Atropin Stragen solution for injection, prefilled syringe ENG SmPC
advertisement

SUMMARY OF PRODUCT CHARACTERISTICS
1.
NAME OF THE MEDICINAL PRODUCT
Atropin Stragen 0.1 mg/ml solution for injection in prefilled syringe
2.
QUALITATIVE AND QUANTITATIVE COMPOSITION
Each ml of solution for injection contains 0.1 mg atropine sulphate. Each 5 ml pre-filled syringe contains
0.5 mg atropine sulphate.
Excipients with known effect:
This medicinal product contains sodium.
One ml contains 3.54 mg sodium equivalent to 0.154 mmol of sodium.
Each 5 ml pre-filled syringe contains 17.7 mg sodium equivalent to 0.77 mmol of sodium.
For the full list of excipients, see section 6.1.
3.
PHARMACEUTICAL FORM
Solution for injection in prefilled syringe
Clear and colourless solution.
4.
CLINICAL PARTICULARS
4.1
Therapeutic indications
Atropin Stragen solution for injection is indicated for:
Vagus-induced bradycardia and bradycardiac conditions in which inhibition of vagus-tone is indicated
(e.g. sinus bradycardia, atrioventricular block).
Pre-anaesthetic medication.
Treatment of an overdose of anticholinesterases as an antidote; in the treatment of poisoning from
organophosphorous insecticides or from chemical warfare 'nerve' gases and in the treatment of
mushroom poisoning.
4.2
Posology and method of administration
Posology
Vagus-induced bradycardia and bradycardiac conditions in which inhibition of vagus-tone is indicated:
Intravenous use.
Adults:
0.5 - 1 mg atropine sulphate (5 - 10 ml).
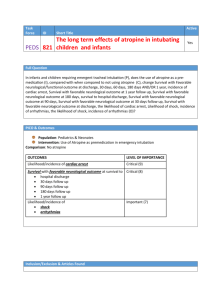
Paediatric population:
The usual dose in children is between 0.01-0.02 mg/kg body weight up to a maximum of 0.6 mg per dose,
dosage should be adjusted according to the patient’s response and tolerance.
Pre-anaesthetic medication:
Intravenous administration immediately before surgery; if necessary an intramuscular administration 30-60
minutes before surgery is possible.
Adults:
1
0.3 – 0.6 mg atropine sulphate (3 – 6 ml)
Paediatric population:
The dosage ranges for the paediatric age groups as stated below are values for guidance. The usual dose in
children is between 0.01-0.02 mg/kg body weight (maximum 0.6 mg per dose), dosage should be adjusted
according to the patient’s response and tolerance.
Body weight (kg)
Atropine sulphate (mg)
Atropin Stragen
0.1 mg/ml Solution for
Injection (ml)
3 - 10
0.10 – 0.15
1 – 1.5
10 - 12
0.15
1.5
12 - 15
0.20
2
15 - 17
0.25
2.5
17 - 20
0.30
3
20 - 30
0.35
3.5
30 - 50
0.40 – 0.50
4-5
In overdose of anticholinesterases as an antidote; in the treatment of poisoning from organophosphorous
insecticides or from chemical warfare 'nerve' gases and in the treatment of mushroom poisoning:
Intravenous use.
Adults:
0.5 - 2 mg atropine sulphate (5 - 20 ml), can be repeated after 5 minutes and subsequently every 10-15
minutes as required, until signs and symptoms disappear (this dose may be exceeded many times).
Paediatric population:
0.02 mg atropine sulphate/kg body weight possibly repeated several times until signs and symptoms
disappear.
Dose adjustments
In general, dosage should be adjusted according to the patient’s response and tolerance. Dosage to a total
maximum dose of 3 mg is usually increased until adverse effects become intolerable; then, a slight reduction
in dosage generally yields the maximum dosage tolerated by the patient.
Special populations
Caution is advised for patients with renal or hepatic impairment and for elderly (see section 4.4).
Method of administration
The syringes are intended for intravenous use but may be administered intramuscularly if necessary.
For instructions on use of the medical product before administration, see section 6.6.
4.3
Contraindications
-
Hypersensitivity to the active substance or to any of the excipients listed in section 6.1;
Bladder outflow obstruction (e.g. prostatic hypertrophy);
Paralytic ileus;
Severe ulcerative colitis and obstructive disease of the gastrointestinal tract;
Angle-closure glaucoma or a narrow angle between the iris and the cornea;
Acute haemorrhage with unstable cardiovascular status.
2
Contra-indications are not applicable to the use of atropine in life-threatening emergencies (e.g. asystole,
intoxications).
