surgical glossary of terms abdominoperineal resection
advertisement

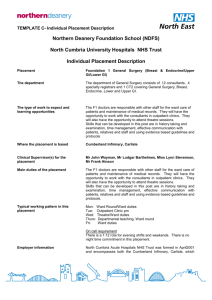
CONTENTS PAGE 1: CONTENTS PAGE 2: INTRODUCTION PAGE 3: MENTORS PAGE 4: OFF DUTY/SHIFT TIMES PAGE 5: THE STAFF PAGE 6: THE CONSULTANTS PAGE 7: LEARNING OPPORTUNITIES PAGE 8: CONTINUATION OF LEARNING OPPORTUNITIES PAGE 9: CHECKLIST PAGE 10: ORTHOPAEDIC GLOSSARY OF TERMS PAGE 11: SURGICAL GLOSSARY OF TERMS PAGE 12: SURGICAL GLOSSARY OF TERMS PAGE 13: ORTHOPAEDIC ABBREVIATIONS 1 INTRODUCTION Welcome to Ward 2! We hope that you enjoy your placement here and that it will be an invaluable learning experience. If at any time you have a problem, please feel free to discuss them with either your mentor, nurse in charge, or the Ward PLT representatives. Ward 2 is a mixed Surgical/Orthopaedic ward consisting of 28 beds. The ward layout is 5, 4 bedded bays and 8 side rooms. The workload is variable and the patient turnover is high. Our orthopaedic patients are generally undergoing planned surgery, or who have sustained traumatic injuries to their musculo-skeletal system. Our Surgical patients undergo Breast and Bowel surgery, Hernia repairs, Cholecystectomy, Urology (TURB/TURP) Patients are admitted to Ward 2 usually from A+E, EAU, Day Ward or from an elective list. A comprehensive nursing assessment is performed, care and interventions planned, care initiated, implemented and evaluated. We generally use core care plans, adapted to the patients’ individual needs. Most of the nursing documentation is done manually, although there will be opportunities to access computer based information, such as Trust policies and procedures. We work very closely with other members of the Multi- professional team: Medical staff, Physiotherapists, Occupational Therapists, Social Workers, Dieticians, Pharmacy and Plaster room staff. 2 MENTORS For the duration of your placement, you will be assigned to a Mentor, Associate Mentor, and an experienced Healthcare Support Worker, who has undertaken the NVQ Assessment level 1+2. Sometimes you may also be allocated a Student Nurse Buddy. MENTOR……………………………………………………… ASSOCIATE………………………………………………….. HCSW…………………………………………………………… STUDENT NURSE BUDDY…………………………………… Wherever possible, we try to allocate you to work with a single mentor during your placement. When this is not possible an associate mentor is allocated, you will gain the most from your placement if you work the same hours as your mentors. If this cause any difficulty, please discuss with your mentor. 3 OFF DUTY/SHIFT TIMES Ward 2 operates a 4 shift pattern Early (E) 0700-1430 Late (L) 1230-2000 Long Day (LD) 0700-2000 Night (N)1930-0730 Your off duty is………………………………………………………………………………………………… We have enclosed your first weeks off duty to ensure a smooth transition into your placement. This is to ensure that you are assigned to your mentor when starting this placement. At times we have a high number of students on the ward at the same time, at these times you may find your off duty is completed for your whole placement. This is to give you all the chance to have the same learning experiences. Please do not change these shifts without speaking to either your mentor or one of the Jr Sr in charge, you may also note that we have assigned an insight visit on a set weekly pattern, this is to ensure that you gain enough insight days to enhance your learning opportunities whilst on this placement. Please note, that as adult learners, it is your responsibility to arrange these insight visit days and not use them as study days. The Ward telephone number is 01476 565232 (Ext 4420/4245). If the need arises that you need to call in sick, we would ask that you follow the guidelines given to you by the School of Nursing and that you also call the ward to let us know that you will not be on duty that day. 4 THE STAFF Ward Sister: Di Woods Junior Sisters: Janet Brassington Sharon Kelham Julie Record Ward Clerks: Rachel Barrett Debbie Buttigieg PLT Reps: Jo Macmillan Joy White Pharmacists: Claire Vaughan Physiotherapist: Maggie Close Breast Care Nurse: Nicki Turner Colorectal Nurses: Bobby Lee Rachel Jefferson Outreach/Pain Nurses: Linda Gough Carole Hay Mental Health Liaison: Jo Jeanette Amanda 5 THE CONSULTANTS ORTHOPEADIC: Mr A Y Othman (AYO) Mr Paramasivan (ONP) Mr G K Singhania (GKS) Mr Trehan (RTR) Mr Uryszek (DUR) BREAST: Mr Modi (MODI) Mr Potdar COLORECTAL: Mr Mathur (DM) Miss Varma (AVA) Patients are seen on a daily basis by the Consultants or their Registrar and surgical teams, usually early morning. The team of orthopaedic doctors are based on the ward but they also have theatre time and cover A+E. 6 LEARNING OPPORTUNITIES AND INSIGHT VISITS There are a variety of learning opportunities on ward 2 including: Investigative procedures, e.g. x-ray, ultrasound, MRI Ward Rounds Discharge Planning Drug rounds Patient transfers Accompanying patients to Plaster Room Transferring and collecting patients from theatre Post-operative care Multidisciplinary meetings Insight Visits include: Pre Assessment Clinic Hip and Knee classes Ward physiotherapist and OT’s Porters Pharmacy Any of the specialist nurses working in conjunction with Ward 2 patients e.g. Breast Nurse, Colorectal Nurse. Dietician Accompanying any of the Ward Team to extended Role Meetings e.g. Infection control, PLT, Tissue Viability. 