Crohns and Ulcertaive Colitis
advertisement

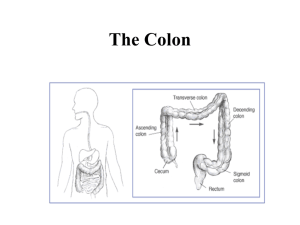
Radiology Website http://myweb1.lsbu.ac.uk/~dirt/museum/ http://myweb1.lsbu.ac.uk/~dirt/museum/unk-gastro.html for case histories with radiology Clinical presentation: A 26 year old woman gives a history of increasing abdominal pain with blood and mucus in the stool. The plain film shows visible gas-filled colon with variable mucosal thickening, giving typical thumb-printing appearance. The colon appears shorter than normal and has lost its usual haustral pattern. The 'instant' barium enema, without preparation, demonstrates an extensive continuous involvement of the bowel with areas of mucosal thickening and areas of mucosal loss. There are visible ulcers, particularly in the descending colon where they have a typical undercut edge. The process gives a granular appearance to the sigmoid colonic mucosa. In the tranverse and ascending colon, the mucosa is irregularly thickened. There is a general loss of the normal haustral pattern. Plain X Ray Abdomen Barium Enema D/D Crhon’s colitis Plain X-Ray Toxic Dilatation Colon Diverticulosis Carcinoma Colon in pre existing U. Colitis 19 year old with a 9 year history of bowel disorder. The view is a late follow-through examination. The terminal ileum is wide and featureless. The colon is shortened and featureless, except in the transverse colon where is appearance is probably redundancy of the taeniae. The contrast shows mucosal coating with unformed faecal material. There is a block to the transit of barium suspension at the splenic flexure. This takes place at a point where acute angles are formed as the walls of the colon end in an irregular convexity of soft-tissue density. The appearance does not exclude the possibility of more proximal mucosal thickening, but at the time this picture was taken, additional imaging was not available A barium enema has demonstrated irregular narrowing of the sigmoid colon at its junction with the descending colon. The affected area shows variable nodular mucosal thickening and occasional Crohn’s Disease deep ulcers "rose thorn" appearance. Asymmetrical involvement of the mid-sigmoid colon gives an area of wall thickening and ulceration on its right side. A further section of irregularly strictured sigmoid colon lies in the mid-line. A collection of barium over this loop has an ambiguous appearance and resembles an extra-luminal process. A biconcave area outlined by barium on the left side of the pelvis, adjacent to the rectosigmoid junction might also represent extraluminal contrast. The terminal ileum is opacified and shows irregular mucosal thickening and deep ulceration. Crhon’s Disease Skip Lesions 30 year old female with abdominal pain and fever. Ileo-coecal Crhon’s This oblique view in a barium followthrough examination shows two adjacent abnormal loops, including terminal ileum. There is narrowing with irregular mucosal thickening. Occasional penetrating ulcers can be seen in the terminal ileum. There are two calcific ring densities in the right para-midline epigastrium. A single view of underfilled small-bowel peristalsis is, by definition, inconclusive. Clinical presentation: Female, 40 year old, with right iliac fossa abdominal pain. The follow-through barium examination shows contrast in the ascending colon, which has not reached the splenic flexure. The examination shows contrast in widely separated loops of narrowed ileum. These show generally thickened mucosal folds. There is pseudodiverticula formation on the antimesenteric side of the terminal ileum about 15 cm.from the ileocaecal valve. Nearer the valve, a fistula from the ileum has filled sigmoid colon. The distribution of affected bowel suggests an inflammatory mass with its centre of radius over the medial side of the lower pole of the caecum. Ileo-Coecal Crohn’s with Fistula in Sogmoid Colon Clinical presentation: Follow-up of a 30 year old female for known chronic condition treated conservatively for the last 10 years. Crohn's disease http://myweb1.lsbu.ac.uk/~dirt/museum/p7-262.html Crohn's disease is an inflammatory condition of bowel that may affect any part of the bowel, including stomach. Its other name indicates its commonest location, regional ileitis. The causative agent (agents?) has still not been identified. Recent culprits include a mycobacterium from sheep, which causes Johnes disease in them and is thought to be transmitted by inadequately pasteurised milk to vulnerable humans. The theory is a worthy successor to those of Tooth-paste particles, or measles and impaired mucosal vascularity. Other theories include the combination of an immature immune system that is exposed to an antigen, or infective agent, with the possibility of an inherited vulnerability. Despite research, conclusive proof of a causative agent