4.4
Special warnings and precautions for use
-
Atropine blocks vagal inhibition of the SA nodal pacemaker and should thus be used with caution in
patients with tachyarrhythmias, congestive heart failure or coronary heart disease.
Atropine should be used with caution in patients with hyperthyroidism, hepatic or renal disease or
hypertension and in patients with high temperature or fever since it reduces the ability to sweat, thus
increasing the risk of hyperthermia.
Parenterally administered atropine should be used cautiously in patients with chronic pulmonary
disease since a reduction in bronchial secretions may lead to formation of bronchial plugs.
Antimuscarinics should be used with extreme caution in patients with autonomic neuropathy.
Atropine should not be given to patients with myasthenia gravis except to reduce adverse muscarinic
effects of an anticholinesterase.
Atropine decreases gastric motility, relax the lower oesophageal sphincter and may delay gastric
emptying; it should therefore be used with caution in patients with gastric ulcer, oesophageal reflux or
hiatus hernia associated with reflux oesophagitis, diarrhoea or gastrointestinal infection.
Atropine should be used with caution in patients with ileostomy or colostomy.
During inhalation anaesthesia (especially with halothane), anticholinergics may cause cardiac
arrhythmia.
-
-
-
-
Paediatric population
Antimuscarinic agents should be used with caution in infants, children and children with spastic paralysis or
brain damage since these patients may be more susceptible to adverse effects.
Other special populations
Persons with Down's syndrome appear to have an increased susceptibility to some of the actions of atropine,
whereas those with albinism may have a reduced susceptibility.
Antimuscarinic agents should be used with caution in the elderly and a dose reduction may be necessary
since these patients may be more susceptible to adverse effects.
4.5
Interaction with other medicinal products and other forms of interaction
-
The effects of atropine may be enhanced by the concomitant administration of other medicinal agents
with anticholinergic activity e.g. tricyclic antidepressants, antispasmodics, anti-parkinsonian drugs
(e.g. amantadine), some antihistamines, phenothiazines, class Ia antiarrythmic agents (e.g.
disopyramide and quinidine), antiemetics, muscle relaxants.
Atropine may also antagonise the gastrointestinal effects of cisapride, domperidone, and
metoclopramide.
By delaying gastric emptying, atropine may alter the absorption of other drugs.
Data regarding interactions are only available for adults, it is not known if the extent of the interactions is
similar in paediatric patients as in adults.
4.6
Fertility, pregnancy and lactation
Pregnancy
Animal studies did not indicate direct or indirect harmful effects with respect to reproductive toxicity (see
section 5.3).
There are limited amount of data from the use of atropine in pregnant women. Studies of the
pharmacokinetics of atropine in mother and foetus in late pregnancy indicated that atropine rapidly crosses
the placental barrier. However, whereas peak concentrations of atropine in foetal cord blood were reached
3
about 5 minutes after intravenous doses, the maximum effect on foetal heart rate occurred after about 25
minutes. Intravenous administration of atropine during pregnancy or at term may cause tachycardia in the
foetus. As a precautionary measure, it is preferable to avoid the use of Atropin Stragen during pregnancy.
Breastfeeding
Trace amounts of atropine appear in the breast milk and may cause antimuscarinic effects in the infant;
lactation may be inhibited. Breast-feeding should be discontinued during treatment with Atropin Stragen.
4.7
Effects on ability to drive and use machines
Atropin Stragen has major influence on the ability to drive and use machines.
4.8
Undesirable effects
The pattern of adverse effects seen with atropine can mostly be related to their pharmacological actions at
muscarinic and, at high doses, nicotinic receptors. Adverse effects are dose-related and usually reversible
when therapy is discontinued. The most common effects occurring with relatively small doses are visual
disturbances, reduced bronchial secretion, dry mouth, constipation, reflux, flushing, difficulty in micturition
and dryness of the skin. Transient bradycardia may develop followed by tachycardia, with palpitations and
arrhythmias.
