephritis without hypertension. Though clinical diagnosis was PSGN due to ASLO being 800; persistence of cola hematuria for more than 4 weeks indicated an unusual course. Renal biopsy EM &IF shows type I MPGN. Discussion: There is enough literature to state that MPGN cannot be suspected from clinical presentation and it has always been a surprise diagnosis. Although the four cases looked straightforward, each had an unusual feature. It becomes crucial to keep a watch for unusual features in each case of nephrotic or nephritic syndrome.MPGN prognosis and therapy depends on the histopathological pattern. Hence timely histopathological diagnosis can help predict the prognosis. Conclusion-Early index of suspicion and early biopsy in case of atypical presentation; will stop us from starting empirical therapy for AGN and or nephrotic syndrome which may give overestimated better prognosis. NEP/4 (O) DENSE DEPOSIT DISEASE (MEMBRANOPROLIFERATIVE GLOMERULONEPHRITIS TYPE II)- RARE ENTITY Rameshwar Gore, Varun Bansal,Radha Ghildiyal, Poonam Sankhe, Jane David. Dept. of Pediatrics, BYL Nair Ch. Hospital and TN Medical College, Mumbai-8 Email: drrameshwargore@gmail.com Introduction: Membranoproliferative Glomerulonephritis(MPGN) type II is also known as Dense deposit Disease,is a rare entity.The incidence being 2-3/10,00,000.It is usually seen in older children , the mean age of onset being 10 year with slight female preponderance. Case history: 11 year old girl, diagnosed as a case of atypical nephrotic syndrome at 9 years of age, was admitted with third relapse of nephrotic syndrome. screening for secondary cause of nephrotic syndrome was negative.As serum C3 level was low renal biopsy was done. Electron Microscopy and Immunoflorenscence examamination was suggestive of Dense deposit disease.Child required extended course of steroids in high doses along with Cyclophosphamide and antihypertensive drugs. Discussion: MPGN type II is a caused by uncontrolled activation of alternate pathway of.complement cascade. The condition may arise as an inherited disorder with factor H deficiency. Factor H dysfunction is due to presence of C3 Nephritic Factor (C3 Nef),which is an Ig G antibody that binds to C3 convertase of alternate complement pathway,preventing cleavage of C3bBb and permiting breakdown of C3. It is characterized by proteinuria, hematuria ,nephrotic syndrome, acute nephritic syndrome ,recurrent gross hematuria or azotemia. Long term administration of alternate day predniolone (1-1.5 mg/kg) combined with Angiotensin converting enzyme inhibitor is considered standard therapy. Cyclophosphamide, Mycophenolate have been tried with little success. Almost all cases progress to end stage renal diseae with in 10 years of diagnosis. Conclusion: MPGN type II should be suspected in a case of atypical nephrotic syndrome, with low C3 level. Early treatment with long term steroid may induce remission in these patients. NEP/5 (O) DISTAL RENAL TUBULAR ACIDOSIS PRESENTING HYPOKALEMIC PERIODIC PARALYSIS- A CASE REPORT Shivani Deswal, Pradeep Debata, Murtaza Kamal, K.C Aggarwal. Department of Pediatrics, Safdarjung hospital & V.M.M.C, New Delhi Email: shivanipaeds@gmail.com AS Renal tubular acidosis (RTA) is a group of tubular transport disorders characterised by inability to appropriately acidify urine, a normal anion gap (hyperchloremic) metabolic acidosis in the setting of normal or near-normal glomerular filtration rate. DRTA defect is usually secretory, characterised by an inability of the tubular cells to secrete H+ ions leading to inappropriately alkaline urine (urine ph>6) despite systemic acidosis (bloodpH<7.2). Hypercalciuria, hypocitraturia and hypokalemia are also usually present. A four year old unimmunised boy of average growth presented with lower limb weakness that had progressed slowly to involve his upper limbs over a period of 12 hours without history of preceding upper respiratory tract infection, diarrhoea , intramuscular injection and seizures.The patient did not have any weakness of the cranial nerves or respiratory muscles, or any sphincteric disturbance.Had similar history one year back, for which he was treated as a case of GBS and received IVIG for two days. Vitals were stable with a fairly normal general physical examination. Power was 2/5 in bilateral lower limbs and 3/5 in upper limbs, with normal tone and deep tendon reflexes, flexor plantars , normal sensory and cranial nerve examination. The investigations showed normal hemogram and counts, ABG (pH =7.178,HCO3- 9.8meq/L).Electrolytes- Na+ 142meq/L,K+ 2.2meq/L, Ca+ 10.1meq/L,PO4 very high, ALP 1307,Blood urea- 26mg/dl, S.creatinine 0.5mg/dl, TSH 5.09IU, ECGhypokalemic changes, NCV normal study, CPK 92IU/L ,urinary ph 7,Urine anion gap – raised-106meq/L (urinary Na+ 143meq/L,K+ 49.5meq/L,Cl-67meq/L, Ca+ 13.4meq/L), Ultrasonography KUB –normal.Alkali solution(urilizer) and potassium supplements were started and the patients weakness improved completely and on follow up blood bicarbonates improved to near normal with normal serum electrolytes. The diagnosis of DRTA in our patient was made from his inability to acidify urine in the face of metabolic acidosis with hypokalemia. Thus, an important presentations of distal renal tubular acidosis (DRTA) is recurrent hypokalaemic weakness, which can be life threatening if not suspected and treated timely. NEP/6 (P) SALMONELLA TYPHI PRESENTING AS ACUTE GLOMERULONEPHRITIS IN TWIN SIBLINGS Girish Chandra Bhatt, Devki Nandan,Vivek Dewan, Nirmaljeet Kaur Associate Professor, Pediatrics, PGIMER & Associated Dr RML Hospital New Delhi, India Email- devkinandan2002@yahoo.com; drgcbhatt@gmail.com Abstract: Introduction: Acute glomerulonephritis occurring during the course of enteric fever is a rare entity and only few cases are reported in the literature. Two interesting cases of acute glomerulonephritis occurring in twin siblings are described. Case 1: Ten years old, first of twin siblings presented with complaints of moderate grad fever for last 7 days, pain abdomen from last 2 days and passing dark coloured urine on the day of admission. There was no history of oliguria, swelling over body, pyoderma or sore throat. Examination revealed temperature of 102.80C, heart rate of 98/minute and blood pressure of 108/60mm of mercury. Per abdomen examination revealed soft non tender enlarge liver (4cm below subcostal margin with smooth surface) and enlarged spleen 2 cm below subcostal margin. which was further confirmed by ultrasonography. Urinary examination showed proteinuria of 1.1 gm/day, with presence of 70-80 red blood cells(RBC’s) with more than 75% dysmorphic RBC’s. Phase contrast microscopy further confirmed the presence of dysmorphic RBC’s. Blood culture was sent which was positive for Salmonella typhi and widal was positive (TH and TO ;1:340). Rest of the work up was inconclusive. Case 2: Second of twin sibling presented with fever for last seven days and pain abdomen for last 2 days. Examination revealed a temperature of 102.60F, heart rate of 92/min, respiratory rate of 20/min and normal blood pressure (104/62mm of mercury). Per abdomen examination revealed hepatosplenomegay. Urinary examination showed proteinuria of 960mg/d with 20-30 RBC cast which were further confirmed on phase contrast microscopy. S.typhi was grown in blood culture and widal was positive(TH and To;1:240). Rest of the work up was inconclusive. Renal biopsy was refused by the parents. A diagnosis of acute glomerulonephritis due to S.typhi was made and patient was commenced on ceftriaxone therapy. Hematuria disappeared in both cases during 4th week on follow up. Conclusion: Enteric fever may sometime present with rare clinical manifestations, such as acute glomerulonephritis as in our case. Early treatment of typhoid fever with intravenous antibiotics and fluid management prevents further progression of the disease. Furthermore, familial