Diabetes Case Study

Caitlin Mazurek
KNH 413
3/26/2012
Type 1 Diabetes Mellitus with Diabetic Ketoacidosis
1.
There are precipitating factors for diabetic ketoacidosis. List at least seven possible factors.
The following are risk factors for diabetic ketoacidosis:
People with type 1 diabetes
Infection
Injury
Serious illness
Surgery
Missing doses of insulin
Hispanic and African Americans are more likely to have ketoacidosis
2.
Describe the metabolic events that led to the symptoms associated with DKA.
Events that can lead to the symptoms include the following: blood sugar greater than
240 mg/dL, having an illness usch as pneumonia or a recent heart attack, nausea or vomiting, or being pregnant.
3.
Assess Susan’s physical examination. What is consistent with diabetic ketoacidosis?
Give the physiological rationale for each that you identify.
Even when Susan is extremely active and taking the normal amount of insulin, her blood glucose tests are still above 240 mg/dL constantly. This is probably cause enough for ketoacidosis. This and the fact that her breath smelled of acetone and her eyes were sunken in.
4.
Examine Susan’s biochemical indices both in the chemistry section and in her ABG report. Which are consistent with DKA? Why?
Her CO2 content was low as well as her blood pH, and HCO3-. These are all probably cause with DKA.
5.
If Susan’s symptoms were left untreated, what would happen?
If the symptoms were left untreated, Susan could all into severe illness or death. Susan could fall into a diabetic coma if treatment is delayed. There could also be fluid buildup in the brain, a heart attack could occur, there could be kidney failure, or death of bowel tissue could happen due to low blood pressure.
6.
Assuming Susan’s SMBG records are correct, what events seem to have precipitated the development of DKA?
Susan’s records indicate that her blood glucose levels being so extremely high after her period was ending and she had her birthday. This could mean that there was possible alcohol intake on her birthday, she also could have eaten more carbohydrates then. Her levels were also strange during a volleyball tournament, when her activity level was higher than normal.
7.
What, if anything, could Susan have done to avoid DKA?
Susan could have eaten less carbohydrates, taken more insulin, or drank more water.
8.
While Susan is being stabilized, Tagamet is being given IV piggyback. What does “IV piggyback” mean? What is Tagamet, and why has it been prescribed?
Tagamet is used to decrease the amount of acid that is found in the stomach. This could be used since her pH levels were found to be slightly more acidic than normal. IV
piggyback means that the medicine is being given on top of a normal IV solution of saline or something of the sorts. It is injected through a stable and previous IV line.
9.
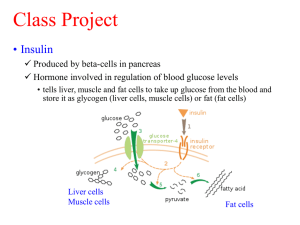
The Diabetes Control and Complications Trial was a landmark multicenter trial designed to test the proposition that complications of diabetes mellitus are related to elevation of plasma glucose. It is the longest and largest prospective study showing that lowering blood glucose concentration slows or prevents development of complications common to individuals with diabetes. The trial compared “intensive” insulin therapy
(“tight control”) with “conventional” insulin therapy. Define “intensive” insulin therapy.
Define “conventional” insulin therapy.
Intensive insulin therapy is an aggressive treatment approach designed to control blood sugar levels. This requires close monitoring as well as frequent doses of insulin.
Conventional insulin therapy usually only involves one to three daily injections of insulin that are the same everyday. How much and when differs depending on activity level and diet.
10.
List the microvascular and neurologic complications associated with type 1 diabetes.
Possible eye problems or sensitivity to light
Feet and skin can develop sores and infections
Poor blood circulation
Difficulty controlling blood pressure and cholesterol, this can lead to heart attack, stroke, and other problems
Nerves in the body can become damaged causing pain, tingling, and loss of feeling
Problems digesting food due to nerve damage
High blood sugar can lead to kidney damage
11.
What are the advantages of intensive insulin therapy?
This can prevent or slow the progression of long-term diabetes complications including reducing risk of heart attacks, strokes, eye damage, nerve damage, and kidney disease.
It can also boost energy and help in feeling more alert in general.
12.
What are the risks of intensive insulin therapy (tight control)?
The main two risks of intensive insulin therapy are low blood sugar and weight loss. If someone has already lost a significant amount of weight, then this therapy method may not be right.
