UTI in childhood - management at a glance 2015
advertisement

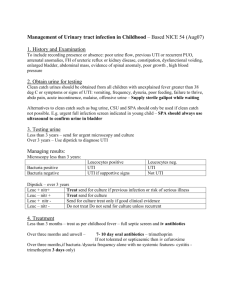
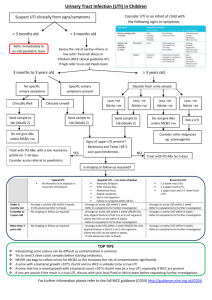
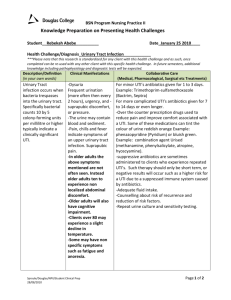
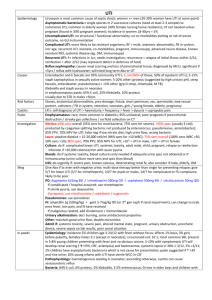
UTI in childhood management at a glance Urinary tract infections are more common in boys until 3 months of age (due to more con.genital abnormalities- obstructive uropathy, vesico-ureteric reflux (VUR)) after which the incidence is substantially higher in girls. At least 8% of girls and 2% of boys will have a UTI in childhood Presentation in childhood depends on age: - Infants: poor feeding, vomiting, irritability - Younger children: abdominal pain, fever, dysuria - Older children: dysuria, frequency, haematuria NICE guidelines for checking urine sample in a child -- If there are any symptoms or signs suggestive or a UTI -- With unexplained fever of 38°C or higher (test urine after 24 hours at the latest) -- With an alternative site of infection but who remain unwell (consider urine test after 24 hours at the latest) Clean catch is preferable but if this is not possible then urine collection pads should be used. Cotton wool balls, gauze and sanitary towels are not suitable Management: -- Infants less than 3 months old should be referred immediately to a paediatrician -- Children aged more than 3 months old with an upper UTI (> 38ºC, loin pain/tenderness) should be considered for admission to hospital. If not admitted oral antibiotics such as cephalosporin or co-amoxiclav should be given for 7-10 days -- Children aged more than 3 months old but <3 years with lower UTI symptoms - send a sample for urgent microscopy and culture. Await the result before starting treatment, unless they are very systemically unwell. -- Children aged >3 years: use dipstick test to diagnose UTI: - If leukocyte esterase and nitrite are positive: start antibiotic treatment for UTI. - If leukocyte esterase is negative and nitrite is positive: start antibiotic treatment if a fresh sample was tested and send urine sample for culture. - If leukocyte esterase is positive and nitrite is negative: send urine sample for microscopy and culture. Only start antibiotic treatment for UTI if there is good clinical evidence of such infection. - If leukocyte esterase and nitrite are negative: do not start treatment for UTI, and explore other causes of illness. Imaging for children with proven UTI: There are three imaging modalities that NICE recommend children to have (depending on circumstances). This is because UTIs in children can cause renal scarring. 1) Ultrasound scan: - Can accurately assess renal size and outline and identify most congenital abnormalities, renal calculi and hydronephrosis or hydroureter, indicating the presence of obstruction or severe reflux. - It is less effective in detecting mild or moderate vesico-ureteric reflux in children with UTIs. 2) Micturating cystography (MCUG): - Is the gold standard investigation for reflux and is the only imaging technique that provides information about the urethra. - Should be performed by a skilled radiologist with experience in acquiring and interpreting the images. - The disadvantage of micturating cystography is its invasiveness, as it requires catheterisation. 3) Dimercaptosuccinic acid scintigraphy (DMSA): - Is the gold standard for detecting renal parenchymal defects. - Study renal function using a radio-pharmaceutical such as technetium 99m. - The isotope is concentrated in the proximal renal tubules, and its distribution correlates with functioning renal tissue. Children less than 6 months old: A) Responds well to treatment within 48 hours - No Ultrasound during the acute infection but USS within six weeks is required. MCUG may be needed if USS is abnormal. B) Atypical UTI (seriously ill, raised creatinine, septicaemia, failure to respond to treatment within 48 hours, infection with non-E. coli species) - USS required in the acute illness (but not at six weeks). However the child will need a DMSA scan 4-6 months following the acute infection. An MCUG would be needed as well. C) Recurrent UTI (two or more episodes of UTI with acute pyelonephritis/infection of the upper urinary tract, three or more episodes of UTI with cystitis/lower urinary tract infection) - USS needed during the acute illness, a DMSA scan 4-6 months later. A MCUG is also needed. Children between 6 months and 3 years old: A) Responds well to treatment within 48 hours - no imaging required. B) Atypical UTI - needs an USS during the acute illness as well as a DMSA scan in 4-6 months post illness. C) Recurrent UTI - need USS within the first six weeks post infection as well as a DMSA scan in 4-6 months post infection. Children older than 3 years: A) Responds well to treatment within 48 hours - no imaging required. B) Atypical UTI - just needs an USS during the acute infection. C) Recurrent UTI - Needs an USS within six week post infection as well as a DMSA scan in 4-6 months. Recurrent UTI guidance =- 2 upper UTI illnesses or 3 lower UTIs