Pharmacology Objectives 15 - U
advertisement

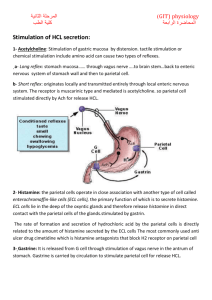
Pharmacology Lecture 15 Gastrointestinal Drugs 1) Explain the mechanism of acid production by the parietal cells. a) Neural stimulation - the dorsal motor nucleus of the vagal nerve (DMNV) sends fibers to the stomach via the vagus nerve to synapse with ganglion cells of the enteric nervous system (ENS). Acetylcholine release from postganglionic vagal fibers can directly stimulate gastric acid secretion via muscarinic receptors on parietal cells. b) Endocrine stimulation - gastrin released from antral G cells. c) Paracrine stimulation - local release of histamine from enterochromaffin-like (ECL) cells or mast cells. The histamine in turn activates parietal cell H2 receptors that are linked to stimulation of adenylyl cyclase, causing activation of the cAMP pathway. Gastrin and muscarinic stimuli may also act directly on the parietal cell to activate calcium sensitive pathways either method stimulates activation of H+, K+-ATPase on parietal cells with the consequent secretion of H+ at rates between 20 and 40 mEq per hour. 2) Identify the role of H. pylori in peptic ulcer disease. H. pylori is a spiral shaped, flagellated, gram-negative bacteria which is a member of a new genus, Helicobacter. They usually live in the stomach where the flagella allow motility in the gastric juice and gastric mucus. They require urease enzyme to colonize the mucus layer because it breaks down the urea in the gastric juice and generates enough bicarbonate and ammonium ion to allow H. pylori safe passage through the gastric acid to the mucus layer where it attaches to phospholipids and Louis B. antigens and delivers soluble protease is in phospholipase which is harmful to the integrity of the mucus layer and the underlying cells. The host reaction exacerbates disease but is ineffective in eradicating the H. pylori. 3) List the approaches used to diagnose H. pylori infection. Approaches include histology and culture at endoscopy (the most sensitive method), a rapid urease (CLO test), serology tests (simplest and most widely available), and breath tests for detection of the urease enzyme of H. pylori. 4) List the approaches used to eradicate H. pylori. a) Omeprazole (Prilosec®, proton pump inhibitor) 20 mg, b.i.d. and amoxicillin 1 g, b.i.d. for 7 to 14 days with a cost of about $130 and a cure rate of about 80% with little side effects. b) "Triple therapy" consists of administration of bismuth subsalicylate tablets (PeptoBismol®) four times daily, tetracycline (500 mg, q.i.d.) and metronidazole (250 mg, q.i.d.) With the cost of about $42 for a course of therapy and a cure rate of about 85 to 90%. c) "MOC therapy" b.i.d. administration of: metronidazole 500 mg, omeprazole 20 mg and clarithromycin 250 mg each for one week with 90% effectiveness. 5) Explain the role of the proton pump in secretion of acid. Secretion of H+ into the lumen results from activity of parietal cell H+, K+-ATPase. The proton pump, H+, K+ATPase, can be activated by acetylcholine at muscarinic receptors, histamine at H2 receptors, and gastrin at gastrin receptors. 6) Define the mechanism of action of the proton-pump inhibitors. Inhibition of the H+, K+-ATPase, proton pump, produces the most effective mechanism known to inhibit gastric acid secretion. Omeprazole (Prilosec®) and esomeprazole (Nexium®) are both H+, K+-ATPase inhibitors. 7) Localize the distribution of histamine receptor types. The H2 histamine receptor occurs on the parietal cell in mediates the stimulatory effect of histamine on acid secretion by parietal cells. H1 histamine receptors mediate a variety of histamine actions on blood vessels, sensory nerves, bronchial smooth muscle and other cells. 8) Compare and contrast H2 receptor antagonists to other peptic ulcer medications. Medication Proton pump inhibitors Omeprazole and esomeprazole H2 receptor antagonists cimetidine, famotidine, nizatidine, and ranitidine Anti-cholinergics Atropine or scopolamine Prostaglandins Misoprostol Action Inhibits H+, K+-ATPase Reduces gastric acid Blocks parietal cell H2 histamine receptors Decreases acid-pepsin secretion Blocks muscarinic cholinergic receptors Decreases acid secretion Inhibit adenylate cyclase stimulation by histamine Cytoprotective effects Side Effects Omeprazole - gastric hyperplasia in animals Cimetidine - interferes with cytochrome P450, binds testosterone, causes confusion Dry mouth, urinary retention, constipation Diarrhea, uterine stimulation (especially during pregnancy) Histamine is thought to stimulate adenylate cyclase in parietal cells, forming cAMP, which acts through a protein kinase to activate the proton pump that secretes H+ into the lumen. H2 receptor antagonists, cimetidine, famotidine, nizatidine, and ranitidine, decrease acid and pepsin secretion by blocking parietal cell H2 histamine receptors to allow the healing of ulcers in the mucosa. 