Autoimmunity Summary
advertisement

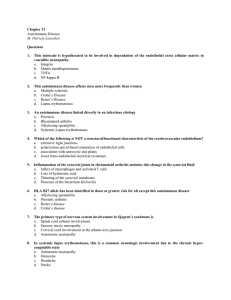
Disease Description Signs and Symptoms Tests Treatment Sjögren's syndrome - Associated with the HLA-DR3 gene. - This is essentially an autoimmune reaction against the bodies exocrine glands, specifically the salivary and lacrimal glands. This leads to dry mouth (xerostomia), eye problems (xeropthalmia) and lymphocytic infiltration of the glands. It eventually destroys the glands. - There are two types, primary and secondary. Primary presents as only sjogren’s, without any other disorders. Associated with the HLA-DR4 gene. 860/100,000 people affected. RhF is an autoantibody against igG. Dry eyes, dry mouth, vaginal dryness, lack of mucous production. - Blood tests for anti-nuclear antibody (ANA) and rheumatoid factor (because SS frequently occurs secondary to rheumatoid arthritis). - Typical Sjögren's syndrome ANA patterns are SSA/Ro and SSB/La, (SSB/La is far more specific; SSA/Ro is associated with numerous other autoimmune conditions but often present in Sjögren's). - Schirmer's test measures the production of tears: a strip of filter paper is held inside the lower eyelid for five minutes, and its wetness is then measured with a ruler. <5ml of liquid = Sjögren's syndrome. Artificial tears, punctal plugs into lacrimal ducts mouth care, regular sips of fluid, artificial saliva topical cyclosporine or other DMDs awareness of lymphoma risk - Initially joint inflammation - Progresses to damage to joints. - Inflammation, pain, deformity - Mall joints affected (e.g. MCP and PIP joints), but large joints can be affected. - Worse in the morning / before exercise, improves with movement during the day. - There may be extra-articular features (about 20% of cases). These include fever, weight loss, malaise, nodules, vasculitis, anaemia, atlantoaxial subluxation and others. - Can be associated with Sjögren's syndrome - FBC : anaemia (chronic disease / haemolytic) - ESR : raised - CRP : moderately raised - RhF : raised in ~70% of cases (but also some healthy people) - Anti-citrullinated protein antibodies - Anti-cyclic citrillunated peptides - Anti-mutated citrullinate vimentin assay - US, MR or isotope bone scans (early changes) - Radiographs of hands & feet (later changes) : - soft tissue swelling, juxta-articular osteopenia, joint space narrowing → periarticular erosions, subluxation, deformity - Steroids - NSAIDs - DMDs : methotrexate = antiproliferative (against folate activity), azathioprine = antiproliferative (against purine synthesis), sulphasalazine = suppressive (against IL-1 & TNF), penicillamine = suppressive (against MΦs, T cells, IL-1) - Gold injections = uncertain mechanism - mAbs : infliximab = anti-TNF cytokine, rituximab = antiCD20 on B lymphocytes Rheumatoid Arthritis Graves’ Disease The most common autoimmune disorder (1152 per 100,000), but more common in women (2% of all women will get Grave’s disease). Caused by autoantibody IgG against the TSH receptor. All the signs and symptoms of hyperthyroidism, including goitre, exophthalmos (in 40% of cases, as they have autoantibodies against the ophthalmic muscles) and pre-tibial myxoedema. - TSH = low - T3 & T4 = high - anti-TSH receptor antibodies (TSHR-Ab) - radio-iodine scans or thyroid biopsy = rarely necessary - beta-blocker (eg. propanolol) - anti-thyroid drugs (eg. carbimazole, propylthiouracil) - radio-active iodine treatment (131I) - thyroidectomy (partial) organ-specific disease with “indirect” treatments available ∴ systemic immunosuppression not justified Hashimoto’s Thyroiditis An autoimmune condition in which the thyroid itself is attacked, resulting in hypothyroidism with possible bouts of hyperthyroid symptoms. - Hashimoto's thyroiditis is All the signs and symptoms of hypothyroidism. Possible bouts of hyperthyroid symptoms. - Various autoantibodies may be present - Low blood pressure - Possible Addisonian crisis - Hyperpigmentation - Low steroid levels even after an ACTH stimulation test. interferon omega; transglutaminase; aromatic acid carboxylase; GAD; HAI; 17 hydroxylase; 21 hydroxylase against thyroid peroxidase, thyroglobulin and TSH receptors, although a small percentage of patients may have none of these antibodies present. - On gross examination, there is often presentation of a hard goitre that is not painful to the touch Simply take T4 replacement (levothyroxine) often misdiagnosed as depression, PMS, chronic fatigue syndrome, fibromyalgia and, less frequently, as ED or an anxiety disorder. Addison’s disease Chronic underproduction of steroid hormones by the adrenal glands. Sometimes (but not always) due to an