Atropine CoSTaR (Feb 14th 2015)
advertisement
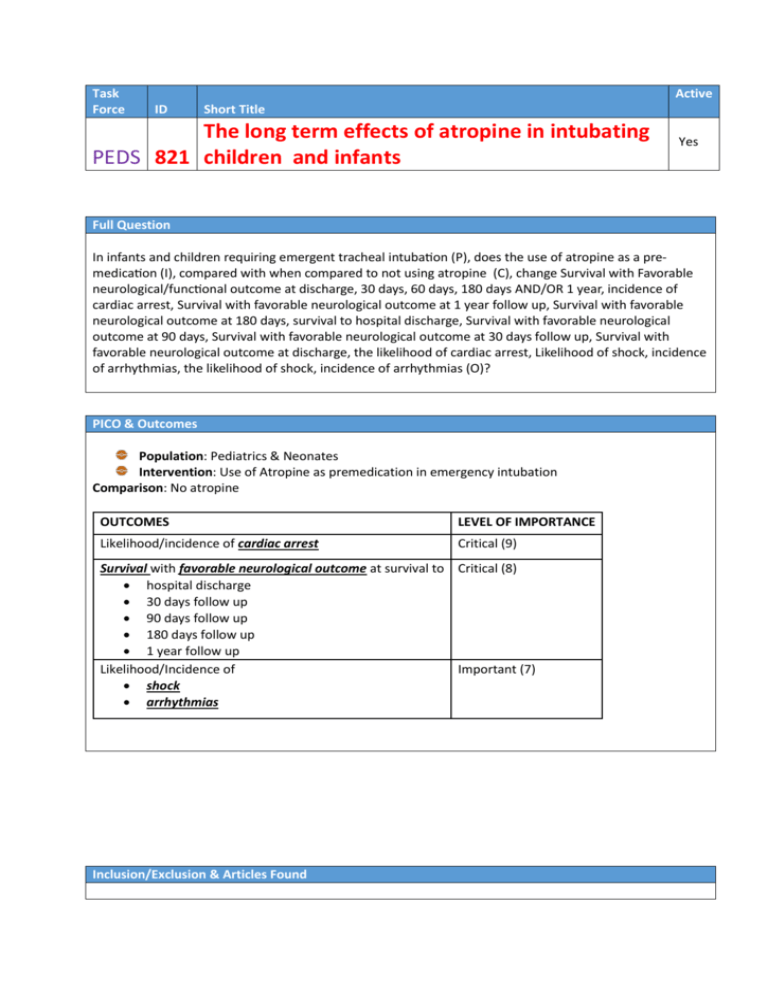
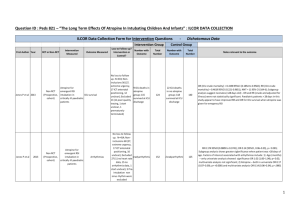
Task Force Active ID Short Title The long term effects of atropine in intubating PEDS 821 children and infants Yes Full Question In infants and children requiring emergent tracheal intubation (P), does the use of atropine as a premedication (I), compared with when compared to not using atropine (C), change Survival with Favorable neurological/functional outcome at discharge, 30 days, 60 days, 180 days AND/OR 1 year, incidence of cardiac arrest, Survival with favorable neurological outcome at 1 year follow up, Survival with favorable neurological outcome at 180 days, survival to hospital discharge, Survival with favorable neurological outcome at 90 days, Survival with favorable neurological outcome at 30 days follow up, Survival with favorable neurological outcome at discharge, the likelihood of cardiac arrest, Likelihood of shock, incidence of arrhythmias, the likelihood of shock, incidence of arrhythmias (O)? PICO & Outcomes Population: Pediatrics & Neonates Intervention: Use of Atropine as premedication in emergency intubation Comparison: No atropine OUTCOMES LEVEL OF IMPORTANCE Likelihood/incidence of cardiac arrest Critical (9) Survival with favorable neurological outcome at survival to Critical (8) hospital discharge 30 days follow up 90 days follow up 180 days follow up 1 year follow up Likelihood/Incidence of Important (7) shock arrhythmias Inclusion/Exclusion & Articles Found Inclusion Criteria - atropine, infants and children, emergent intubation, human Exclusion Criteria - case reports, animals, adults, abstracts, reviews No Articles initially identified = 54 No Finally Included in Evidence Profile tables = 3 observation studies RCTs = 0 Non-RCTs = 3 Risk of Bias in studies Non-RCTs = 3 Evidence profile tables Survival In PICU Arrhythmias Non-RCTs = 3 Consensus on Science For the critical outcome of survival with favorable neurological outcome, there was no study identified that addressed this for when atropine was used for in-hospital emergent intubation. For the critical outcome of survival to ICU discharge there was very low quality evidence (downgraded for risk of bias & imprecision) from one pediatric observational study of in-hospital emergent intubation (Jones, 2013, 264) of 264 infants and children, supporting the use of atropine pre-intubation for those patients >28 days of life. The use of atropine pre-intubation for neonates was not significantly associated with survival to ICU discharge. (Neonates: propensity score adjusted OR 1.3, 95%CI 0.31–5.1 p=0.74; Older children OR 0.22, 95%CI 0.06–0.85, p = 0.028) For the critical outcome of likelihood/incidence of cardiac arrest there was no study identified that addressed this for when atropine was used for in-hospital emergent intubation For the important outcome of likelihood/incidence of shock or arrhythmias we have identified very low quality evidence (downgraded for risk of bias, inconsistency and imprecision) from two pediatric observational studies. One study of 322 emergent pediatric intubations (Jones, 2013, 289) showed that the use of atropine pre-intubation was significantly associated with a reduced incidence of any dysrhythmia (OR 0.14 95% CI 0.06–0.35) [p value removed for consistency], while the second study of 143 emergent pediatric intubations (Fastle, 2004, 651) failed to find an association between the pre-intubation use of atropine and a reduced incidence of bradycardia (OR 1.11 95% CI 0.22-5.68). Treatment Recommendations There is insufficient evidence for the routine use of atropine as a premedication for emergent intubation in infants and children. (Weak recommendation, Very low quality of evidence) Knowledge Gaps There are very few papers that have studied the effects and outcomes of atropine. Further studies, preferably RCTs would help shed light on the effects of atropine when used in emergent intubations in infants and children. Specific research is required particularly for: Survival with neurological outcomes Incidence of Arrhythymias Values & Preferences In making our treatment recommendation, we placed value on causal outcomes from use of atropine. There was only 1 study (low quality of evidence) that showed a higher ICU survival in children > 28 days with while there was unclear evidence on the relationship between use of atropine and arrhythmias. Therefore, due to insufficient and conflicting low quality evidence, we cannot recommend the routine use of atropine in emergent intubation in infants and children until further studies are done.