9) Classify antacids as far as the side effects are concerned. (See question 10) Systemic antacids - are absorbed into the bloodstream, can increase blood pH, and alkalinize the urine. Nonsystemic antacids - do not alter blood pH and do not alkalinize the urine. 10) Compare relative onset of action and effect on stool of different antacids. Antacids Sodium and potassium salts Onset of action Almost immediate (pH of 5-7) short duration Calcium salts Very rapid (pH of 4-5) remains high until stomach is emptied Slow onset, maintains desirable levels until stomach is emptied Magnesium and aluminum salts Magnesium hydroxide (milk of Magnesia) Rapid onset (pH of 8-9) Side effects (stool) React with bicarbonate and carbonate secreted in the pancreatic juice to form salts (excreted in the feces) React with fatty acids to form soaps (also excreted) Promotes gastrin and acid secretion "acid rebound" can produce systemic hypercalcemia with formation of caluli "milk alkali syndrome" Magnesium is (laxative), can induce muscle weakness and fatigue Aluminum is (constipating), can bind phosphate leading to phosphate deficiency, muscle weakness, and bone resorption Magnesium is (laxative) 11) What are the two types of GI contractions & identify the mechanism of prokinetic agents. The two types of GI contractions are: peristalsis (propulsion) and segmentation contractions (mixing). Metoclopramide and related prokinetic drugs are known to possess antagonist activity at 5-hydroxytryptamine 5-HT3 receptors and agonist activity at 5-HT4 receptors. Metoclopramide also possesses dopamine receptor antagonist properties, which account for its antiemetic activity. The precise mechanism for increase of GI contractions is not known, but may be related to increased release of acetylcholine at the terminals of cholinergic neurons animating the GI smooth muscle, release of acetylcholine at interneurons in the myenteric plexus, or even by blockade or stimulation of certain types of 5-HT receptors. Cisapride (Propulsid®) was withdrawn from the market as a prokinetic agent due to cardiac arrhythmias. Tegaerod maleate (Zelnorm®) is a new 5-HT receptor agonists approved for short-term treatment of women with irritable bowel syndrome. 12) Identify the mechanism of action of laxative substances. Category Secretary Sailing Emollient Bulk forming Example Castor oil, Ex-Lax (Senna), bisacodyl Magnesium hydroxide, sodium phosphate or sulfate Dioctyl sodium sulfocuccinate, mineral oil Bran, methylcellulose, psyllium Action Stimulate secretion by activating adenylate cyclase in crypt cells which increases cAMP to activate chloride channels Decreases viscosity by retaining fluid in the lumen and promoting flow through the bowel (often explosive) Decreases viscosity by acting as an autumn Zorba lubricant Increases bulk by hydrating non-digestible cellulose fibers 13) Describe the mechanism of antidiarrheal effect of opioids. In humans, opioids increase segmenting contractions of the small and large intestines, thereby increasing resistance to flow through the lumen, and promote mucosal absorption of fluid and electrolytes. This allows for slowed transit through the gut and more complete fluid absorption resulting in increased viscosity of luminal content and formed stools. 14) Identify conditions where use of opioids for antidiarrheal actions is inappropriate. Morphine, codeine, and related agents can be used orally or by injection as antidiarrheal drugs. However, the natural opioids possess abuse potential and in overdose can have dangerous side effects. Opioid antidiarrheals should not be employed in the systematic treatment of diarrhea induced by enteric infections with invasive organisms, especially species out of Shigella and Salmonella. Diarrhea in these infections may be protective and help to flush organisms from the gut; the delay in transit of gut contents induced by opioids can exacerbate the infection. Drugs Opioids α2 agonists Anticholinergics Somatostatin (octreotide) Bismuth subsalicylate Cholestyramine Inhibit propulsive contractions +++ Stimulate nonpropulsive contractions +++ Enhance fluid absorption Decrease fluid secretion ++ + +++ +++ +++ ++ + +++ Bind luminal secretagogues +++ +++