Mechanism of increasing airway resistance In Asthma - PBL-J-2015
advertisement

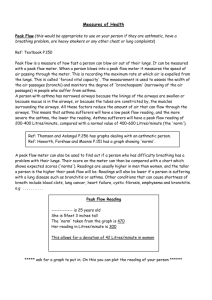
Mechanism of increasing airway resistance In Asthma Airways are ‘hypersensitive’ to specific stimuli which act as triggers causing bronchospasm, mucosal hypersecretion, oedema, epithelial and smooth muscular changes of the airways. *The varying clinical severity and chronicity of asthma is dependent on an interplay between airway inflammation and airway wall remodelling. This consists primarily of 2 stages: Early/immediate phase(bronchospasm) Late phase (inflammation) Stage 1: Stimulus triggers mast cells (with IgE attached as major factor responsible for binding to allergens) to activate spasmogens ( LTB4, LTC4, LTD4 , histamine and PGD2). These are powerful mediators that act on smooth muscle in the wall of the bronchioles. This causes a spasm of the bronchial smooth muscle and thus is responsible for the acute narrowing of the airways. Additionally, platelets and alveolar macrophages release other spasomgenic agents as well as additional mediators (chemotaxins/chemokines) which lead to the infiltration and activation of inflammatory cells (initiating the late phase response). Stage 2: Occurs in response to chemotactic agents that are released in the first phase and are responsible for the acute inflammatory reaction. Associated with the infiltration/activation of; eosinophils, neutrophils, platelets and monocytes/macrophages. This inflammatory response is characterised by vasodilatation, localised oedema in the walls of the small bronchioles (due to dilation of blood vessels for passage of immune cells) and secretion of thick mucus into the lumen of the airways. This is coupled by the spasm of the bronchiolar smooth muscle. Thus, airway resistance is increased greatly. A characteristic feature of chronic asthma is the alteration (remodelling) in structure/function of the airways which is the major factor responsible for increasing airway resistance in asthma. These structural changes interact with inflammatory cells and mediators and are responsible for the characteristic clinical features of asthma. Epithelial disruption with the shedding of epithelial cells in to the lumen of the airway contributes to airway obstruction. Thickening and metaplasia of the sub-epithelial reticular basement membrane results in an increase in the number/activity of mucus-secreting goblet cells. This causes a further narrowing of the lumen of the airway (remodelling) as well as increased levels of thick mucous into the airways causing further obstruction. Smooth muscle hyperplasia (due to increase growth factors) leads to further thickening of the wall of the airways. In addition to the increase in amount of, the smooth muscle has been shown in Asthma patients to alter in function by contracting more easily and for longer periods due to a change in actin-myosin crosslink cycling. This change allows the asthmatic airways to contract excessively as well as the least provocation. Asthmatic smooth muscle also secretes a wide range of cytokines and growth factors that help sustain the chronic inflammatory response. Lungs over a period of years become hyperinflated and this further causes a narrowing of the airways. As lung tissue grows the chest cage becomes permanently enlarged, causing a "barrel chest,” as seen in some patients. With this, both the functional residual capacity and lung residual volume become permanently increased. Bronchiolar diameter becomes more reduced during expiration than during inspiration in asthma, because complete bronchiolar collapse occurs during expiration as the outside of the bronchioles are compressed even more. This is also a reason as to why a wheeze in an asthmatic patient is more commonly heard on expiration. Bronchioles of the asthmatic lungs are already partially occluded; further occlusion resulting from the external pressure creates especially severe obstruction during expiration. That is, the asthmatic person often can inspire quite adequately but has great difficulty expiring. Clinical measurements show (1) greatly reduced maximum expiratory rate and (2) reduced timed expiratory volume. Note: Most asthmatics complain of greater difficulty during inspiration than expiration, due to the uncomfortable work of breathing necessary to ventilate hyperinflated, abnormally stiff, or noncompliant lungs? References: Kumar & Clark (2009) Clinical Medicine. Berger, E. AND Currie, G ( 2010) Asthma. Asthma Drugs Lecture by Professor Graham Nicholson CCS Lecture on Asthma by Dr. Charlotte Hespe Shim CS, Williams H Jr. Relationship of wheezing to the severity of obstruction in asthma. Arch Intern Med. 1983;143:890–92. [PubMed]