The evaluation of adverse reactions is based on the following definition of frequency:
Very Common: ≥1/10;
Common: ≥1/100 to <1/10;
Uncommon: ≥1/1,000 to <1/100;
Rare: ≥1/10,000 to <1/1,000;
Very rare: <1/10,000;
Not known: cannot be estimated from the available data
Frequency
Very Common
(≥1/10)
System
Organ Class
Immune system
disorders
Nervous system
disorders
Eye disorders
Cardiac
disorders
Common
(≥1/100 to
<1/10)
Uncommon
(≥1/1,000 to
<1/100)
Excitement,
incoordination,
mental confusion,
and/or
hallucinations
(especially with
higher dosages),
hyperthermia
Psychotic
reactions
Rare
(≥1/10,000
to
<1/1,000)
Very Rare
(<1/10,000)
Allergic
reactions
Seizure,
drowsiness
Anaphylaxis
Headache,
restlessness,
ataxia,
insomnia
Visual
disturbances
(mydriasis,
inhibition of
accommodation,
blurred vision,
photophobia)
Tachycardia
(arrhythmias,
transient
Atrial
arrhythmias,
ventricular
4
Not known
(cannot be
estimated
from the
available
data)
Frequency
Very Common
(≥1/10)
Common
(≥1/100 to
<1/10)
Uncommon
(≥1/1,000 to
<1/100)
Rare
(≥1/10,000
to
<1/1,000)
Very Rare
(<1/10,000)
System
Organ Class
exacerbation of
bradycardia)
Vascular
disorders
Respiratory,
thoracic and
mediastinal
disorders
Gastrointestinal
disorders
Skin and
subcutaneous
tissue disorders
Musculoskeletal
and connective
tissue disorders
Renal and
urinary disorders
Not known
(cannot be
estimated
from the
available
data)
fibrillation,
angina,
hypertensive
crisis
Flushing
Reduced
bronchial
secretion
Dryness of the
mouth
(difficulty in
swallowing and
talking, thirst),
parasympathetic
inhibition of
gastrointestinal
tract
(constipation
and reflux),
inhibition of
gastric
secretion, loss
of taste, nausea,
vomiting,
bloated feeling
Anhidrosis,
urticaria, rash
Inhibition of the
parasympathetic
control of the
urinary bladder,
urinary retention
Paediatric population
Infants, children and children with spastic paralysis or brain damage may be more susceptible to
antimuscarinic effects.
Other special populations
Atropine may cause excitement, incoordination, confusion and/or hallucinations especially in the elderly.
An epidemiological study similarly reported lower cognitive performance in elderly patients receiving
antimuscarinics.
Patients with Down syndrome may be more susceptible to antimuscarinic effects.
5
Reporting of suspected adverse reactions
Reporting suspected adverse reactions after authorisation of the medicinal product is important. It allows
continued monitoring of the benefit/risk balance of the medicinal product. Healthcare professionals are
asked to report any suspected adverse reactions via the national reporting system listed in Appendix V.
4.9
Overdose
Adults:
Toxic dose: > 10 mg atropine
Lethal dose: approx. 200 mg
Symptoms:
Marked dryness of the mouth accompanied by a burning sensation, difficulty in swallowing, pronounced
photophobia, mydriasis, flushing and dryness of the skin, raised body temperature, rash, nausea, vomiting,
tachycardia and hypertension. Restlessness, tremor, confusion, excitement, hallucinations and delirium may
result from CNS stimulation; this is followed by increasing drowsiness, stupor and general central
depression terminating in death from circulatory and respiratory failure.
Treatment:
Treatment of acute overdose consists of symptomatic and supportive therapy. In severe cases,
physostigmine, 1 to 2 mg, should be slowly administered intravenously, the dose may be repeated if
necessary since it is rapidly eliminated from the body. Diazepam may be administered for sedation of the
delirious patient but the risk of central depression occurring late in the course of atropine poisoning
contraindicates large doses of sedative. An adequate airway should be maintained and respiratory failure
may be treated with oxygen and carbon dioxide inhalation. Fever is reduced by the application of cold packs
or sponging with tepid water. Adequate fluid intake is important. Urethral catheterisation may be necessary.
If photophobia is present or likely, the patient should be nursed in a darkened room.
Paediatric population
Small children:
Lethal dose: > 10 mg atropine
Treatment of acute overdose consists of symptomatic and supportive therapy. In severe cases,
physostigmine, 0.02- 0.04 mg/kg body weight, should be slowly administered intravenously, the dose may
be repeated if necessary since it is rapidly eliminated from the body. Diazepam may be administered for
sedation of the delirious patient but the risk of central depression occurring late in the course of atropine
poisoning contraindicates large doses of sedative. An adequate airway should be maintained and respiratory
failure may be treated with oxygen and carbon dioxide inhalation. Fever is reduced by the application of
cold packs or sponging with tepid water. Adequate fluid intake is important. Urethral catheterisation may be
necessary. If photophobia is present or likely, the patient should be nursed in a darkened room.
5.
