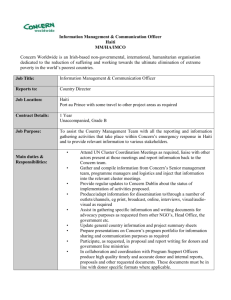
Position/Job Title: Condition Management Nurse Reports to
advertisement
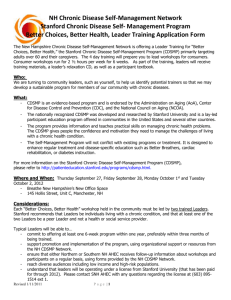
Position/Job Title: Reports to: Approved/Revised Date: Job Code: Pay Class: Condition Management Nurse Program Manager Condition Management 01/20/2014 E-005/E-006 E-005/E-006 Summary: The Condition Management (CM) Nurse is responsible for the implementation of the Integrated Health Partners (IHP) condition management program. This program focuses on improving the health status of individuals with specific chronic conditions ultimately resulting in improved quality of life for the participant, a more engaged employee for the customer/employer, and health care cost savings for the customer/employer. The CM Nurse identifies potential enrollees within targeted populations with specific conditions, conducts outreach, facilitates engagement in the customer CM program, assesses participant needs, and together with participants develops plans to address needs/issues related to condition(s) and/or overall health. Essential Functions: 1. 2. 3. 4. 5. 6. Using risk stratification system, targets enrollees in customer’s condition management program for outreach. Conducts outreach by telephone, secure e-mail, or mail with goal of engaging enrollee in program. Conducts condition management education regarding the condition, symptom management, red flag warning signs related to the condition, importance of adhering to medications and evidence-based guidelines, and refers to customer sponsored support programs as appropriate for individuals with target chronic conditions or within identified sub-populations. With participant, establishes self-management goal using self-management support concepts and motivational interviewing techniques. Develops and implements plans to increase client motivation and self-efficacy in all aspects of chronic condition management. Documents all condition management activities appropriately, promoting accurate and timely reporting to customer. Additional Responsibilities/Duties: (The following examples are intended to be descriptive but not restrictive.) 1. 2. Applies the principles of the nursing process to condition management of individuals with chronic conditions. Revises the risk score of a participant based on information obtained during conversations with the participant. Document1 -1- 3. 4. 5. 6. 7. 8. Monitors clinical objectives related to clients’ chronic conditions, including self-reported ability to do regular daily activities and be productive at work, avoid hospital and emergency department admissions, and reduce gaps in evidence-based care. Encourages participant to consent to sharing of information between CM nurse and primary care physician. Assists with program development, planning, and meetings with customer as requested. Maintains a working knowledge of applicable Federal, State and local laws and regulations, the Compliance Accountability Program, Code of Ethics, ERISA, HIPAA privacy and transaction and code set requirements, as well as other policies and procedures, in order to ensure adherence in a manner that reflects honest, ethical and professional behavior. Demonstrates commitment to providing outstanding customer service in a manner that is reflective of our mission, values, and customer service standards. Performs related duties as assigned. Education/Experience (Minimum Requirements): RN with current Michigan license in good standing; Bachelor’s degree in nursing or health related field preferred. Minimum three years clinical experience. Certified Case Management or Chronic Care Nurse preferred. Stanford Self-management (PATH) certified or commitment to complete the training is desired. Specific Knowledge, Skills, Licenses, Certifications, Etc: Experience: Three to five years clinical nursing experience in acute care setting or equivalent ambulatory experience. Additional experience in home health, physician practice, or other community setting preferred. Skills: Ability to communicate orally and in writing clearly and assertively. Ability to analyze, plan, and problem-solve effectively. Ability to organize, prioritize, and be flexible. Licensure: RN with current Michigan license in good standing. This position will require flexible daytime and evening hours to accommodate participant needs. Weekend on call hours will be required. Integrated Health Partners (IHP) is committed to the principle of equal opportunity in employment. Integrated Health Partners does not discriminate on the basis of gender, race, color, creed, national origin, age, religion, sexual orientation, veteran status, or disability in participation in, access to, or employment in its organization, programs and activities. The above statements are intended to describe the general nature and levels of the work performed and are not exhaustive lists of all duties, responsibilities, knowledge, skills, and abilities and working conditions associated with the job. As changes occur IHP reserves the right to modify the above description. Document1 -2-