autoimmune problem. Autoimmune adrenalitis is the most common cause of Addison's disease in the industrialised world. Autoimmune destruction of the adrenal cortex is caused Oral hydrocortisone to replace the steroid hormones. Replacement for other steroids if needed. Systemic Lupus Erythematosus by an immune reaction against the enzyme 21-hydroxylase - Associated with the HLA-DR2 and 3 genes. - SLE most often harms the heart, joints, skin, lungs, blood vessels, liver, kidneys, and nervous system. The course of the disease is unpredictable, with periods of illness (called flares) alternating with remissions. - SLE occurs 9 times more often in women than in men. - It is both a type 2 and a type 3 hypersensitivity reaction - The main cause of death is from cardiovascular disease due to accelerated atherosclerosis. - The most common presenting symptom is joint pain, followed by butterfly rash. - Ulcers - Stillbirth / miscarriage - Photosensitivity of the skin - Chest pain when taking a deep breath - Fatigue - Fever with no other cause - General discomfort, uneasiness, or ill feeling (malaise) - Hair loss - Mouth sores - Sensitivity to sunlight - Skin rash - a "butterfly" rash in about half people with SLE. - Swollen lymph nodes - Anti-nuclear autoantibodies, specifically autoantibodies to double stranded DNA. These are 70% specific for SLE. - You may also get anti Ro and anti La forms of anti-nuclear antibodies. - Treated mainly with immunosuppression - Cyclophosphamide, corticosteroids and other immunosuppressant’s. - The treatment of SLE involves preventing flares and reducing their severity and duration when they occur. - DMD’s used to reduce the frequency and duration of flares include methotrexate and azathioprine. - Recently a new drug for the treatment of SLE has become available, belimumab. Coeliac disease Crohn’s disease - Coeliac disease is an autoimmune disorder of the small intestine that occurs in genetically predisposed people of all ages from infancy onward. - Can be screened for, so a lot of people are diagnosed while asymptomatic. - It is thought to affect 1% of the population in the UK. - It is caused by an immune reaction to gliadin, a protein found in wheat and other common grains. This protein is modified by an enzyme (tissue transglutaminase), and the immune system then cross reacts with the small bowel tissue, causing inflammation. - NOTE: this is different from a wheat allergy! - Linked with the HLA-DQ2 allele. - The aetiology of Crohn’s disease is not well understood. It is known to be an immune disorder, but it is theorised that the immune reaction is against the gut flora, and the damage to the gut itself is an unfortunate side effect. - It may not be classified as an autoimmune disorder as the reaction is triggered by non self-antigens (theoretically), - Pain and discomfort in the digestive tract. - Chronic constipation and diarrhoea - Failure to thrive - Anaemia - Malabsorption - Steatorrhoea - Weight loss - Anti-gliadin & anti-endomysial autoantibodies - Anti-transglutaminase antibodies to the enzyme tissue transglutaminase (tTG) are found in an overwhelming majority of cases, and this is the most common test for coeliac disease. - The gold standard test is a small bowel biopsy, and this is usually done for everyone with a positive serological test. Gluten free diet is the only long term treatment, and symptoms should begin to improve following the start of a gluten fre diet. It can take up to a year for the bowel to recover, so patients may still be symptomatic during this time. If a patient does not improve on a gluten free diet (possibly because they do not stick to the diet, or because the intestine is so badly damaged that it cannot heal properly), then the patient may be given immunosuppressants such as azathioprine. Patchy, cobblestone appearance to the GIT mucosa due to transluminal skip lesions. - The patient may present with abdominal pain, diarrhoea (may be bloody), vomiting and weight loss. - The gold standard test is colonoscopy and a biopsy analysis. - Under a microscope, biopsies of the affected colon may show mucosal inflammation, characterized by focal infiltration of neutrophils, a type of inflammatory cell, into the epithelium. This typically occurs in the area overlying lymphoid aggregates. These neutrophils, along with mononuclear cells, may infiltrate the crypts, leading to inflammation (crypititis) or abscess (crypt abscess). Granulomas, aggregates of - There is no cure for Crohn’s disease, and remission may not be possible. - Smoking is BAD FOR CROHN’S DISEASE! Stopping smoking is one of the best treatments (if people do