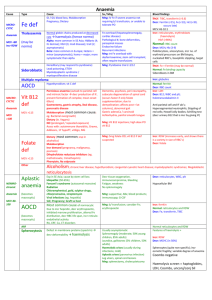
Anaemia
advertisement

Anaemia Fe Deficiency Aetiology: GI / GU blood loss; malabsorption; pregnancy; dietary Investigations: : TIBC, transferrin : ferritin, iron, Hct (occurs late) MCV: Hb 10:1 Management: IV iron if severe anaemia not requiring blood transfusion, or unable to tolerate PO Thalassaemia Aetiology: normal globin chains produced at decreased rate haemolysis Alpha: more common in SE Asia; HbBarts (4 intrauterine death); HbH (3 moderate disease); trait (2 asymptomatic) Beta: more common in Europe; hetero minor (asymptomatic); homo major; more symptomatic than alpha Symptoms: iron overload (hepatosplenomegaly, cardiac disease); pathological #; bone deformities; paraspinal masses; endocrine failure; recurrent infections Investigations: : reticulocytes, erythroblasts, HbF (>90%) Normal: RBC count : MCH; Hb (3-9) Poikilocytosis, anisocytosis, number of erythroid precursors on bone marrow biopsy; nucleated RBC’s; basophilic stippling; target cells Management: treat iron overload with desferrioxamine; stem cell transplant; often require transfusions Microcytic MCV <80 RDW Sideroblastic Macrocytic Aetiology: hereditary ; lead poisoning; ETOH; myelodysplastic / myeloproliferative disease Investigations: : iron; ferritin (may be normal) Normal: iron binding capacity Sideroblasts in bone marrow Management: pyridoxine trial 2-3/12 Multiple Myeloma Investigations: : globulins Anaemia of Chronic Disease Aetiology: hypothyroidism; vitamin C deficiency Investigations: normal: ferritin : RBC count Vitamin B12 Deficiency Aetiology: pernicious anaemia (autoantibodies to parietal cell and intrinsic factor production of intrinsic factor, prevent formation of complex; mean onset 60yrs); gastrectomy; gastric atrophy; ileal disease; pancreatic disease; malabsorption (most common cause); repeated and prolonged exposure to nitric oxide; associated with autoimmune thyroiditis, Graves, Addisons, primary hypoparathyroidism, vitiligo, myasthenia gravis Symptoms: dementia, psychosis, peripheral neuropathy, subacute degeneration of the spinal cord (occurs faster if only folate supplementation; due to demyelination; affects posterior and lateral columns); abnormal gait; gastric adenocarcinoma; carcinoid; achlorhydria; painful smooth tongue Investigations: : LDH : B12; WBC; platelets; holotranscolabalmin Antiparietal cell and intrinsic factor antibodies; hypersegmented neutrophils; stippling of red cells; Howell Jolly bodies; Schilling test ( urinary B12 that is by giving intrinsic factor) Management: vitamin B12 injections; high dose PO vitamin B12 MCV >100 Folate Deficiency Aetiology: dietary (most common; especially in alcoholics); malabsorption; demand (pregnancy, cancer, psoriasis); dihydrofolate reductase inhibitors (eg. Methotrexate, trimethoprim); phenytoin; sodium valproate Investigations: : RDW (increases early and shows there’s a variety in size of RBC’s) : folate Management: 5mg folate OD; vitamin B12 if deficiency suspected Macrocytic (cntd) Other Aplastic Anaemia Aetiology: especially in SE Asia; cause by stem cell loss; idiopathic (50-65%); Fanconi’s syndrome (autosomal recessive); radiation; chloramphenicol, gold, sulphur durgs, chlorpromazine, streptomycin; viral infections (eg. Hepatitis); SLE; pregnancy; GVHD Symptoms: tissue oxygenation; immunocompromise; bleeding; fatigue; weakness; no splenomegaly Investigations: : reticulocytes; WBC; platelets Hypocellular bone marrow; becomes macrocytic after time Management: supportive; antibiotics; blood products; immunosuppression; G-CSF Anaemia of Chronic Disease Aetiology: most common cause of normochromic; due to hepcidin, erythropoietin, inhibited marrow proliferation; altered Fe distribution; RBC life span; reticulo-endothelial activity; rheumatoid arthritis; CRF; cancer; connective tissue disorders Investigations: : ferritin Normal: reticulocytes and RDW : Fe; transferrin; TIBC Management: blood transfusion; consider Fe; erythropoeitin ARF Normochromic Alcoholism; chronic liver disease; hypothyroidism; congenital cyanotic heart disease; myelodysplastic syndromes; megaloblastic reticulocytosis Investigations: Normal reticulocytes and RDW Spherocytosis Aetiology: defect in