1- Mucous cells
advertisement
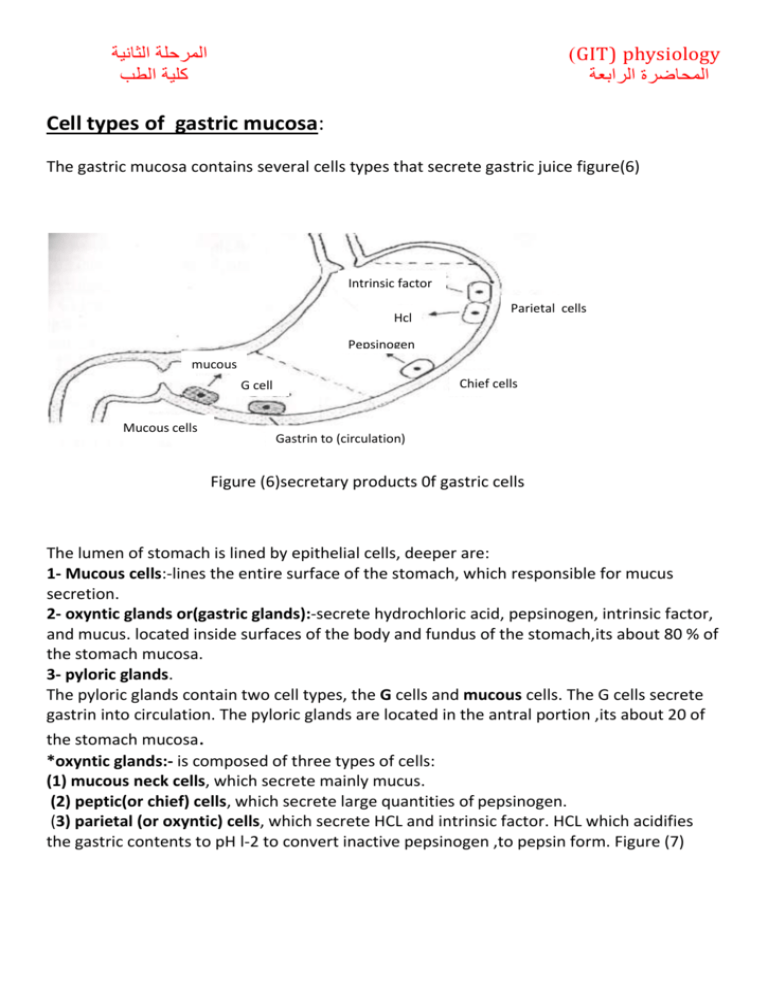
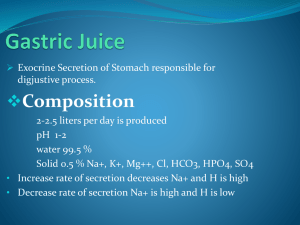
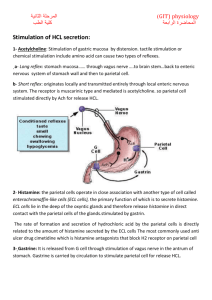
) GIT) physiology المحاضرة الرابعة المرحلة الثانية كلية الطب Cell types of gastric mucosa: The gastric mucosa contains several cells types that secrete gastric juice figure(6) Intrinsic factor Hcl Parietal cells Pepsinogen mucous Chief cells G cell Mucous cells Gastrin to (circulation) Figure (6)secretary products 0f gastric cells The lumen of stomach is lined by epithelial cells, deeper are: 1- Mucous cells:-lines the entire surface of the stomach, which responsible for mucus secretion. 2- oxyntic glands or(gastric glands):-secrete hydrochloric acid, pepsinogen, intrinsic factor, and mucus. located inside surfaces of the body and fundus of the stomach,its about 80 % of the stomach mucosa. 3- pyloric glands. The pyloric glands contain two cell types, the G cells and mucous cells. The G cells secrete gastrin into circulation. The pyloric glands are located in the antral portion ,its about 20 of the stomach mucosa. *oxyntic glands:- is composed of three types of cells: (1) mucous neck cells, which secrete mainly mucus. (2) peptic(or chief) cells, which secrete large quantities of pepsinogen. (3) parietal (or oxyntic) cells, which secrete HCL and intrinsic factor. HCL which acidifies the gastric contents to pH l-2 to convert inactive pepsinogen ,to pepsin form. Figure (7) Figure (7)types of cells in the gastric mucosa Function of HCL: 1-HCL participates in break down of protein. 2- It provides an optimal pH for convert an active pepsinogen to active pepsin. 3- It hinders the growth of pathogenic bacteria. Mechanism of HCI secretion: HCL is secreted by the following steps: 1- CL- ions is transported by active transport into the canaliculus. The flow of CL- create a negative potential inside the canaliculi, causing K+ to flow passively into the canaliculus. 2- H+ ion is then exchanged for K+ ion by H+-K+ ATPase pump. The source of H+ ion is from the dissociation of carbonic acid (H2C03) into H+ + HCO3- (CO2+ H2O = H2C03). H+ react with CL_ to form HCL, HC03- diffuse back to plasma. After meal sufficient H+ ions may be secreted. 3- Water enter canaliculus down the osmotic gradient created by movement of the HCL into the canaliculus. Figure (8) HCL secreted Figure (8) gastric parietal cell Substances affecting HCL secretion: A- Stimulation of HCL secretion: 1- Acetylcholine: Stimulation of gastric mucous by distension, tactile stimulation and chemical stimulation include amino acid. This stimulation can cause two types of reflexes. a- Long reflex: stomach mucosa vagus nerve system of stomach wall and then to brain stem enteric nervous parietal cell. b- Short reflex: originates locally and transmitted entirely through local enteric nervous system. The receptor is muscarinic type and mediated is acetylcholine. so parietal cell stimulated directly by Ach for release HCL. 2- Histamine: the parietal cells operate in close association with another type of cell called enterochromaffin-like cells (ECL cells) stimulated by gastrin, the primary function of which is to secrete histamine. The ECL cells lie in the deep of the oxyntic glands and therefore release histamine in direct contact with the parietal cells of the glands. The rate of formation and secretion of hydrochloric acid by the parietal cells is directly related to the amount of histamine secreted by the ECL cells.. The most commonly used anti ulcer drug cimetidine which is histamine antagonists that block H2 receptor on parietal cell. 3- Gastrin: It is released from G cell through stimulation of vagus nerve in distal stomach. Gastrin is carried by circulation to stimulate parietal cell for release HCL. B-Inhibition of HCL : Somatostatin inhibits HCL secretion by parietal cell and gastrin secretion by G cell. Somatostatin is released from interneurons within the enteric nervous system. gastric HCL secretion:is divided into three phases; cephalic, gastric and intestinal. The cephalic and gastric phases are illustrated in Figure (8). 