13.
Dr. Green consults with you, and the two of you decide that Susan would benefit from insulin pump therapy combined with CHO counting for intensive insulin therapy. This will give Susan better glycemic control and more flexibility. What are some of the key characteristics of candidates for intensive insulin therapy?
They understand how to carbohydrate count, they do not have heart disease, blood vessel disease, or any severe complications. They are able to control their blood sugar with diet and insulin injections. They are usually active individuals as well.
14.
Explain how an insulin pump works. Is Susan a candidate for an insulin pump?
An insulin pump is a device that automatically delivers a certain amount of insulin to the body. This is a device that can be taken off and moved around on the body. It is adhered to certain spots of skin on the body commonly around the waist or on the back of an arm. The insulin can then be injected in a bolus, which is a large amount all at once, or a dose that is pumped continuously at an adjustable rate. Susan is a candidate for an insulin pump due to her ability to be able to count carbohydrates and being an active individual, this is a little easier at times to take insulin, rather than syringes.
15.
How would you describe CHO counting to Susan and her family?
Carbohydrate counting is a simple process. Generally speaking, use the rule of 15, where most foods can be counted in increments of 15. Generally, foods that are in the grains, dairy, fruits, and starchy vegetables are the food groups that need to be accounted for as well as sweets. A serving of dairy is around 12 carbs, and a serving of carbs, fruits, and starchy vegetables is usually 15 carbs per serving.
16.
How is CHO counting used with intensive insulin therapy?
Understanding how many carbohydrates are being eaten at each time during the day, certain adjustable boluses can be given using the insulin pump. By telling the pump how much you are about to eat or have already eaten, the correct amount of insulin can be taken without hesitation.
17.
Estimate Susan’s daily energy needs using the Harris-Benedict equation.
2300 kcal/day
18.
Using the 1-week food diary from Susan, calculate the average amount of CHO usually consumed each meal and snack. a.
100 grams CHO breakfast b.
60 grams CHO lunch c.
30 grams CHO snack d.
75 grams CHO dinner e.
45 grams CHO HS
19.
After you have calculated Susan’s usual CHO intake from her food record, develop a
CHO-counting meal plan that she could use. Include menu ideas.
Meal
Breakfast
Nutrients
45-60 grams of carbohydrates or
3-4 CHO choices
1 oz meat/meat substitutes
1-2 servings of fat
Food Ideas
1 cup of Cheerios with ½ cup 2% milk,
½ of a banana with 1 T peanut butter
Lunch
Snack
45-60 grams of carbohydrates or
3-4 CHO choices
2-3 oz meat/meat substitutes
1-2 servings fat
Turkey sandwich: 2 slices whole wheat bread, 2 oz deli turkey, lettuce, tomato, 2 tsp mayonnaise, mustard
1 medium apple, 1 oz carrot sticks 2 T fat-free Ranch dressing
1 oz pretzels with peanut butter or hummus, or a yogurt
Dinner
HS
15-25 grams of carbohydrates or
1-2 CHO choices limit meat and fat
45-60 grams of carbohydrates or
3-4 CHO choices
3 oz meat/meat substitutes
1-2 servings fat
15 grams of carbohydrates or 1
CHO choice limit meat and fat
3 oz chicken breast- grilled with bbq sauce, side salad with fat-free dressing, 1 small baked potato with sour cream and cheese, 1 8-oz glass of
2% milk, 1 small slice of cake
3 graham crackers or 1 small piece of fruit or ½ cup of ice cream
20.
Just before Susan is discharged, her mother asks you, “My friend who owns a health food store told me that Susan should use Stevia instead of artificial sweeteners or sugar.
What do you think?” What will you tell Susan and her mother?
Stevia is a great alternative for certain people. Some people tend to not like the aftertaste that it has when used in baking products. The sugar is not the main thing to worry about with Susan’s diet, however, it is the carbohydrates. Yes sugar adds to the carbohydrates in the food, but changing to Stevia will not cure anything. Personally, if you choose to use regular sugar, you will just have to be counting the carbohydrates for that product and making sure that you are counting accordingly. As mentioned, the most necessary component for diabetes management is carbohydrate counting. The use of Stevia can be a personal preference, but I would say that you could probably stick to using sugar instead of the artificial sweeteners.