occurrence of this rare complication may be an incidental finding in this case, it is indeed intriguing and requires further research. NEP/7 (P) A CASE REPORT OF CONGENITAL DISTAL RENAL TUBULAR ACIDOSIS PRESENTING AS RECURRENT CHEST INFECTION Barik Chinmay, Chandan CK,Mohanty Ajay ,Mohanty Niranjan C/O Narahari Barik, Maitri Vihar, Jagannathpur, Bhadrak, Orissa Email: chinmay.scb@gmail.com A 4 month 1.9kg female child of birth weight 2.5kg born out of nonconsanguinous marriage presented to our emergency OPD with severe respiratory distress,loosing of weight since birth. She was very sick looking and cachectic.On enquiry she had two prior similar episode of chest infection for which hospitalized and relieved. There was history of polyuria,loss of weight and frequent vomiting. On examination she was dehydrated,skin pinch going slow,rapid thready pulse,bilateral crepitation in chest,no obvious cardiological abnormality. She was stabilized and routine investigation done. Hemoglobin-9.6mg/dl, TLC-14,450/cmm. DC-N-68%, L-30%, E-2%, platelet count - 3.2lac/cmm, serum urea-102mg/dl, serum creatinine-1.8,serum NA+-149meq / l,S. K+2.9meq/l,s. ca++8.9mg/dl,s.albumin-3.8mg/dl. Urine sugar, ketone bodies and albumin was negative. Urine c/s-no growth and blood c/s-no growth. Urinary CA++: Creatine-.28. Urinary Ph-7, not improved with ingestion of frusemide.Urinary anion gap +30meq/l. Artery blood gas analysis showed Ph 7.080,bicarbonate-6.2mmol/l, base excess-22.5mmol/l. On USG ABDOMEN bilateral medullary nephrocalcinosis found.serum PTH-46pg/l.chest x ray-bilateral patchy opacities found. She was treated with intravenous antibiotic for bronchopneumonia . After stabilization oral syrup potassium citrate ( SOHL SOLUTION),syp calcium given.After 14 days she had significant general improvement with gain of wieght. ABG showed pH 7.249, bicarbonate18.9, base excess-8.7. Conclusion- Infants presenting with failure to thrive with clinical picture of sepsis or bronchopneumonia renal causes must be kept on mind. Correct & early diagnosis and long term treatment required to prevent complication and morbidity of children. NEP/8 (P) A STUDY OF THE CARDIOVASCULAR RISKS IN CHILDREN WITH CHRONIC KIDNEY DISEASE Dulari Gupta, Indira Agarwal, Swasti Chaturvedi, Sunil Chandy Department of Pediatrics, Christian Medical College, Vellore Email: dularigupta@gmail.com Introduction: Cardiovascular risks are a leading case of mortality and morbidity amongst children with chronic kidney disease. They are responsible for 20-41% of death in children with Chronic Kidney disease (CKD). These risks are often ignored during normal clinical practice. Aims And Objectives: This is a cross-sectional study of the cardiovascular consequences in children with CKD aged 1-18 years with GFR < 60 ml/min/1.73 m2. The prevalence of Left Ventricular Dysfunction by ECHO and of hypertension- both manifest (clinic BP) and latent hypertension (Ambulatory Blood Pressure Monitoring- ABPM) was studied. Materials And Methods: 37 children with CKD, of which 9 were on dialysis had ECHO, Clinic BP and ABPM monitoring. LVH was defined as lvmass > 95th centile for age and sex. ABPM was correlated with clinic BP readings. Results: 8 children had clinic hypertension (14.2% of CKD, 44.4% on dialysis). Nine more children were found to be hypertensive using ABPM. The BP load (defined by BP > 25% of 95th centile) was increased in 18 children (39.2% of CKD, 77.7% on dialysis), with loss of nocturnal BP dipping in 17 children (33.3% of CKD, 88.8% on dialysis). Fourteen children were found to have LVH (77.7 % of children on dialysis and 25% of children with CKD). Conclusions: LV Hypertrophy is common amongst children with CKD, especially those on dialysis. APBM was able to identify more hypertension in children compared to single clinic BP readings alone. It is important to look for and treat these cardiovascular risk factors to decrease morbidity and mortality.