smoke). - Acute treatment uses medications to treat any infection (normally antibiotics) and to reduce inflammation (normally but it usually treated as though it were. Diabetes Mellitus type 1 Associated with the HLA-DR4 and 3 genes. - Autoimmune destruction of the pancreas, usually onsets in childhood. - It has an incidence of between 8 and 17 per 100,000 in the UK - It is a polygenic disease, and may be dominant, recessive or new onset. - The most influential gene, IDDM1, is located in the MHC class II region on Ch6, at region 6p21. - The classical symptoms are polyuria, nocturia, weight loss, polyphagia (increased hunger) and polydipsia (increased thirst) - Untreated, type 1 diabetes is fatal. - Diabetic ketoacidosis is the most deadly complication of DM1 macrophage derivatives known as giant cells, are found in 50% of cases and are most specific for Crohn's disease. aminosalicylate antiinflammatory drugs and corticosteroids). - Medications used to treat the symptoms of Crohn's disease include 5aminosalicylic acid (5-ASA) formulations, prednisone, immunomodulators such as azathioprine (given as the prodrug for 6mercaptopurine), methotrexate, infliximab, adalimumab, certolizumab and natalizumab. Hydrocortisone should be used in severe attacks of Crohn's disease. Type 1 diabetes can be distinguished from type 2 by autoantibody testing - glutamic acid decarboxylase autoantibodies (GADA), islet cell autoantibodies (ICA), insulinomaassociated (IA-2) autoantibodies, and zinc transporter autoantibodies (ZnT8) are present in individuals with type 1 diabetes, but not type 2. The C-peptide assay, which measures endogenous insulin production, can also be used. - Supplemental insulin - Islet or pancreas transplant - Cyclosporine A, an immunosuppressive agent, has apparently halted destruction of beta cells (on the basis of reduced insulin usage), but its nephrotoxicity and other side effects make it highly inappropriate for long-term use. - The risk of a child developing type 1 diabetes is about 10% if the father has it, about 10% if a sibling has it, about 4% if the mother has type 1 diabetes and was aged 25 or younger when the child was born, and about 1% if the mother was over 25 years old when the child was born. If one individual of a pair of monozygotic twins has DM1 then there is a 50% chance of the other twin having it. Guillain–Barré syndrome - This is an acute polyneuropathy affecting the peripheral nervous system. - It typically begins as weakness in the hands and feet, and advances rapidly up the body, so that within a day or two the patient is completely paralysed. - It can be life threatening if the respiratory muscles are affected or if the autonomic nervous system is involved. - It is usually (but not always) triggered by an infection. - Six subtypes of Guillain-Barré syndrome exist, but you do not really need to know these for the exams. - This autoimmune condition targets the nerve tissues due to molecular mimicry. - The most common preceding infection is Campylobacter Jejuni, but others are possible. - The most common symptom is symmetrical weakness that usually affects the lower limbs first, and rapidly ascends towards the trunk. - Often this will lead to involving the respiratory muscles, which can be life threatening. - The demyelination that can occur causes the majority of the symptoms. - This is a purely peripheral nerve disorder, and does not cause damage to the brain or spinal cord. - The diagnosis is usually made via nerve conduction studies and examination of the CSF. - The nerve conduction studies may show prolonged distal latencies, conduction slowing, conduction block, and temporal dispersion of compound action potential in demyelinating cases. - Patients often demonstrate areflexia (complete loss of the deep tendon reflexes). - About 80% of patients have myelin loss (which means they can rapidly recover by simply remyelinating the nerves. - The other 20% have axonal loss, which takes far longer to recover from. - The diagnosis of GBS depends on findings such as rapid development of muscle paralysis, areflexia, absence of fever, and a likely inciting event. Cerebrospinal fluid analysis (through a lumbar spinal puncture) and electrodiagnostic tests of nerves and muscles (such as nerve conduction studies) are common tests ordered in the diagnosis of GBS. - With prompt treatment by intravenous immunoglobulins or plasmapheresis, together with supportive care, the majority will recover completely. - Most patients require hospitalisation, and about 30% require ventilator assistance. - Subsequent treatment consists of attempting to reduce the body's attack on the