Physiologically-based Pharmacokinetic Modeling of Target
Supplementary Information
Physiologically-based Pharmacokinetic Modeling of Target-Mediated
Drug Disposition of Bortezomib in Mice
Li Zhang · Donald E. Mager
Department of Pharmaceutical Sciences, University at Buffalo, State University of New York, NY
14214, USA
Corresponding Author:
Dr. Donald E. Mager
Department of Pharmaceutical Sciences,
University at Buffalo, State University of New York, Buffalo, NY, 14214
Tel: (716) 645-2903
Fax: (716) 829-6569
Email: dmager@buffalo.edu
1
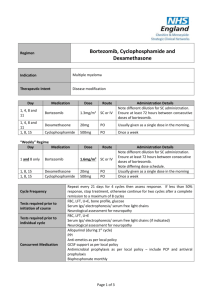
Table S1.
Final PK Parameters for Bortezomib in Humans
Tissue
Erythrocyte
Lung
Spleen
Liver
Kidney
Muscle
Bone
Remainder
Permeability
( PS )
L/hr
208.1
0.16
0.12
3.51
0.84
1.51
0.88
51.0
Target density
( R ti
) nM
349.8
107.4
275.7
315.0
146.2
8.60
48.12
970
Nonspecific
binding ( NS ) ti
--
7.57
2.54
3.68
1.54
9.60
1.17
1.06
96.76
Clearance
L/hr
7.5
--
--
--
--
--
--
0.15
2
.
Model validation
A model simulation was performed to assess the fidelity to which the final bortezomib PBPK model could recapitulate an independent dataset of bortezomib blood PK following a single intravenous (IV) dose (0.8 mg/kg) in mice [28]. The final PK parameters (Tables 2 and 3) were integrated with the bortezomib PBPK model to simulate the time-course of bortezomib blood concentrations. Figure S1 shows that the model simulations reasonably capture the reported bortezomib blood concentrations in mice.
10000
1000
100
0 5 10 15
Time (hr)
20 25 30
Fig. S1 . Model predicted and observed blood bortezomib concentration-time profile after
IV dosing of 0.8 mg/kg bortezomib in mice. Original data was extracted from the literature
(1). Symbols represent observed data (mean ± SD), and dashed line represents model simulated profile.
3
Sensitivity analysis
A sensitivity analysis of the final PBPK model was conducted using the Matlab toolbox
PottersWheel 2.0.59 [36, 37]. Sensitivity analysis was performed by simulating the model for
1000 times using the built-in 3-D sensitivity analysis method in PottersWheel, which evaluated the sensitivity of the mean concentrations of plasma and tissues with respect to all parameters perturbed simultaneously. The model parameters were perturbed by 10% of their nominal estimated values, and normalized sensitivity indices were assessed for each parameter in each tissue. Model output following perturbations in all parameters is shown in Figure S2. As expected, tissue output was primarily sensitive to the tissue target density, wherein the extent of bortezomib partitioning in each tissue was highly dependent on the capacity of proteasome in corresponding tissues. Moreover, tissue permeability coefficient terms exert a positive influence on corresponding tissue concentrations. As the drug-specific term, target binding affinity exerted a subtle influence on all the tissues. This could be attributed to the fact that the tissue drug concentrations were much higher than the K
D
nominal value, resulting in model outputs that were relatively insensitive to the K
D value.
4
Fig. S2 . Sensitivity analysis indices for the final PBPK model. X-axis consists of model parameters of target density, target binding affinity, nonspecific binding, and tissue permeability coefficient. Y-axis represents the output of each tissue in the model. The box on the right side of plot shows the range of the sensitivity index. The sensitivity index indicates the impact of the parameter on bortezomib concentrations in each tissue.
5
References
1. Kupperman E, Lee EC, Cao Y, Bannerman B, Fitzgerald M, Berger A, et al. Evaluation of the proteasome inhibitor MLN9708 in preclinical models of human cancer. Cancer Res.
2010;70(5):1970-80.
2. Maiwald T, Timmer J. Dynamical modeling and multi-experiment fitting with
PottersWheel. Bioinformatics. 2008;24(18):2037-43.
3. Mager DE, Mody V, Xu C, Forrest A, Lesniak WG, Nigavekar SS, et al. Physiologically based pharmacokinetic model for composite nanodevices: effect of charge and size on in vivo disposition. Pharm Res. 2012;29(9):2534-42.
6