Gastric Secretion
advertisement

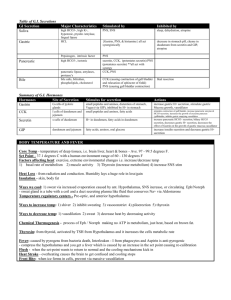
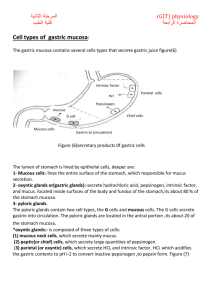
Gastric Secretion Logo OBJECTIVES Describe the three types of gastric exocrine secretory cells and their secretions. Summarize the mechanism of HCl secretion. Explain the role of HCl and pepsinogen in digestion. Emphasize the protective role of mucus and its applied importance. Describe the multiple regulatory pathways that control stomach secretion. Appreciate absorption. the role of stomach in digestion and GASTRIC SECRETION Gastric Secretion is about 2 liters per day. There are Gastric Glands present in stomach. They lie at the base of ‘Gastric Pits’. Gastric Glands have exocrine & endocrine cells. Two distinct areas of gastric mucosa that secrete gastric juice: 1- Oxyntic mucosa: Lines body & fundus. 2- Pyloric gland area (PGA): Lines antrum. Exocrine Cells in Gastric Gland 1. Mucus Cells: Secrete thin watery mucus. 2. Chief Cells: Secrete enzyme precursor pepsinogen. Chief cells are present in oxyntic mucosa (fundus and body). 3. Parietal [=Oxyntic cells]: Secrete HCL and intrinsic factor. They are present in fundus and body. Therefore, pH in stomach lumen is below 2. Mechanism of HCL Secretion Hydrogen [H+] is actively transported in parietal cell membrane, from cell to the lumen. Chloride [Cl-] is secreted by secondary active transport mechanism. FUNCTIONS OF GASTRIC JUICE 1- Functions of HCL: 1) Digestion of protein by activation of Pepsinogen into pepsin & give optimum pH of its effect & hydrolysis of protein. 2) Sterilization by acidity. It kills microorganisms ingested with food. 3) Absorption of iron (by converting ferric into ferrous) & calcium (by prevention of calcium salts precipitation). 4) When HCl enters duodenum secretin hormone bile & pancreatic secretion. 2- Secretion of Enzymes: 1- Pepsinogens: • Secreted by chief cells & Optimum pH = 1 – 3. • Inactive pepsinogen active pepsin (by HCl & auto activation). • Pepsin initiates protein digestion. 2- Gelatinase: which liquefies gelatin. 3- Gastric lipase: acts on short chain fat. Its optimum pH = 3. 4- Rennin: milk clotting enzyme (not present in human). 3- Function of Intrinsic Factor: It is secreted by parietal cells. It is essential for absorption of vitamin B12 [vitamin B12 is only absorbed when in combination with intrinsic factor]. Intrinsic factor – vitamin B12 complex have special receptors in terminal ileum, where vitamin B12 is absorbed. Vitamin B12 is essential for Maturation of RBCs & Myelination of nerves. If no intrinsic factor (either in deficiency of intrinsic factor or gastrectomy), vitamin B12 is not absorbed, it causes pernicious anemia. 4- Functions of Mucus: Surface of gastric mucosa is covered by mucus. It is derived from surface epithelial cells and mucous cells. Mucus works as a protective barrier. It protects stomach wall from self-digestion by pepsin. As mucus is alkaline (pH=7), it protects stomach from HCL [pH=2]. Lubricating: protection from mechanical injury. Stomach Is Protected From Acidity & Pepsin, How? Gastric mucosal barrier is protected by: 1) Insoluble thick alkaline mucus (HCO3-). 2) Tight junctions between mucosal cells to prevent passing HCl in between. 3) Mucosal cells are impermeable to H+ pumped to the lumen. 4) Entire stomach lining is replaced every 3 days. 5- Gastrin secretion: Gastrin is a major GIT hormone. It is released from G-cells in pyloric antrum. It is secreted in response to protein products in lumen of stomach and in response to ACh. It is the main factor increasing HCL during meal digestion. Gastrin is carried by blood to the fundus and body of the stomach and then stimulates parietal & chief cells, therefore, causes secretion of HCL and pepsinogen. Gastrin stimulates Entero Chromaffin Like Cells (ECLC) to release histamine and increase HCL secretion. It causes growth of mucosa of stomach & small intestine. Endocrine & Paracrine Cells in Gastric Glands 1) G-cells: secrete Gastrin (antrum). 