nervous system, either by plasmapheresis, filtering antibodies out of the blood stream, or by administering intravenous immunoglobulins (IVIg), to neutralize harmful antibodies and inflammation causing disease. These two treatments are equally effective and a combination of the two is not significantly better than either alone. Glucocorticoids have not been found to be effective in GBS. Multiple Sclerosis - MS is also known as disseminated sclerosis or encephalomyelitis disseminate. - It is an inflammatory disease that leads to destruction of the myelin sheaths in the brain and spinal cord. - It is postulated (not known for certain) that MS is due to autoimmune destruction of the myelin producing schwann cells. - MS has an uncertain natural history, and the prognosis is very difficult to ascertain with any accuracy. In general, women have a better prognosis than men. - A better prognosis is also likely in people who develop the disease when they are young, those who initially experienced few attacks and those whose symptoms disappear completely between attacks. - There is a possible link between MS and vitamin D, as MS is less common in people living on or near the equator, regardless of their genealogical heritage. People that move to a new area of - The symptoms of MS include both physical and neurological problems. - The symptoms (especially symptoms occurring once the disease is more progressed) can occur either in isolated attacks or building up in a progressive manner. - Symptoms may disappear completely in between attacks, but unfortunately with repeated attacks, neurological damage occurs that is irreversible. - 85% of people improve after an attack, but the other 15% gradually worsen over time with no periods of recovery. - Features required for diagnosis are progressive weakness in legs and often arms, and areflexia (the absence of deep tendon reflexes) - MS is diagnosed based on the clinical picture (signs and symptoms) and some test results. - It is impossible to predict when an attack will occur, but they rarely occur more than twice per year. - It is known, however, that some things (springtime, viral infections etc) can increase the risk of a flare up. - There is no cure for MS, so treatment is mainly based around ameliorating attacks and delaying progression. - Unfortunately, many of the drugs used to treat MS have rather nasty side effects, so many people pursue alternative treatments. the world before the age of 15 acquire that regions risk of MS, and moving may be of benefit to older people as well. Wegener's granulomatosis - This disease is now known as Granulomatosis with polyangiitis. It is a systemic autoimmune disorder that involves both granulomatosis and polyangiitis. - It is a form of vasculitis that affects small and medium blood vessels. - Granulomatosis with polyangiitis is part of a larger group of vasculitic syndromes, all of which feature an autoimmune attack by an abnormal type of circulating antibody termed ANCAs (antineutrophil cytoplasmic antibodies) against small and - In general, rhinitis is the first sign in most patients. - Other signs include decreased kidney function and chronic renal failure, upper airway disease, ENT (ear, nose and throat) damage, pulmonary disease, joint problems, skin nodules and occasionally sensory neuropathy. - c-ANCA (antineutrophil cytoplasmic antibodies) - Granulomatosis with polyangiitis is usually suspected only when a patient has had unexplained symptoms for a long period of time. Determination of Anti-neutrophil cytoplasmic antibodies (ANCAs) can aid in the diagnosis, but positivity is not conclusive and negative ANCAs are not sufficient to reject the diagnosis. Cytoplasmic-staining ANCAs that react with the enzyme proteinase 3 (cANCA) in neutrophils are associated with Wegener's. - If the patient has renal failure or cutaneous vasculitis, a biopsy is obtained from the kidneys. - Without treatment, life expectancy is only around 5 months. - Steroids increase this to 8 months - Cyclophosphamide and newer immunosuppressive drugs have led to a 5 year survival rate of 87%. - In general, treatment is initially corticosteroids and oral cyclophosphamide, although the cyclophosphamide can be given IV. - Once the patient is in remission, treatment is usually changed from cyclophosphamide to medium-size blood vessels. Apart from Wegener's, this category includes Churg– Strauss syndrome and microscopic polyangiitis. azathioprine or methotrexate, as these are less toxic. - Rituximab has also recently been approved to treat the condition. Learn the following table regarding Crohn’s disease and ulcerative colitis!