Tolerance, Immune Regulation, and Autoimmunity
advertisement

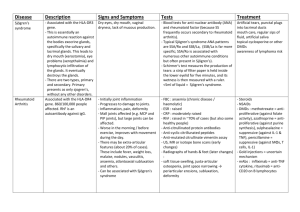
Aims • Describe autoimmune diseases, concentrating on the role of immunity in their pathogenesis. • Readings: Robbins, Chapter 5 Sjögren’s Syndrome • A systemic autoimmune disease • Inflammatory destruction of _exocrine_ glands. • Several secretory gland may be affected. salivary gland -dry mouth lacrimal gland -dry eye Robbins’ Basic Pathology 5-26 Sjögren’s Syndrome • Antibodies against a cytoplasmic RNA-protein complex, SS-A (Ro) and SS-B (La). • Associated with other systemic autoimmune diseases SLE RA scleroderma Graves Disease • Antibody mediated • _Hyperthyroidism_ induced by antibodies against TSH receptor. • Tissue-specific (thyroid gland) with systemic manifestations exophthalmos • Associated with specific alleles of HLA-DR3. • Women 7X more likely than men. Robbins and Cotran’s Pathologic Basis of Disease 24-8 Graves Disease • Thyroid stimulating immunoglobulin (TSI) binds to and activates the TSH receptor. Increased rate of thyroid hormone secretion. TSH levels are lower than normal. Graves Disease • Symptoms can be passively transferred Autoimmune Hypothyroidism • TSH-binding inhibitor immunoglobulins (TBIIs) Antibodies block TSH receptor activity rather than mimicking TSH as in Graves disease. • Antibody binding and recognition of a different epitope than that of Graves disease makes for a considerable difference in the clinical outcome. Multiple Sclerosis • Primarily a T cell-mediated disease. CD4+ and CD8 + cells MHC class _II_ expressing cells. Type IV hypersensitivity • Results in a progressive demyelinization of CNS leading to a loss of neuronal transmission. Adopted from WebPath Multiple Sclerosis • Is defined as “ Distinct episodes of neurologic deficits separated in time and separated by space.” • Relapsing-remitting form Myelin is destroyed, action potential is lost and neurological function is decreases. Neurological function returns slowly as the nerves generate more Na2+ channels to compensate for loss of action potential. • Chronic progressive form Myelin and axons are destroyed, no remissions, no return or restoration of function • Very rare acute progressive form (FYI) Multiple Sclerosis • Pathogenesis due to a genetic predisposition and environmental exposure. Linked to specific _HLA-DR2_ alleles. Possibly linked to viral infections: • EBV • adenovirus-2 • hepatitis B • A similar disease can be induced in mice immunized with myelin basic protein and a strong adjuvant. Type I Diabetes Mellitus • Mostly T cell-mediated disease. • CD8+ CTL destroy b cells of the pancreatic islets of Langerhans that produce insulin • Early Insulitis Lymphocyte infiltrate Similar to Robbins & Cotran’s Pathologic Basis of Disease 24-35 Type I Diabetes Mellitus • Genetic susceptibility In some cases, there is a hereditary tendency for b cell degeneration. 40% concordance in twins. Associated with DR3 and secondarily with DR4, and relative risk is almost 100 in those carrying DR3 and DQw8 Adapted from Robbins’ Basic Pathology 17-7 7th Ed Type I Diabetes Mellitus • Environment Emigrants assume the risk of type I diabetes closer to that of their destination country than their country of origin. Viral infections. • Coxsackie virus Chemicals. • Cow’s milk Adopted from Robbins’ Basic Pathology 17-7 7th Ed Type I Diabetes Mellitus • Organ-specific with systemic manifestations. • ~10% of patient have some other autoimmune disorder. • Anti-insulin antibodies may be generated. Anti-islet cell antibodies (70-80-% of patients). Rheumatoid Arthritis • Both antibody and T cell mediated disease. • Systemic disease. • Characterized by chronic inflammation of the synovium and other connective tissues. • The inflammation