Anaemia - WordPress.com
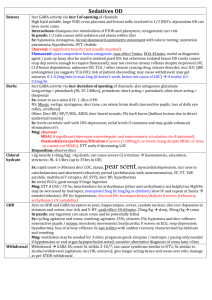
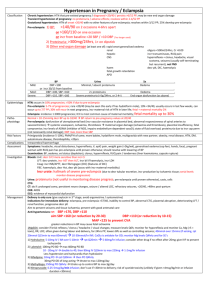
advertisement

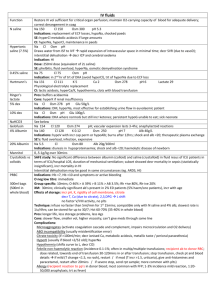
Anaemia Cause MICROCYTIC Anaemia MCV <80 Incr RDW Type Cause GI / GU blood loss; Malabsorption Pregnancy; Dietary Sx / Mng Mng: IV Fe if severe anaemia not requiring b/ transfusion, or unable to tolerate PO (may be normo) Normal globin chains produced at decreased rate haemolysis (hence normo) Alpha: more common in SE Asia; HbBarts (4; IU demise); HbH (3; mod disease); trait (2; asymptomatic) Beta: more common in Europe; Hetero = minor (asymptomatic); homo = major; more symptomatic than alpha Fe overload (hepatosplenomegaly, cardiac disease) Pathological #, bone deformities, paraspinal masses Endocrine failure Recurrent infections Mng: trt Fe overload with desferrioxamine; stem cell transplant; often require transfusions Decr: Ferritin (<15), Fe (<13), Hct (<30, occurs late) MCV:Hb 10:1 Incr: reticulocytes, erythroblasts (haemolysis) HbF (>90%) Normal: RBC count Decr: MCH; Hb (3-9) Poikilocytosis, anisocytosis, incr no. of erythroid precursors on BM biopsy, nucleated RBC’s, basophilic stippling, target cells Mng: Pyridoxine trial 2-3/12 Incr: Fe + Ferritin (may be normal) Sideroblastic Hereditary (may respond to pyridoxine) Lead poisoning, ETOH Myelodysplastic syndrome / myeloproliferative disease Fe def Thalassaemia MACROCYCTIC Anaemia MCV >100 Vit B12 def MCV >115 Folate def MCV >115 Other Incr: TIBC, transferrin (>3.6) Normal: Fe binding capacity Sideroblasts in BM Incr: globulins Multiple myeloma AOCD Blood findings Hypothyroidism; vit C def Pernicious anaemia (autoab to parietal cell and intrinsic factor decr production of IF, prevent formation of complex; mean onset 60yrs) Gastrectomy, gastric atrophy, ileal disease, pancreatic disease Malabsorption (most common cause; eg. Bacterial overgrowth) Dietary (ie. Vegans) NO (prolonged / repeated exposure) Assoc with: autoimmune thyroiditis, Graves, Addisons, 1Y hypoPT, vitiligo, MG Dementia, psychosis, peri neuropathy, subacute degeneration of spinal cord (occurs faster if only folate supplementation; due to demyelination; affects post + lat columns), abnormal gait Gastric adenoCa / carcinoid Achlorhydria, painful smooth tongue Dietary (most common; esp in alcoholics) Malabsorption Incr demand (pregnancy, malignancy, psoriasis) Dihydrofolate reductase inhibitors (eg. methotrexate, trimethoprim) Phenytoin, Na valproate Mng: 5mg folate OD; vit B12 if def suspected Normal: ferritin Decr: RBC count Incr: LDH Decr: B12; WBC and plt; holotranscolabalmin II Anti-parietal cell and IF ab’s; Hypersegmented neutrophils; Stippling of red cells; Howell Jolly bodies; Schilling test (decr urinary B12 that is incr by giving IF) Mng: Vit B12 injections; high dose PO vit B12 Incr: RDW (increases early, and shows there is a variety in size of RBC’s) Decr: folate Alcoholism; chronic liver disease; hypothyroidism; congenital cyanotic heart disease; myelodysplastic syndromes; Megaloblastic reticulocytosis NORMOchromic Anaemia MCV 80100 Aplastic anaemia (becomes macrocytic) AOCD (becomes macrocytic) Esp in SE Asia; cause by stem cell loss Idiopathic (50-65%) Fanconi’s syndrome (autosomal recessive) Radiation Chloramphenicol, gold, sulphur drugs, chlorpromazine, streptomycin Viral infections (eg. hepatitis) SLE; Pregnancy; Graft vs host Decr tissue oxygenation, immunocompromise, bleeding Fatigue, weakness No splenomegaly Most common cause of normocytic Mng: b/ transfusion; consider Fe; erythropoietin Due to incr hepcidin, decr erythropoietin, inhibited marrow proliferation, altered Fe distribution, decr RBC life span, incr reticuloendothelial activity RA, CRF, Ca, CT disorders Defect in membrane proteins (spectrin) decr deformability haemolysis Hypocellular BM Mng: supportive; ABx; blood products; immunosupp; G-CSF ARF Spherocytosis Decr: reticulocytes, WBC, plt Usually asymptomatic Splenomegaly (moderate; 50% young children, 85% adults) Jaundice, gallstones (5% children, 50% adults) Haemolytic crises (usually during infections; mild) Aplastic crises (parvovirus infection) Leg ulcers, spinal cord lesions Mng: splenectomy, cholecystetcomy Incr: ferritin Normal: reticulocytes and RDW Decr: Fe, transferrin, TIBC Normal reticulocytes and RDW Features of haemolysis + Incr: RDW Decr: MCHC (in 50%) Spherocytes (quite non-specific); incr osmotic fragility; variable degree of anaemia Coombs negative Haemolysis screen = haptoglobins, LDH, Coombs, unconj/conj bil Urinary: urobilinogen Elliptocytosis haemolysis Similar to above but milder As per spherocytosis G6PD def X-linked inherited; more common in males, Black Splenomegaly, neonatal jaundice, gallstones Features of haemolysis + G6PD assay Due to oxidative stress haemolysis Trigger: infection; sulphonamides, nitrofurantoin, antimalarials, vit K, aspirin PK def Sickle cell disease Autosomal recessive haemolysis Autosomal recessive; account for 70% congenital Hb disorders; esp in Black (occurs in 8%), Middle East, Indian Defect in Hb production (valine/glycine) HbS polymerization when low NO conc damage to membrane haemolysis, incr intracellular Ca, rigid RBC’s, activation of thrombosis Triggers: hypoxia, acidosis, 2,3,DPG, vascular stasis, IV vol depletion, infection, dehydration, altitude, cold Acquired autoimmune haemolytic, cold Extravascular haemolysis via type II hypersensitivity reaction: autoab vs RBC IgM on RBC in peripheries destroyed in reticuloendothelial system Lymphoproliferative, infections (eg. Mycoplasma) Mng: partial response to splenectomy Features of haemolysis Onset after 6m (when HbF gone) Arthralgia, dactylitis (most common presentation <2yrs; periosteal elevation on XR, painful swelling); bone thinning CCF; murmurs in 80% Jaundice, gallstones, AP, Hepatosplenomegaly (spleen small in adulthood due to recurrent infarction; functional asplenia); incr bil; jaundice; gallstones Leg ulcers Sepsis is most common cause of death in children, esp strep pneumoniae Vasoocclusive crises (MS, GI, RS, CNS, renal), CVA, pul infarction; acute chest syndrome Haematologic crises (splenic sequestration – 2nd most common cause of death, aplastic, infectious) Splenomegaly Reynaud’s disease and other symptoms of circulatory obstruction Livedo reticularis Worse in winter Features of haemolysis + Incr: LFT’s, plt Hb 6-9; HbF 2-20%; RBC survival 10-20/7 (instead of 120); reticulocytes 5-15% Haematuria; Sickle cells; Howell Jolly bodies For Mng: see Dunn Features of haemolysis + Incr: plt, WBC Haemaglobinuria Coombs positive More common than cold Splenomegaly Features of haemolysis + Acquired autoimmune haemolytic, warm Extravascular haemolysis via type II Microangiopathic haemolytic anaemia Intravascular haemolysis Features of haemolysis + DIC, TTP, HUS, prosthetic heart valves, malignant HTN, pre-eclampsia, Wegener’s granulomatosis, malignancy, HELLP, snake envenoming, vasculitis Irregularly fragmented RBC’s, Helmet cells RBC mechanical trauma Intravascular haemolysis (eg. March Hburia, cardiac valve, IABP) Features of haemolysis Other causes of Infections: Clostridia, CMV, coxsackie, EBV, haemophilus, herpes simplex, HIV, malaria, measles, mycoplasma, varicella, IMN Drugs: antimalarials, arsenic, bites, copper, lead, LA, nitrates, sulfonamides, ceftriaxone Autoimmune: incompatible b/ transfusion, SLE, RA, UC, hepatitis, lymphoma, CLL Haemolytic disease of the newborn: Rh of mother crosses placenta; need anti-D Features of haemolysis: haemolysis hypersensitivity reaction: autoab vs RBC IgG / complement or both on RBC destroyed in reticuloendothelial system 50% idiopathic; 50% 2Y (lymphoproliferative, post-infection, autoimmune, neoplasm, CT disorder, drugs (eg. Methyldopa, penicillin)) Paroxysmal nocturnal haemoglobinuria Intravascular haemolysis Others BM infiltration, congenital (eg. Fanconi’s syndrome, Diamond-Blackfan syndrome) Def of membrane proteins injury to BM stem cell pool autoimmune lysis of RBC, WBC + plt; functional WBC defect Incr: plt, WBC Coombs positive Predisposition to thrombosis (venous thrombosis in 20%, often prox) 5% become AML Mng: immunosupp; BM transplant may be curative Incr: LDH, unconjugated bil, reticuloctyes, mild MCV, RDW, urobilinogen, faecal stercobilinogen Decr: haptoglobin Heinz bodies In intravascular: methaemalbumin Features of haemolysis + Decr: WBC, plt, Fe Haemoglobinuria, urinary Fe; Acidosis