7 We suggest you follow a patient journey from Pre Admission clinic, through theatre and back to rehabilitation on the ward, through to discharge. This is of great value to both Student and the Patient. The staff on Ward 2 acknowledge the individuality of each student and therefore, after discussion with your mentor, every effort will be made to tailor available opportunities to your individual needs. Please come to placement prepared, with your Action Plan outlining goals, learning needs and objectives for this placement. 8 CHECKLIST Whilst on placement, ensure that you are able to: Find: Emergency phone numbers Emergency bells and recognise the sound Resuscitation Trolley Fire alarms and exits Have Knowledge of: Visiting Times and arrangements Staff Breaks Protocol for telephone enquiries Facilities for relatives refreshments Have knowledge and understanding of individual bed areas: The oxygen, suction and air points How each bed works Documentation and observation charts Be able to contact the following: Porters Standby Sister On call Doctor Pharmacy Emergency Call out/ medical emergency At the end of your placement we appreciate feedback, please be as honest as you like, we can only be aware of our strengths and weaknesses if you tell us!! 9 GLOSSARY OF TERMS ABDUCTION: Moving a limb away from the mid line of the body ADDUCTION: Moving a limb towards the mid line of the body ARTHROPLASTY: Remodelling or reorganisation of a joint AVULSION: Forcible separation DISLOCATION: Displacement of joint surfaces DORSIFLEXION: Bringing the foot and toes upwards EFFUSION: An increase of synovial fluid within a joint causing swelling MENISCUS: A semilunar cartilage in the knee ORTHOSIS: Splint or surgical appliance OSTEOTOMY: Surgical division of the knee PLANTAR FLEXION: Bringing the foot and toes downwards PROTHESIS: An artificial part fitted to the body to replace a diseased/damaged part SUBLUXATION: Partial dislocation of two surfaces that are normally in contact with each other TENOTOMY: Surgical division of a tendon VALGUS: A limb deformity which the extremity is moved away from the mid line VARUS: A limb deformity which the extremity is moved towards the mid line 10 SURGICAL GLOSSARY OF TERMS ABDOMINOPERINEAL RESECTION: the surgical removal of the anus, rectum, and sigmoid colon, resulting in the need for a permanent colostomy. ADHESION: a band of scar tissue that connects two surfaces of the body that are normally separate. AXILLARY NODES: The lymph nodes (or glands) located under the arms COLOSTOMY: the surgical creation of an opening between the surface of the skin and the colon; also referred to as a large intestine stoma. This is usually done when very large areas of bowel are removed, and the ends cannot be joined, or when there is a blockage in the intestine. DIVERTICULITIS: an inflammation or infection of small sacs or outpouchings (diverticula) of the inner lining of the intestine that protrude through the intestinal wall. ENDOSCOPY: a method of physical examination using a lighted, flexible instrument to see the inside of the digestive tract. The scope can be passed through the mouth or through the anus, depending on which part of the digestive tract is being examined. This method is referred to by different names depending on the area of examination, such as: esophagoscopy (esophagus), gastroscopy (stomach), upper endoscopy (small intestine), sigmoidoscopy (lower third of the large intestine), and colonoscopy (entire large intestine). FISTULA: abnormal connection that forms between two internal organs or two different parts of the intestine. 11 ILEOSTOMY: the surgical creation of an opening between the surface of the skin and the ileum, the lowermost section of the small intestine. LAPAROSCOPY/LAPAROSCOPIC SURGERY: a method of surgery that is much less invasive than traditional surgery. Tiny incisions are made to create a passageway for a special instrument called a laparoscope. This thin telescope-like instrument with a miniature video camera and light source is used to transmit images to a video monitor. The surgeon watches the video screen while performing the procedure with small instruments that pass through small tubes placed in the incision LUMPECTOMY: Removal of a small area of breast tissue with or without healthy tissue, also known as Wide Local Excision (WLE). PERISTALSIS: the means by which food or waste is propelled through the gastrointestinal tract in a series of muscular contractions. STOMA: an artificial opening of the intestine to outside the abdominal wall TURBT: Transurethral resection of a tumour in the bladder TURP: Transurethral resection of a tumour in the prostate 12 ORTHOPAEDIC ABBREVIATIONS # Fracture PIP Proximal Inter Phalangeal DIP Distal Inter Phalangeal MC Metacarpal MT Metatarsal #NOF Fractured Neck of Femur #SOF Fractured Shaft of Femur THR Total Hip Replacement TKR Total Knee Replacement DHS Dynamic Hip Screw ORIF Open Reduction + Internal Fixation MUA Manipulation under Anaesthetic CSM Colour Sensation Movement NWB Non Weight Bearing PWB Partial Weight Bearing FWB Full Weight Bearing 13