is initiated by the deposition of IC and sustained by chronic inflammatory cells. Pathogenesis of Rheumatoid Arthritis • Molecular mimicry Unknown antigen • Genetic susceptibility Associated with HLADR4. • T cell activation • Rheumatoid factor production Anti-Ig antibody (usually IgM) in a high percentage of patients. • Pannus formation Adopted from Robbins’ Basic Pathology 5-25 Pannus • _Fibrovascular_ tissue. • Consists of fibroblasts, macrophages, T cells and plasma cells. • Has the potential to invade surrounding tissues including the bone, cartilage, and tendon. Some notes on Rheumatoid Factor and ANA • A minority of RA patients do not have elevated RF and some with RF do not have RA. • Relatively high ANA and RF may be found in some otherwise normal persons. • Certain infectious diseases induce high RF and ANA. • Titers of RF do not always correlate with severity and occurrence. • RA occurs in some agammaglobulinemic patients. • RF may be elevated in SLE and ANA in RA. • RF may be a marker but may not be a mechanism. Hashimoto’s Thyroiditis • Autoimmune disease of the Thyroid gland. Highly organ-specific. • Results in _Hypothyroidism. • Most likely T cell-mediated. Due to presence of infiltrating mononuclear cells. Characteristic of type IV hypersensitivity reaction. • There are autoantibodies present in these patients. Antibodies against a cytoplasmic antigen. Hashimoto’s Thyroiditis • HLA association with HLA-DR5 and DR-3 as well as HLA-B8 alleles. Treatments of Autoimmune Diseases • Metabolic control therapies. factor replacement therapy • Graves’ disease • Myasthenia gravis organ transplant • SLE nephritis _plamapheresis • SLE Treatments of Autoimmune Diseases • Immunosuppressive therapy inhibit inflammation examples • NSAIDs • corticosteroids have no effect on cause of disease Recent Therapies • Bone marrow ablation and transplant SLE and scleroderma • IFN-b.1a MS • TNF-alpha blockade RA Oral Tolerance - Low Dose Ag Ag administered orally induces specific regulatory T-cell (Th3) Inhibits IgA isotype switch Th3 TGF-b suppresses Th1 and Th2 activation, proliferation, and cytokine production Oral Tolerance - High Dose Ag • Induces Systemic T-cell tolerance probably through clonal exhaustion Oral Tolerance • Clinical trials involving oral tolerance: Bovine myelin basic protein in MS Type II collagen in RA Retinal S-antigen in posterior uveitis Insulin in type I diabetes mellitus Oral feeding of HLA molecules to prevent graft rejection Crohn’s and Ulcerative Colitis patients may have deficient oral tolerance mechanisms. Review • Tolerance is the process by which the body ensures that immune responses are directed against foreign or altered self antigens and not normal self. There is central and peripheral tolerance. • Autoimmune diseases result from a breakdown of tolerance. • Autoimmune diseases can be organ specific or systemic. • Autoimmune diseases can be antibody mediated, cell mediated, or both. • Autoimmune diseases can be types II, III, or IV hypersensitivity reactions. • Autoimmune diseases are treated through direct metabolic control, by immunosuppression, and by immunomodulation. Next Time • Define autograft, isograft, allograft, and Xenograft. • Compare and contrast hyper acute, acute, and chronic graft rejection and graft vs. host and host vs. graft disease. • Quantitative and qualitative deficiencies in neutrophils (phagocytosis). • Readings: Abbas & Lichtman, Chapter 10 Objectives 1. Describe autoimmune diseases, concentrating on the role of immunity in their pathogenesis. 1. Sjogren’s syndrome, Graves disease, Autoimmune hypothyroidism, Multiple sclerosis, Type I diabetes, Rheumatois arthritis, Hashimoto’s thyroiditis 2. Describe the treatment options for these various autoimmune diseases.