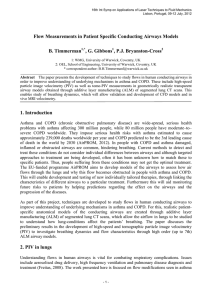
Flow Measurements in Patient Specific Conducting Airways Models:
advertisement

Flow Measurements in Patient Specific Conducting Airways Models: Towards Tailoring Treatment of Asthma and COPD http://www.airprom.european-lung-foundation.org/ http://www.airprom.eu B. Timmerman, G. Gibbons and P.J. Bryanston-Cross AirPROM In Silico Modelling The EU-funded programme AirPROM aims to develop models of human airways to assess how air flows through the lungs and why this flow becomes obstructed in people with asthma and Chronic Obstructive Pulmonary Disease (COPD). This will enable development and testing of new individually tailored therapies, through linking the characteristics of different airways to a particular treatment. Furthermore this will aid monitoring future risks to patients by helping predictions regarding the effect on the airways and the progression of the diseases. As part of this project techniques are developed to study flows in human conducting airways to improve understanding of underlying mechanisms in asthma and COPD. Realistic in silico airway models are created through additive layer manufacturing of segmented lung CT scans. Flow measurements are obtained in these models using (high-speed) particle image velocimetry (PIV). This enables study of breathing dynamics, which will allow validation and development of CFD models and in vivo MRI velocimetry. To understand how lung-conditions affect patients’ breathing, patient-specific in silico models of the conducting airways are created, which allow the airflow in lungs to be studied. For this, a patient’s CT data is segmented to extract the 3-dimensional shape of the airways. A model is then created of these airways using Additive Layer Manufacturing (ALM) techniques. Optically Transparent Models Two types of optically transparent RP models of conducting human airways have been created. Low order model Segmented CT: lower airways Segmented airway data was clipped down to 2nd order. This was used to produce a rapid-prototyped model constructed from water soluble support material (SR-30). After smoothing RP-layer surface imperfections the model was encapsulated by urethane rubber (Clear Flex® 50 water clear, Smooth-On Inc) with an estimated Young's modulus of ~2.47MPa, similar to that of the trachea and bronchial tubes. The core was then dissolved using an alkaline detergent (P400SC), leaving an optically transparent rectangular block with hollow passages in the shape of the airways. High order transparent model High order model To enable study of the effects of complex airway geometry a 7th order CT-based rigid transparent model was produced through standard RP. Compliant models Methodologies will be developed for the use of ALM techniques to provide flexible compliant boundary high-order airway physical models with an anatomically and mechanically-realistic description of the airway, based on bronchial tube tissue (muscle and cartilage) mechanical properties. This will make use of novel multi-material ALM technology (Objet Connex 260). Asthma: Patients suffering asthma have inflamed airways, making them swollen and very sensitive. When the airways react, mucus production increases and the muscles around airways tighten, narrowing them and thus causing less air to flow into the lungs. http://www.nhlbi.nih.gov Lung CT data. http://www.rad-zep.de COPD: COPD typically involves two separate lung conditions: chronic bronchitis and emphysema. In chronic bronchitis, the airways (bronchi) become inflamed, congested with mucus, and narrowed, resulting in obstructed air flow. In emphysema, the walls of the air sacs (alveoli) are destroyed, leading to fewer but larger alveoli, making them less efficient in transferring oxygen from the lungs to the bloodstream. High order model PIV: raw image, instantaneous and average 2C velocity Outlook Low order transparent model with RP core - High-speed PIV will be used to capture real time response of air flow to boundary movement, both on global large-scale as well as localised high-resolution, providing insight into ventilation dynamics and airflow mechanisms in human lungs in obstructive airway diseases. The integration of the large scale analysis with the local scale analysis will allow small scale effects on flow (e.g. reduced air flow due to partial closure of the middle lobar bronchus) to be correlated