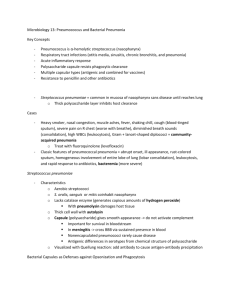
Case Study: Pneumonia Content produced by the Alliance for the
advertisement
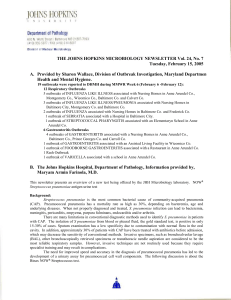
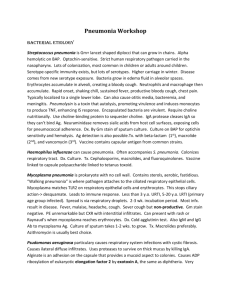
Case Study: Pneumonia Content produced by the Alliance for the Prudent Use of Antibiotics (APUA) through an unrestricted educational grant from Alere Inc. Reported by: Shira Doron, MD, Assistant Professor, Division of Infectious Diseases, Associate Hospital Epidemiologist, Antimicrobial Management, Tufts Medical Center, Boston, MA Kirthana Beaulac, PharmD, Clinical Pharmacy Specialist- Infectious Diseases and Antimicrobial Stewardship, Tufts Medical Center, Boston, MA Patient Background: RP is a 68 year-old male who was admitted to the hospital from his long-term care facility after 1 week of dyspnea and cough. He was seen by a staff physician at the long-term care facility and was diagnosed with a COPD exacerbation. He was prescribed azithromycin, but has not improved after 3 days of antibiotics. He has a history of dyslipidemia, COPD, alcoholic cirrhosis, and HTN. He routinely takes lisinopril, atorvastatin, tiotropium and fluticasone/salmeterol, and has recently had a heavier reliance on his rescue albuterol inhaler. Review of systems reveals fever, chills, cough (sometimes productive) and dyspnea (worse than baseline). Radiology: Chest X-ray showed focal consolidation in the right lower lobe, suggestive of pneumonia. Diagnosis: Upon admission, RP was initially given the broad spectrum antibiotics vancomycin, piperacillin/ tazobactam, and tobramycin for the treatment of healthcare-associated pneumonia (HCAP).1 At that time, he had blood and sputum cultures taken. Upon being seen by the internist on hospital day one, he had urinary antigen tests performed for pneumococcus and legionella. When the test results returned with a positive pneumococcal antigen test, he was deescalated to ceftriaxone and completed a 7 day course of antibiotics. Given RP’s exposure to multi-drug resistant organisms at his long-term care facility, consensus guidelines dictate that he receive broad empiric pneumonia therapy with two anti-pseudomonal agents and an anti-staphylococcal agent.1 This regimen covers most of the potential pathogens that can potentially cause healthcare associated pneumonia (HCAP), and relies heavily on microbiologic cultures for de-escalation. In situations, like RP’s, in which microbiologic cultures cannot identify a causative pathogen, alternative microbiologic testing, like urinary antigen tests can be informative and provide opportunities to de-escalate therapy. Pneumococcal Urinary Antigen Test: “The pneumococcal urinary antigen test is a useful method for detecting pneumococcus, especially in patients who are unable to produce a reliable respiratory sample or those who are already on antibiotics.” The pneumococcal urinary antigen test is a useful method for detecting pneumococcus, especially in patients who are unable to produce a reliable respiratory sample or those who are already on antibiotics.2 RP provided a sputum culture that was significantly contaminated with squamous epithelial cells, suggesting that if a pathogen grew, it would have to be interpreted as a potential contaminant from the patient’s oral flora. Furthermore, he had been on antibiotics for several days, which likely would have penetrated into his sputum sample to inhibit bacterial growth on the culture media. The pneumococcal urinary antigen test (pUAT) is a useful diagnostic tool, especially in patients who have high risk of pneumococcal pneumonia. Guidelines recommend performing pUAT in patients requiring intensive care admission, those who have failed outpatient antibiotic therapy, leucopenia, active alcohol abuse, chronic severe liver disease, asplenia, or pleural effusion.2 It is a relatively simple and rapid test to perform, requiring only a urine specimen from the patient and taking only 15 minutes. It has a demonstrated specificity of >90%, but is relatively insensitive (70-80%).3-5 It maintains specificity after several days of antimicrobial therapy.6Concentration of the urine prior to testing may enhance the sensitivity, but may decrease the specificity.7 Costs: The cost of treating HCAP is highly variable, depending on the agent chosen. The cost could range from $50-$300 per day of therapy.1 With the pUAT costing approximately $30, de-escalating therapy can produce a significant cost savings, plus provide an opportunity to avoid further exposure to broad- spectrum antibiotics. Furthermore, when a three-drug regimen is changed to a single-drug regimen, the patient benefits from the lower risk of adverse events potential drug reactions. The pUAT also has utility in the treatment of CAP. Because of the need to cover both typical and atypical organisms, the recommended treatment for CAP is either fluoroquinolonemonotherapy or a beta-lactam plus macrolide. The fluoroquinolone and macrolide drugs classes are both known to be cardiotoxic drugs, potentially prolonging the QT interval, which can lead to sudden cardiac death.8 An opportunity to discontinue one of those agents and use beta-lactam monotherapy for pneumococcus may limit the incidence of these adverse cardiac events. References 1. Niederman, M.S.et al. (2005) Guidelines for the Management of Adults with Hospital-acquired, Ventilatorassociated, and Healthcare-associated Pneumonia. Am J RespirCrit Care Med. 2005; 171; 388-416. 2. Mandell, L.A.et al. (2007) Infectious Diseases Society of America / American Thoracic Society Consensus Guidelines on the management of Community-Acquired Pneumonia in Adults. ClinInf Dis. 2007; 44S27-72. 3. Dominguez, J.et al. (2001) Detection of Streptococcus pneumonia antigen by a rapid immunochromatographic assay in urine samples. Chest.2001; 119:243–9. 4. Yu, V.L.et al. (2000) Evaluation of the Binax urinary gram stain and sputum culture for Streptococcus pneumoniae in patients with community-acquired pneumonia. Clin Infect Dis 2000; 32: 258. 5. Murdoch, D.R.et al. (2001) Evaluation of a rapid immunochromatographic test for detection of Streptococcus pneumonia antigen in urine samples from adults with community-acquired pneumonia.J ClinMicrobiol.2001; 39:3495–8. 6. Smith, M.D.et al.(2003) Rapid diagnosis of bacteremic pneumococcal infections in adults by using the Binax NOW Streptococcus pneumoniae urinary antigen test: a prospective, controlled clinical evaluation. J ClinMicrobiol.2003; 41:2810–3. 7. Stralin, K. (2008) Usefulness of aetiological tests for guiding antibiotic therapy in community-acquried pneumonia. Int J Antimicrob Agents.2008; 31: 3-11. 8. Ray, W.A. et al. (2012) Azithromycin and the Risk of Cardiovascular Death. NEJM. 2012; 366; 1881-1890.