GASTROINTESTINAL PHYSIOLOGY
Chapter-I
(Gastrointestinal Secretions)
Ass. Prof. Dr. Emre Hamurtekin
EMU Faculty of Pharmacy
STRUCTURAL CONSIDERATIONS
STRUCTURAL CONSIDERATIONS
• The intestine has a very substantial surface
area for absorption.
• Sphincters:
– upper & lower esophageal sphincters
– pylorus
– ileocecal valve
– inner & outer anal sphincters
STRUCTURAL CONSIDERATIONS
• Throughout the small intestine, it is folded up into fingerlike
projections called villi.
• Crypts are the infoldings between the villi.
GASTROINTESTINAL SECRETIONS
•
•
•
•
•
Salivary secretion
Gastric secretion
Pancreatic secretion
Biliary secretion
Intestinal fluid
SALIVARY SECRETION
SALIVARY SECRETION
• Saliva is produced by 3 pairs of salivary glands:
– Parotid gland
– Submandibular gland
– Sublingual gland
• Constituents:
– Amylase (initiate digestion)
– IgA, lysozyme (protect oral cavity from bacteria)
– Mucin (lubricate the food)
• Saliva is hypotonic and alkaline
• Salivary secretion is almost entirely controlled by neural
influences:
– Parasympathetic*: most important role
– Sympathetic: composition of saliva (little influence on volume)
SALIVARY SECRETION
Chewing
Smelling/Seeing food
Nausea
Salivary secretion
Sleep
Fear
Fatigue
• Functions of saliva:
–
–
–
–
–
–
Facilitates swallowing
Initiates digestion
Keep the mouth moist
Solvent for molecules that stimulate the taste buds
Aids speech
Keep the mouth and teeth clean (mechanical&antibacterial)
GASTRIC SECRETION
ANATOMIC CONSIDERATIONS
ORIGIN & REGULATION
• Cephalic phase (before the meal is taken)
• Gastric phase (most significant)
• Intestinal phase (when the meal left the
stomach)
•
•
•
•
SECRETIONS: (fundus/body of stomach)
Surface mucous cells: mucus,
bicarbonate, trefoil peptide
Parietal cells: hydrocholoric acid, intrinsic
factor
ECL cell: histamine secretion
Chief cell: pepsinogen AND gastric lipase
ORIGIN & REGULATION
• There are 3 primary stimuli of gastric secretion:
– Gastrin
– Histamine
– Acetylcholine
• GASTRIN:
– Gastrin is a hormone released by G cells in the antrum of the stomach.
– It is released in response to,
a) GRP (bombesin) which is relesed from enteric nerve endings
b) oligopeptides in the gastric lumen.
– Carried to fundic glands by bloodstream
– Binds to receptors on parietal, chief cells(?) to activate secretion and also ECL
cells to activate histamine release
• HISTAMINE:
– Binds to H2 receptors on parietal cells and activate parietal cell secretion.
• ACETYLCHOLINE:
– Enteric nerve endings release acetylcholine
– Stimulates parietal and chief cells
ORIGIN & REGULATION
• During the cephalic phase of gastric secretion,
secretion is activated by vagal input originates from the
brain region.
• Vagal outflow to the stomach releases acetylcholine
and GRP initiating secretory function.
• Meal constituents trigger gastrin release + distension
of stomach activates strech receptors which provoke
vago-vagal and local reflexes that further amplify
gastric secretion.
• Somatostatin (released from antral D cells) inhibits
both G and ECL cells as well as parietal cell acid
secretion.
GASTRIC PARIETAL CELLS
GASTRIC PARIETAL CELLS
GASTRIC PARIETAL CELLS
Stomach Lumen
Ca
Acid secretion
cAMP
Ca
M3
H2
CCK-B
Ach
Histamine
Gastrin
Basolateral membrane
PANCREATIC SECRETION
ANATOMIC STRUCTURE
• Exocrine pancreas is a compound alveolar gland.
• Duct cells : secrete bicarbonate
– HCO3 is secreted in exchange for Cl (Cl / HCO3 exchanger)
• Exocrine cells : secrete enzymes
• Zymogen granules are formed in the cell and
discharged by exocytosis.
• The small duct radicles
pancreatic duct of
Wirsung
ampulla of Vater
duodenal
papilla (sphincter of Oddi)
• Duct of Santorini
PANCREATIC JUICE
• Pancreatic juice is alkaline and has a high bicarbonate
content.