to an overall large-scale change in flow pattern (e.g. flow field in the trachea), thus providing a true macro-large airway CFD validation. Asthma and COPD Asthma and COPD are wide-spread, serious health problems with asthma affecting 300 million people, while 80 million people have moderate–to–severe COPD worldwide. They impose serious health risks with asthma estimated to cause approximately 239,000 deaths worldwide per year and COPD predicted to be the 3rd leading cause of death in the world by 2030 [1]. In people with COPD and asthma damaged, inflamed or obstructed airways are common, hindering breathing. Current methods to detect and treat these conditions do not consider individual differences between airways and although targeted approaches to treatment are being developed, often it has been unknown how to match these to specific patients. Thus, people suffering from these conditions may not get the optimal treatment. - Methods will be developed to obtain measurements for compliant opaque models, including endoscopic PIV, X-ray PIV [5] and digital holography [6]. - The in silico prototypes will be used for validation of ultrafast hyperpolarised 3He MRI, which has been shown to provide insight into in vivo ventilation dynamics in human lungs [7]. - With flow phantoms of known geometry and input flow rates and pressures that can be controlled, a direct means of validation of CFD calculations with well-defined experimental boundary conditions is provided. Low order model: 2C velocity Low order model: 3C velocity Airways tissue Segmented CT: lower and upper airways Particle Image Velocimetry References [1] AirPROM consortium website, http://www.airprom.european-lung-foundation.org or http://www.airprom.eu Illuminated model with dissolved core and diagram for PIV system Flows in human airways have been studied using CT-based silicone optically transparent rapid prototyped models with a water-glycerine mixture as the refractive index matched working fluid, generally aimed at improving artificial ventilation (e.g. [2]-[4]). In the experiments described here these techniques are investigated further using particle image velocimetry (PIV) to study the flow dynamics, based on patient specific breathing patterns. To minimise distortions due to refractive index differences here rapeseed oil is used as flow medium, enabling visualisation in the complex airway geometries. To enable velocity measurements the flow is seeded with reflective polyamide particles of 50 µm diameter. A light sheet is used to illuminate a plane or thin volume in the geometry. The movement of the particles is then recorded using a (high-speed) camera and velocities are extracted. By scanning the light sheet different parts of the airways can be investigated and the turbulent flow distribution through the complete airway geometry can be built up. [2] M. Vermeulen, C. van Holsbeke, T. Claessens, J. de Backer, P. van Ransbeeck, P. Verdonck, “Flow Analysis in Patient Specific Lower Airways using PIV", 15th Int Symp on Applications of Laser Techniques to Fluid Mechanics, Lisbon, Portugal, 05-08 July; 2010. [3] T. Soodt, F. Schröder, M. Klaas, T. van Overbrüggen and W. Schröder, “Experimental investigation of the transitional bronchial velocity distribution using stereo scanning PIV”, Experiments in Fluids, Online First 4May 2011. [4] S. Große, W. Schröder and M. Klaas, “Time-Resolved PIV Measurements of Vortical Structures in the Upper Human Airways”, Topics in Applied Physics, vol. 112,, pp. 35-53, 2008 [5] S. Dubsky, S.B. Hooper, K.K.W. Siu, A. Fouras, “Dynamic four-dimensional X-ray PIV of the lung”, 9th International Symposium on Particle Image Velocimetry –PIV’11, Kobe, Japan, July 21-23, 2011. [6] D. Claus, M. Fritzsche, D. Iliescu, B. Timmerman, and P. Bryanston-Cross, "High-resolution digital holography utilized by the subpixel sampling method", Applied Optics, Vol. 50, Issue 24, pp. 4711-4719, 2011 [7] J.M. Wild, M.N.J. Paley, L. Kasuboski, A. Swift, S.Fichele, N. Woodhouse, P.D. Griffiths, E.J.R. van Beek, “Dynamic radial projection MRI of inhaled hyperpolarized 3He gas”, Magn Reson Med 49:991–997, 2003 Acknowledgements: Olympus KeyMed Ltd., P. Hackett, C. Maske, A. Patronis, T. Bradbury, S. Final, D. Carter WMG/OEL School of Engineering, University of Warwick, Coventry, UK B.H.Timmerman@warwick.ac.uk, G.J.Gibbons@warwick.ac.uk, P.J.Bryanston-Cross@warwick.ac.uk