membrane froteins (spectrin) deformability haemolysis Symptoms: usually asymptomatic; moderate splenomegaly (50% young children; 85% adults); jaundice; gallstones (5% children, 50% adults); haemolytic crises (usually during infections, mild); aplastic crises; leg ulcers; spinal cord lesions Investigations: : RDW : MCHC (in 50%) Spherocytes; osmotic fragility; variable degree of anaemia; Coombs negative; haemolysis screen = haptoglobins, LDH, Coombs, unconjugated and conjugated bilirubin; features of haemolysis +; urinary urobilinogen Management: splenectomy; cholecystectomy Elliptocytosis As per spherocytosis G6PD Deficiency Aetiology: X-linked inherited; more common in males; black; due to oxidative stress haemolysis; triggered by infection, sulphonamides, nitrofurantoin, antimalarials, vitamin K, aspirin Symptoms: splenomegaly; neonatal jaundice; gallstones Investigations: features of haemolysis; G6PD assay PK Deficiency Aetiology: autosomal recessive haemolysis Investigations: features of haemolysis Management: partial response to splenectomy MCV 80100 Acquired AutoImmune Haemolytic Aetiology: extravascular haemolysis due to type II hypersensitivity reaction causing RBC to be destroyed in reticuloendothelial system Warm: autoantibody vs igM on RBC in peripheries; due to lymphoproliferative infections (eg. Mycoplasma) Cold: autoantibody vs IgG / complement / both on RBC; 50% idiopathic; 50% secondary (lymphoproliferative, post-infection, autoimmune, neoplasm, connective tissue disorder, methyldopa, penicillin) Symptoms: splenomegaly; symptoms more common in warm; in cold also get Reynaud’s disease, livedo reticularis, worse in winter Investigations: features of haemolysis; platelets, WBC; Coomb’s positive Normochromic (cntd) MCV 80100 Sickle Cell Disease Aetiology: autosomal recessive; account for 70% congenital Hb disorders; especially in Black (occurs in 8%), Middle East, Indian; Defect in Hb production (valine/glycine) HbS polymerization when low NO concentration damage to membrane haemolysis, intracellular calcium, rigid RBC’s, activation of thrombosis Triggers: hypoxia, acidosis, 2,3,DPG, vascular stasis, IV volume depletion, infection, dehydration, altitude, cold Symptoms: Onset after 6 months (when HbF gone); Arthralgia, dactylitis (most common presentation <2yrs; periosteal elevation on XR, painful swelling); bone thinning; CCF; murmurs in 80%; Jaundice, gallstones, abdominal pain, Hepatosplenomegaly (spleen small in adulthood due to recurrent infarction; functional asplenia); incr bil; jaundice; gallstones; Leg ulcers; Sepsis is most common cause of death in children, especially strep pneumoniae Vasoocclusive crises (MS, GI, RS, CNS, renal), CVA, pulmonary infarction; acute chest syndrome Haematologic crises (splenic sequestration – 2nd most common cause of death, aplastic, infectious) Investigations: features of haemolysis; platelets, LFT’s; Hb 6-9; HbF 2-20%; RBC survival 1020/7 (instead of 120); reticulocytes 5-15%; Haematuria; Sickle cells; Howell Jolly bodies Management: see Dunn Mechanical Trauma Aetiology: intravascular haemolysis (eg. March Hburia, cardiac valve, IABP) Investigations: features of haemolysis Paroxysmal Nocturnal Hburia Aetiology: Intravascular haemolysis; Deficiency of membrane proteins injury to bone marrow stem cell pool autoimmune lysis of RBC, WBC + platelets; functional WBC defect Symptoms: Predisposition to thrombosis (venous thrombosis in 20%, often proximal); 5% become AML Investigations: features of haemolysis; WBC, platelets, iron; Hburia; urinary Fe; acidosis Management: immunosuppression; bone marrow transplant may be curative Other Haemolysis Aetiology: Infections: Clostridia, CMV, coxsackie, EBV, haemophilus, herpes simplex, HIV, malaria, measles, mycoplasma, varicella, IMN; Drugs: antimalarials, arsenic, bites, copper, lead, LA, nitrates, sulfonamides, ceftriaxone; Autoimmune: incompatible b/ transfusion, SLE, rheumatoid arthritis, ulcerative colitis, hepatitis, lymphoma, CLL; Haemolytic disease of the newborn: Rh of mother crosses placenta; need anti-D Investigations: features of haemolysis : LDH, unconjugated bilirubin, reticulocytes, mild MCV, RDW, urobilinogen, faecal stercobilinogen : haptoglobin Heinz bodies