• Most of the digestive enzymes in the pancreatic juice are
released in inactive forms.
• Trypsin is main the activator of most of the pro-enzymes.
• Acute pancreatitis !!!
• Secretion of pancreatic juice is primarily under hormonal
control:
– Secretin - rich in HCO3 and poor in enzymes
– CCK (cholecystokinin) – rich in enzymes but low in volume
• The effect of secretin is mediated by cAMP
• The effect of CCK is mediated by phospholipase C
• Neuronal control:
– Acetylcholine - cause discharge of zymogen granules
(mediated by phospholipase C)
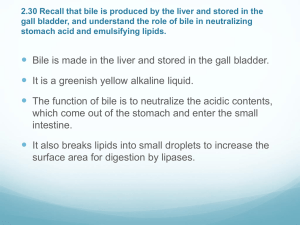
BILIARY SECRETION
BILIARY SECRETION
INTRODUCTION
FUNCTIONS:
• Digestion and absorption of fats (bile acids)
• Excretory fluid by which the body disposes of
lipid soluble end products of metabolism
lipid soluble xenobiotics
cholesterol (native or as bile acids)
BILE
• Bile is made up of bile acids, bile pigments, and other
substances dissolved in alkaline solution.
• Bilirubin and biliverdin pigments are responsible for
the color of the bile.
• Bile acids is the most important component in bile for
the digestion and absorption function of the biliary
secretion.
• 4 major bile acids in humans:
–
–
–
–
Cholic acid
Chenodeoxycholic acid
Deoxycholic acid
Lithocholic acid
primary (principle)
bile acids
BILE
Cholic acid
Colonic bacteria
Chenodeoxycholic acid
Deoxycholic acid
Colonic bacteria
Colonic bacteria
Ursodeoxycholic acid
Seconder bile acids:
Deoxycholic acid
Lithocholic acid
Ursodeoxycholic acid
Lithocholic acid
BILE
• Bile acids reduce
surface tension.
• Bile acids are
responsible for
emulsification of
fat preparatory to
its digestion and
absorption in the
small intestine
(form micelles).
BILE
• 90-95% of the bile acids are absorbed from small
intestine.
– Simple diffusion
– Na-bile salt co-transport system (terminal ileum)
• 5-10% are enter the colon and converted to
deoxycholic acid (absorbed back) and lithocholic acid
(mostly excreted in the stool)
• Absorbed bile acids are transported back to the
liver (enterohepatic circulation) and excreted
again in the bile.
Daily water turnover (ml) in GI tract
INGESTED
2000
ENDOGENOUS SECRETIONS
* Salivary glands
1500
* Stomach
2500
* Bile
500
* Pancreas
1500
* Intestine
1000
7000
TOTAL INPUT
2000 + 7000 = 9000
REABSORBED
* Jejunum
5500
* Ileum
2000
* Colon
1300
8800
BALANCE IN STOOL
9000 - 8800 = 200
INTESTINAL FLUID
• In the small intestine, secondary active
transport of Na is important in bringing about
absorption of glucose, amino acids and bile
acids.
• Presence of glucose in the intestinal lumen
facilitates Na reabsorption.
• Between meals, Na and Cl are absorbed
together by coupled activity of Na / H
exchanger and Cl / HCO3 exchanger.
ELECTRONEUTRAL NaCl ABSORPTION IN THE
SMALL INTESTINE and COLON
Apical
Basal
2K
H
Na, K
ATPase
NHE
3Na
Na
3Na
HCO3
CLD
Cl
Cl
Modified from Ganong’s Physiology
ELECTROGENIC Na ABSORPTION IN THE COLON
K
Na
Apical
2K
2K
Na, K
ATPase
3Na
Na
Na
Distal colon epithelium
Basal
Modified from Ganong’s Physiology
Daily water turnover (ml) in GI tract
INGESTED
2000
ENDOGENOUS SECRETIONS
* Salivary glands
1500
* Stomach
2500
* Bile
500
* Pancreas
1500
* Intestine
1000
7000
TOTAL INPUT
2000 + 7000 = 9000
REABSORBED
* Jejunum
5500
* Ileum
2000
* Colon
1300
8800
BALANCE IN STOOL
9000 - 8800 = 200
Cl SECRETION IN SMALL INTESTINE and COLON
2Cl Na
Cl
2Cl
Cl
Lumen
K
Na
K
Na, K
ATPase
Na
K
Modified from Ganong’s Physiology
THE END