is not available yet... The pathology affects the whole thickness of the bowel and produces a rigid and narrowed bowel. The wall-thickening separates adjacent loops. In contra-distinction to Ulcerative Colitis, the involvement of the bowel is typically irregular and discontinuous. The mesenteric and antimesenteric margins may be affected to differing degrees. There is serosal involvement and more reaction in the regional lymph nodes. The mucosal involvement is of nodular thickening and fissures that may be deep, "rose thorn ulcers". Microscopy reveals non-caseating granulomas, rather like Sarcoidosis. Fibrosis develops in the diseased segments. Where there is colonic involvement, the pathology is often typically asymmetric. A pan-colitis may also be seen. Generally, extensive or continuous colitis is often seen on the plain film as an unusually large length of undilated gas-filled bowel, implying a local lack of peristalsis. If there is colonic dilatation, the same reasoning as in Ulcerative colitis applies to the relationship between diameter and wall-tension. Because of the involvement of the whole wall, fistula formation is common. The fistula may link the affected bowel with other loops, or may join to other hollow organs or even may fistulate to the skin. Perineal fistulae may be a clinical indication of Crohn's disease. The process may interfere directly with nutrient absorption or indirectly through non-absorption in the terminal ileum of the constituents of the entero-hepatic circulation and secondary effects from the lack of bile salts. Anaemia and fat-soluble vitamin deficiencies are clinical sequelae. Long term, there is some increased chance of adenocarcinoma. This risk is less than in Ulcerative Colitis, but assessment is much more difficult in Crohn's disease with so many strictures that are present anyway. There is an increased risk of arthropathies in bowel disorders. The association varies, depending on the underlying pathological process. A vasculitis is easy to associate, but bowel disorders with their effects on absorption of nutrition and toxins may have a more complex aetiology. A large proportion of those patients with a Sacroiliitis in Crohn's or other Colitis test positive for the HLA B27 antigen, which is often found in Anklyosing Spondylitis. On follow-through examination, the abnormal loops are revealed by the bowel-wall thickening and the inflammatory mass that separates the loops with lots of space around them. This same inflammatory mass can be seen on ultrasound examination, often tender to palpation. Various anatomic expressions of pathology. Cobblestone mucosa terminal ileum (cases reports) inflammat ory mass, abcess terminal ileum (cases report) Asymmetric involvement string sign. (case report) Ileal incidental gallstones (case report) Involvement of adjacent loops, fistula? (case report) Colitis with ileum involved. (case report) Colitis with skip-lesions. (case report) Postresection Recurren ce (case report) Fistula, ileocolic. (case report) Fistula vesico ureteric junction (case report) Hypertrophic Osteoarthrpa thy, HPOA. (case report) associate d Sacroiliitis (case report) Ileal Obstruction, sacroiliitis (case report) Ulcerative Colitis http://myweb1.lsbu.ac.uk/~dirt/museum/p75-261.html Ulcerative colitis is an inflammatory process in the bowel that can be found at any age, but has its peak incidence in young adults (about 80% between 20 and 40 years in UK.). The bowel is typically involved by a fairly superficial mucosal inflammation in a continuous area of bowel. The presence of a continuous pattern of colitis with rectal bleeding helps to distinguish the condition from Crohn's disease. The distal part of the bowel is involved in Ulcerative Colitis with more extensive cases having greater involvement of the proximal bowel. The mucosa may become oedematous, particularly if there is haemorrhage or secondary infection by opportunist or commensal organisms. The absorption of toxins from the bowel contributes to the clinical picture. The Radiology contributes to the management, but the management of a toxic colitis will often depend on general clinical assessment, including colonoscopy. The plain film will often give a clue to the degree of involvement. Since normal peristalsis has to affect short segments of bowel, by definition, the presence of visible gas-filled long segments of bowel implies an ileus. The plain film abdomen may demonstrate visible gas-filled anhaustral colon, without its usual faecal contents. The extent of the emptying of the faecal material from the colon can give an indication of the extent of colitis. At barium enema, the view will show superficial ulceration and a shortened bowel, often without the usual haustral pattern. The ulcers are typically shallow and can be wide mouthed with undercutting of