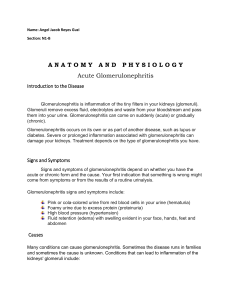
Glomerulonephritis
advertisement

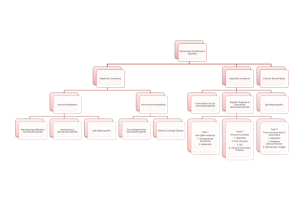
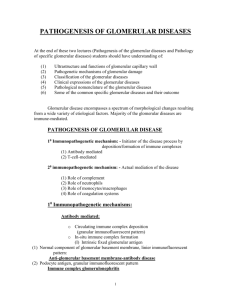
Glomerulonephritis Dr. Abdelaty Shawky Dr. Gehan mohamed • Glomerular diseases constitute some of the major problems in nephrology; indeed, chronic glomerulonephritis is one of the most common causes of chronic renal failure in humans. • Glomeruli may be injured by a variety of factors and in the course of a number of systemic diseases. Systemic immunologic diseases such as systemic lupus erythematosus (SLE), hypertension and polyarteritis nodosa, diabetes mellitus, often affect the glomerulus. • These are termed secondary glomerular diseases to differentiate them from disorders in which the kidney is the only or predominant organ involved. 2 * Classification of glomerular diseases: I. Primary G.N (the disease affects kidney only): • Minimal change glomerular disease (Lipoid nephrosis). • Acute diffuse proliferative G.N: – Post-streptococcal G.N. – Non-post-streptococcal GN. • Rapidaly progressive G.N. • Membraneous G.N. • Membranoproliferative G.N. • Chronic G.N. 3 II. Secondary G.N (the disease affects kidney and other organs): – Systemic lupus erythematosus (SLE). – Polyarteritis nodosa (PAN). – Wegener granulomatosis. – Diabetes mellitus (diabeteic nephropathy). – Goodpasture syndrome. – Amyloidosis. 4 Normal Glomerulus 5 6 7 • Most of the 1ry glomerular disease are due to immunologic mechanisms. • To study any glomerular disease, a renal biopsy is taken and examined by 3 types of microscopes: 1. Light microscope: to examine the structure of glomeruli, tubules and interstitium. 2. IF (immune flourescent microscope): to detect the type of deposited immunoglobulin in the glomeruli. 3. EM (electron microscope): to detect the site of immune complex, either sub-epithelial, subendothelial, mesangial or basement membrane.. 8 Minimal change glomerular disease 9 *Etiology & pathogenesis: • Chemical change in the glomerular basement membrane causing protein loss. 10 * Grossly: • Mild bilateral kidney enlargement. * LM (Light microscope): • No abnormalities. * IF (Immunoflurescence): • No immune deposits. * EM (Electron microscope): • Fusion of the foot processes of the epithelial cells (podocytes). 11 EM of normal glomerulus 12 EM of minimal change glom. disease 13 * CP (Clinical picture): • Affect children and young adults. • Cause nephrotic syndrome. * Fate: • The disease has excellent prognosis and most patients respond to corticosteroids with complete resolution of proteinuria. 14 Post-streptococcal G.N 15 *Etiology & pathogenesis: • Immune complex reaction; (nephrotegenic strains of group A beta haemolytic streptococci + Ig G), the complex is deposited in the glomeruli with subsequent complement activation acute inflammation. 16 * Grossly: • Mild bilateral kidney enlargement with petechial haemorrhages. 17 * LM (Light microscope): a. Glomeruli: • Proliferation of endothelial and mesangial cells. • Glomerular capillaries contain neutrophils. • Bowman’s space shows: neutrophils, RBCs, some albumin. b. Tubules: • The lining cells are swollen. • The lumens show casts (RBCs casts, neutrophil casts & hyaline casts). c. Interstitium: • Acute inflammatory reaction…... 18 Normal kidney 19 Normal kidney 20 Post-streptococcal GN 21 Post-streptococcal GN 22 Post-streptococcal GN 23 Post-streptococcal GN 24 * IF (Immunoflurescence): • Deposition of Ig G and C3. 25 Positive Ig G and C3 26 * EM (Electron microscope): • Subepithelial immune complex deposit (humps). 27 28 * CP (Clinical picture): • In the classic case, a young child abruptly develops malaise, fever, nausea, oliguria, and hematuria (smoky or cocoa-colored urine) 1 to 2 weeks after recovery from a sore throat. • The patients exhibit red cell casts in the urine, mild proteinuria (usually less than 1 mg/day), peri-orbital edema, and mild to moderate hypertension. 29 Hematuria (coca cola colored urine) 30 RBCs cast • In adults, the onset is more likely to be atypical, with the sudden appearance of hypertension or edema, frequently with elevation of serum creatinine. Important laboratory findings include elevations of anti-streptococcal antibody (ASO) titers and a decline in the serum concentration of C3 (consumed). 31 • More than 95% of affected children eventually recover totally with conservative therapy aimed at maintaining sodium and water balance. • A small minority of children (perhaps less than 1%) do not improve, become severely oliguric, and develop a rapidly progressive glomerulonephritis. • Some of the remaining patients may undergo slow progression to chronic glomerulonephritis. 32 • In adults, the prognosis is bad. Most of the patients pass to rapidly progressive glomerulonephritis or chronic renal failure. 33 Nephritic syndrome - A syndrome formed of: 1. Haematuria. 2. Oliguria. 3. Peri-orbital oedema. 4. Hypertension. - The most common cause of nephritic syndrome in children is post-streptococcal GN. 34 Nephrotic syndrome - A syndrome formed of: 1. Hypoproteinaemia. 2. Proteinuria . 3. Oedema. 4. Hypercholesterolaemia. - The most common cause of nephrotic syndrome in children is minimal change glomerular disease. - The most common cause of nephrotic syndrome in adults is membranous GN. 35 Thanks References: Robbins and Cotran’s: Pathologic Basis of Disease. Seventh edition. 36