PHARMACOLOGICAL PROPERTIES
5.1
Pharmacodynamic properties
Pharmacotherapeutic group: Belladonna and derivatives, ATC code: A03BA01
Mechanism of action
Atropine is an antimuscarinic agent which competitively antagonises acetylcholine at postganglionic nerve
endings, thus affecting receptors of the exocrine glands, smooth muscle, cardiac muscle and the central
nervous system. It has peripheral and central actions, although it has almost no detectable effect on the CNS
in doses that are used clinically.
Pharmacodynamic effects
6
Peripheral effects include tachycardia, decreased production of saliva, sweat, bronchial, nasal, lachrymal
and gastric secretions, decreased intestinal motility and inhibition of micturition.
Atropine increases sinus rate and sinoatrial and AV conduction. Usually heart rate is increased but there
may be an initial bradycardia.
Atropine inhibits secretions throughout the respiratory tract and relaxes bronchial smooth muscle producing
bronchodilatation.
Paediatric population and elderly patients
Children, particularly those younger than two years, and elderly patients may be more susceptible to the
actions of atropine.
5.2
Pharmacokinetic properties
Absorption:
Peak plasma concentrations of atropine after intramuscular administration are reached after approximately
30-60 minutes.
Distribution:
The volume of distribution is approximately 2-3 L/kg and less than 50% of the dose is bound to plasma
proteins.
Biotransformation:
Atropine is metabolised by the microsomal mono-oxygenase enzymes and atropine esterase to four major
metabolites. Following i.v. administration of atropine sulfate approximately 50% will be metabolised, while
approximately 30-50% of the administered dose is excreted as unchanged atropine.
Elimination:
The elimination half life is about 2 to 4 hours. About 30 to 50% of the dose is excreted in the urine as
unchanged drug.
Paediatric population
The elimination half-life of atropine is more than doubled in children less than two years compared to
adults.
Elderly
The elimination half-life of atropine is more than doubled in the elderly (>65 years old) compared to adults.
5.3
Preclinical safety data
Effects in non-clinical studies were observed only at exposures considered sufficiently in excess of the
maximum human exposure indicating little relevance to clinical use.
6.
PHARMACEUTICAL PARTICULARS
6.1
List of excipients
Sodium chloride
Concentrated hydrochloric acid (for pH adjustment)
Water for injections
6.2
Incompatibilities
In the absence of compatibility studies, this medicinal product must not be mixed with other medicinal
products.
7
6.3
Shelf life
3 years.
After opening: the product must be used immediately.
6.4
Precautions for storage
This medicinal product does not require any special storage conditions.
6.5
Nature and contents of container
5 ml polypropylene pre-filled syringe with a polypropylene tip cap; sterile outer surface; individually
packaged in a transparent blister pack; in box of 10.
6.6
Special precautions for disposal and other handling
Instructions for use:
Be careful to strictly respect the protocol for the use of the syringe.
The pre-filled syringe is for single patient only. Discard syringe after use. DO NOT REUSE.
The content of un-opened and un-damaged blister is sterile, and must not be opened until used.
The product should be inspected visually for particles and discoloration prior to administration. Only clear
colourless solution free from particles or precipitates should be used.
The product should not be used if the tamper evident seal on syringe is broken.
Using aseptic technique, Atropin Stragen 0.1 mg/ml, Solution for injection in pre-filled syringe can be used
on a sterile field.
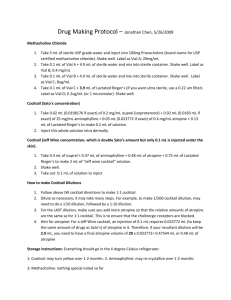
1.
Before opening the syringe, push firmly the piston rod in
order to break open the syringe plunger.
2.
Twist off the tip cap to break the frangible obturator.
8
3.
Check that the sealing cap has been completely removed.
4.
Purge the air of the syringe by pushing the piston slightly.
5.
Connect the syringe to the IV access.
Push the piston carefully to inject the required volume.
Any unused medicinal product or waste material should be disposed of in accordance with local
requirements. This medicinal product must not be mixed with other medicinal products
7.
MARKETING AUTHORISATION HOLDER
<[To be completed nationally]>
{Name and address}
<{tel}>
<{fax}>
<{e-mail}>
8.
MARKETING AUTHORISATION NUMBER(S)
<[To be completed nationally]>
9.
DATE OF FIRST AUTHORISATION/RENEWAL OF THE AUTHORISATION
Date of first authorisation: 2012-03-14
<Date of latest renewal: {DD month YYYY}>
<[To be completed nationally]>
10.
DATE OF REVISION OF THE TEXT
2015-05-21
9