the mucosa, sailor hat ulcers. The mucosa may slough off (incompletely) and leave oedematous tags of mucosa, the pseudo-polyps. Inflammation, by its effect on peristalsis, may give an appearance of proximal bowel dilatation. Given the abundance of intraluminal material (and gas) that goes through the ileo-caecal valve and accumulates from colonic inflammatory exudate, it is worth noting that colonic bacterial fermentation will not be completely suppressed by problems with colonic wall movement. The colon may show atonic gaseous dilatation and this can be a Radiological indication of a Toxic Colitis. The assessment of possible developing colitis must include clinical features. Recognisably dilated colon on the plain film may arrive a little too late to benefit the patient, if surgery proves necessary. The plain film may hint at the degree of wall involvement, but is not accurate at predicting the point of failure. Bowel dilatation can increase to a point where the tension and stretching of the wall may impair its blood supply. Even if relative pressures inside the bowel and abdomen remain the same, the geometry means that an increase in radius 'r' will mean an increase in the tension 't' in the wall. The point at which normal bowel may perforate is about 10 cm. diameter. The crucial point is that abnormal bowel may perforate earlier. At some stage, surgical intervention may be necessary. This is where co-operative clinical assessment becomes so important. The last thing anyone wants is for the surgeon to have to operate on necrotic bowel. The presence of a severe colitis may be indicated by mucosal thickening, widely dilated bowel, extensive involvement and gas in the bowel wall. If you wait for these without paying attention to the clinical features, then Surgery might be too delayed. A colleague once described the situation "like trying to sew up wet blotting paper" (loose weave soft paper), not to mention the greater risk of faecal soiling of the peritoneum. The text book definition of Toxic Dilatation of the Colon is of systemic toxicity in a patient whose colonic diameter exceeds 6cm, but no author would recommend delaying surgery on a particular measurement. In addition to the general symptoms of ill-health, there may be an arthropathy, often with a Sacro-iliitis, sometimes with a uveitis as well. Erythema nodosum, pyoderma gangrenosum may also occur in combination with inflammatory bowel disease. Longer term complications of Ulcerative colitis include ascending cholangitis. It's not a bad idea to ask for a history of bowel disorder in unknown chronic liver disease, especially if the bile ducts appear a little irregular on Liver ultrasound. Strictures with fibrosis rarely occur in Ulcerative colitis. If there is a long history you should consider the possibility of Carcinoma being the cause of an smooth stricture of the colon. In a patient with a long history, not only is carcinoma a higher risk, up to 30% in some families, but the presentation may be atypical. Multiple tumours are also commoner than the usual 5%. Each case of Ulcerative Colitis is managed individually and supervised by regular colonoscopy. It is not appropriate to make a general statement about the time to proceed to pre-emptive colectomy, but indications include epithelial dysplasia and polyp formation. Various anatomic expressions of pathology. Smallbowel fluid-levels (case report) Ulcers and mucosal thickening (case report) Sailor-hat ulcers (case report) Typical acute appearanc e on plain film. (case report) Toxic dilatation. (case report) Pseudopoly ps (case report) Preexisting diverticulos is. (case report) Carcinoma 9 year history of colitis (case report). Carcinoma s can be atypical and may resemble fibrous strictures. TB Intestine Journal of Medical Case Reports 2008, 2:90 A 14-year-old girl presented with complaints of paraplegia, ataxia, fever and fatigue that had started a few months earlier, which had progressively worsened in the last three weeks. Her laboratory results were indicative of macrocytic anemia with a serum B12 level <100 (normal, 160-970) pg/ml and hypersegmented neutrophils and MRI revealed brain atrophy. Her fever workup eventually led to the diagnosis of tuberculosis, documented by bone marrow aspiration smear & culture. A small bowel series showed that tuberculosis had typically involved the terminal ileum which had resulted in vitamin B12 deficiency. She was treated for vitamin B12 deficiency and tuberculosis. Her fever ceased and her hemoglobin level returned to normal. This is the first report of macrocytic anemia with unusual manifestations such as brain atrophy and seizures due to intestinal tuberculos . Brain MRI shows senile dilatation in the CSF space and sulci of brain hemispheres that is compatible with mild atrophic changes. Plain X-Ray abdomen