2) ECLC (Entero Chromaffin Like Cells): secrete Histamine (Fundus and body ) 3) D-cells: secrete Somatostatin (pyloric antrum & duodenum). Gastrin, Histamine & Acetylcholine [ACh] stimulate parietal cells to secrete HCL. Somatostatin inhabits HCL secretion. ACh & Gastrin increase pepsinogen by acting on chief cells. FACTORS AFFECTING H+ SECRETION N.B. Alcohol & caffein stimulate HCl secretion Gastric juice is increased before food reaches stomach. Stimuli: thinking, smelling, tasting, chewing and swallowing vagal nerve activity. Vagus stimulates intrinsic plexus increases ACh secretion which increases HCL and pepsinogen. Vagus stimulates G-cells release of gastrin which increases HCL and pepsinogen. 2- GASTRIC PHASE (75 %): • Presence of food in stomach as protein, caffeine, alcohol & by distension gastric secretion by: 1- Local nerve plexus. 2- Vagus. 3- Gastrin secretion from G-cells. N.B. Protein is most potent stimulus. It acts via local plexus, vagus and stimulates gastrin release. N.B. People with hyper-acidity or peptic ulcer should avoid caffeine and alcohol. 3- INTESTINAL PHASE (inhibitory): •The presence of food in duodenum gastric secretion. •This inhibition occurs by nervous & hormonal mechanisms. 1- NERVOUS mech. (=ENTEROGASTRIC REFLEX): •Stimulus: presence of acid, fats or hyperosmotic solution in duodenum or distention of duodenum. •Response: inhibition of gastric secretion and motility. •Center: local or vago – vagal reflex. •Importance of enterogastric reflex: •Protection of duodenum from over distention by delay emptying. •Protection of duodenum from hyperacidity (till neutralized by alkaline duodenal secretion). •Insure Protein digestion. 2- HORMONAL mech. (=ENTEROGASTRONE HORMONES): •Stimulus: presence of fats and fatty acids in duodenum. •Response: release of Cholycystokinin (CCK), Secretin, Gastric Inhibitory Peptide (GIP) & Vaso Active Inhibitory Peptide (VIP) from duodenum inhibition of gastric secretion and motility for complete digestion of fat. How Gastric Secretion Decreases After It Is Produced? It decreases by three ways: i). As a meal gradually leaves the stomach, major stimulus that is protein in stomach is withdrawn. ii). Somatostatin is released when food goes to duodenum. It has an inhibitory effect. iii). Stimuli which inhibit gastric motility are fat, acid, hypertonicity or distension in the duodenum. DIGESTION & ABSORPTION IN STOMACH Protein digestion begins in the antrum of stomach, where food is mixed with HCL and pepsin. Carbohydrate digestion which started in mouth due to action of salivary amylase, continues in the stomach, till amylase is destroyed by the HCL. Stomach absorbs alcohol and aspirin. Alcohol is lipid soluble, therefore, can diffuse through lipid membrane of epithelial cells lining stomach. Alcohol is absorbed more rapidly in small intestine. Peptic Ulcer Sites: Ulcer or erosion in the stomach, duodenum or esophagus can occur due to increased acidity and pepsin. Causes: 1- ‘Helicobacter pylori’ bacterium that causes peptic ulcer by toxins which cause gastritis & weakening gastric mucosal barrier. 2- Ethyl alcohol. 3- NSAIDS [Non Steroidal Anti-Inflammatory Drugs] e.g. Aspirin, Ibuprofen [used for arthritis, pain]. 4- Stress: probably by increased gastric secretion. TREATEMENT FOR PEPTIC ULCER 1) Anta-acids. 2) H2 Histamine receptor Blockers e.g. Cimetidine & Ranitidine. 3) Proton pump Blockers (it blocks H+ - K+ ATP pump) e.g. Omeprazole. 4) Antibiotics for H.Pylori. تاج األدعية (ربنا آتنا في الدنيا حسنة وفي اآلخرة حسنة وقنا عذاب النار).