File
advertisement
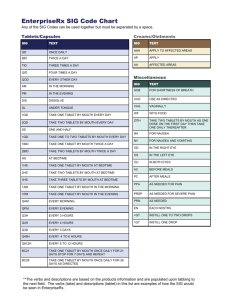
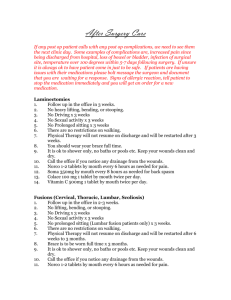
Congestive Heart Failure Riley’s Emergency By Stephanie Scott 1 Riley is a 12 year old, Cavalier King Charles spaniel that weighs 20 pounds. He presented to the clinic as an emergency. Patient recently went to the groomers and when he came home, he couldn’t stand and was having a hard time breathing. Patient has a history of congestive heart failure since 2012. The patient is currently on Lasix (Furosemide 20mg) 1 tablet by mouth (PO) twice a day (BID), Pimobendan (Vetmedin 5mg) ¾ tablet by mouth in the morning and ½ tablet my mouth at night every day for life and Enalapril 5mg 1 tablet by mouth (PO) twice a day (BID). His physical findings: Oral cavity: Mucous Membranes (MM): Pink, 2+ Tartar Eyes: Normal Ears: Normal Nose: Normal Lymph nodes: Normal Skin: Normal Cardiology: 4/6 Systolic Murmur Lungs: Very labored breathing, inspiratory dyspnea with crackles Abdomen: Normal Muscular Skeletal: Unable to stand Neurologic: Normal Upon examination, Riley is having labored breathing and suspect decompensated congestive heart failure. We have placed Riley on an oxygen mask and placed an intravenous catheter 22G Left cephalic. At 10:40AM. We gave the patient Lasix 45mg (0.9mL) intravenous, performed radiographs two views of the chest and noticed severe cardiomegaly and severe pulmonary edema. We also performed an Echocardiogram. The EKG presented with normal sinus rhythm with one atrial premature contraction; left atrial dilation; tall R waves consistent with left ventricle enlargement. Placed the patient in oxygen cage. The patient is sitting up and breathing more easily. Gave Pimobendan (Vetmedin) 5mg ½ tablet by mouth (PO), patient took readily with baby food. 1:40PM. Performed another echocardiogram which showed left atrium severely dilated, left ventricle mildly dilated; and mitral valves are thickened. 2 3:00PM Patient is resting comfortable in oxygen cage, and will take patient out of the oxygen cage to see how he does. Performed a Complete Blood Count (CBC), Chem 10, and electrolytes. Pack Cell Volume (PCV) at 46.5%, Blood Urea Nitrogen (BUN) at 29, Alanine transaminase (ALT) at 259, Alkaline Phosphatase (ALKP) at 585. 4:00PM Peripheral Capillary Oxygen Saturation (SpO2) is at 94%, Heart Rate (HR) is at 123 4:45PM Respiratory Rate (RR) is at 32, no longer hear crackles in lungs upon auscultation The patient has continued to improve the owners will take the patient home tonight to rest; will take to an animal emergency care if any problems occur. We will leave the catheter in place. We have increased Pimobendan (Vetmedin) 5mg to ¾ tablet by mouth (PO) three times a day (TID). Increased Lasix (diuretic) 20mg to 1 ½ tablet by mouth (PO) three times a day (TID). We have prescribed Spironolactone (aldosterone receptor antagonist) 25mg ½ tablet by mouth (PO) twice a day (BID) with a total of 30 tablets. Our plan is to recheck the patient tomorrow morning.