1- Cephalic phase: 30% of total HCL secreted in response to meal. The stimuli for HCL secretion in this phase are smelling, tasting, chewing, swallowing and conditioned reflexes. Two mechanisms promote HCL secretion in this phase. First is direct stimulation of the parietal cell by vagus nerves, which release Ach. Second is indirect stimulation of the parietal cells by gastrin. Indirect path vagus nerve release, at G cells stimulating gastrin secretion, gastrin enters the circulation and stimulate the parietal cells. 2- Gastric phase: 60% of total HCL secreted in response to meal. The stimuli are distension of stomach and presence of breakdown products of protein; amino acid and small peptides. Four physiological mechanism are involved. First two mechanisms which are initiated by distension of the stomach. Distension causes direct vagus stimulation of the parietal cells and indirect stimulation of the parietal cells via gastrin release. The third mechanism is initiated by distension of the stomach antrum and local reflex which stimulate gastrin release. Fourth mechanism direct effect of amino acid and small peptides like GRP(gastric releasing polypeptides) to stimulate gastrin release. Alcohol and caffeine also stimulate gastric HCL secretion . GRP )) Figure (8) Cephalic and gastric 3- Intestinal phase: Itphase is only 10% of HCI secretion. It is mediated by products of protein digestion. Peptic ulcer and gastric barrier: A peptic ulcer is an excoriated area of stomach or intestinal mucosa caused principally by the digestive action of gastric juice or upper small intestinal secretion. peptic ulceration is an imbalance between the rate of secretion of gastric juice and the degree of protection by mucous which secrete along GIT and the alkalinity Secretion of the small intestinal(bicarbonate secretion) it caused by: 1- Breakdown of the barrier in which (the Stomach is lined with highly resistant mucous cells that secrete a viscid and alkaline adherent mucus. And the adjacent epithelial cells has tight junction between the gastric barrier prevent the stomach from auto digestion and irritation by gastric secretion or by infection with a bacterium ( Helico bacteria pylori ), disrupts this barrier, as do aspirin and other nonsteroidal anti-inflammatory drugs (NSAIDs), which inhibit the production of prostaglandins and consequently decrease mucus and HCO3 –secretion. The NSAIDs are widely used to combat pain and treat arthritis. 2- Prolonged excess secretion of acid:two feedback control mechanisms that neutralization of gastric juices: A- When excess acid enters the duodenum, it reflexly inhibits gastric secretion and peristalsis in the stomach, both by nervous reflexes and by hormonal feedback from the duodenum, thereby decreasing the rate of gastric emptying. B- The presence of acid in the small intestine liberates secretin from the intestinal mucosa, which then passes by way of the blood to the pancreas to promote rapid secretion of pancreatic juice. This juice also contains a high concentration of sodium bicarbonate, for neutralization of the acid . Gastric and duodenal ulcers can be given a chance to heal by inhibition of acid secretion with drugs that block the H2 histamine receptors on parietal cells or drugs that inhibit H+– K+ ATPase. Bacteria can be eradicated with antibiotics, and NSAID-induced ulcers can be treated by stopping the NSAID. peptic ulcers most frequently occur, In a few centimeters of the pylorus ,and along the lesser curvature of the antral end of the stomach or, more rarely, in the lower end of the esophagus where stomach juices frequently reflux.