Microbiology 13
advertisement

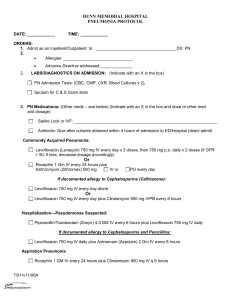
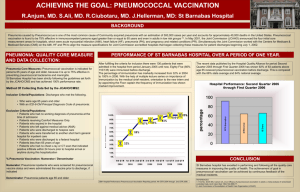
Microbiology 13: Pneumococcus and Bacterial Pneumonia Key Concepts - Pneumococcus is α-hemolytic streptococcus (nasopharynx) Respiratory tract infections (otitis media, sinusitis, chronic bronchitis, and pneumonia) Acute inflammatory response Polysaccharide capsule resists phagocytic clearance Multiple capsular types (antigenic and combined for vaccines) Resistance to penicillin and other antibiotics - Streptococcus pneumoniae = common in mucosa of nasopharynx sans disease until reaches lung o Thick polysaccharide layer inhibits host clearance Cases - - Heavy smoker, nasal congestion, muscle aches, fever, shaking chill, cough (blood-tinged sputum), severe pain on R chest (worse with breathe), diminished breath sounds (consolidation), high WBCs (leukocytosis), Gram + lancet-shaped diplococci = communityacquired pneumonia o Treat with fluoroquinolone (levofloxacin) Classic features of pneumococcal pneumonia = abrupt onset, ill appearance, rust-colored sputum, homogeneous involvement of entire lobe of lung (lobar consolidation), leukocytosis, and rapid response to antibiotics, bacteremia (more severe) Streptococcus pneumoniae - Characteristics o Aerobic streptococci o S. oralis, sanguis or mitis coinhabit nasopharynx o Lacks catalase enzyme (generates copious amounts of hydrogen peroxide) With pneumolysin damages host tissue o Thick cell wall with autolysin o Capsule (polysaccharide) gives smooth appearance -> do not activate complement Important for survival in bloodstream In meningitis -> cross BBB via sustained presence in blood Nonencapsulated pneumococci rarely cause disease Antigenic differences in serotypes from chemical structure of polysaccharide o Visualized with Quellung reaction: add antibody to cause antigen-antibody precipitation Bacterial Capsules as Defenses against Opsonization and Phagocytosis - - Other encapsulated organisms = Str. pneumoniae (pneumococcus), pyogenes (group A strep), agalactiae (group B strep), Staph. aureus, Neisseria meningitides (meningococcus), H. influenza, Klebsiella pneumonia, E. coli, Bacteroides fragilis, Cryptococcus neoformans (fungi) o H. influenza and Neisseria meningitidis with pneumococcus are most frequent cause of bacterial meningitis Complement system (lytic complex) highly efficient in eliminating extracellular bacteria o Pneumococcus require complement + phagocytes via opsonization but polysaccharide capsule doesn’t activate complement sans antibody Other components of innate immune system opsonize pneumococci Epidemiology - Pneumococcal pneumonia = most common form of bacterial pneumonia acquired in community o High in children (<5), adults (>40), blacks, Native Americans, impoverished and debilitated, sickle cell anemia, alcoholism, Hodgkin disease, multiple myeloma, HIV infection, absence of spleen o Seasonal, winter and early spring o May cause otitis media, acute sinusitis, chronic bronchitis, peritonitis, endocarditis, septic arthritis, meningitis Encounter - Reservoir of S. pneumonia = humans (majority never have symptoms) o Step 1: colonization of nasopharynx May remain in carrier state or progress to disease (strain virulence and host defense determine outcome) Incidence declines with age Different serotypes due to serotype-specific immune response limiting reacquisition of same serotype o Transmission through airborne droplets (person-to-person) Entry - Lungs usually protected by 1) tortuous path, 2) epiglottis, 3) cough reflex, 4) mucus and cilia, 5) alveolar macrophages o Affected by unconscious aspiration, cigarette smoke, alcohol, virus or excess fluid Spread, multiplication and damage - Stage 1: serous fluid in alveoli Stage 2: early consolidation (neutrophil and RBCs in alveoli) o Chemotactic signals (from complement path) - - Some may have type-specific anticapsular antibodies opsonizing organism for phagocytosis o interaction of C-reactive protein (CRP) (acute phase reactant) with phosphorylcholine on pneumococcal surface -> activates complement cascade Stage 3: late consolidation (victorious neutrophils, few bacteria) o Affected lung heavy = hepatization Stage 4: resolution (neutrophils replaced by macrophages) o Most cases, architecture of lung restored to normal Complications = pleural effusion, empyema (purulent infection of pleural space), spread to blood and distal (bacteremia) o Direct seeding of blood from nasopharynx = occult bacteremia Humoral factors assist spleen, liver, and lymph nodes in filtering function Diagnosis - Leading cause of lobar pneumonia, acute otitis media, chronic bronchitis, and acute sinusitis Gram stain sputum = 10 lancet-shaped Gram + diplococcic and neutrophils Antipneumococcal antibiotic = levofloxacin Blood agar = α-hemolysis Sensitivity to Optochin and soluble in bile salts Definitive if found in blood sample Treatment and Prevention - Penicillin, erythromycin -> treatment fails because of rapid progression of infection (lyse cell wall -> short-term increased inflammation) Mild drug resistance can still use penicillin unless in CNS (3/4 of strains) High resistant strains -> cannot use other β-lactams, macrolides, and sulfas, use levofloxacin Penicillin-binding proteins confer resistance to penicillin o Selective pressure from antibiotic presence + adaptation (transformation) Antigenic diversity barrier to vaccine development o Vaccine developed for common serotypes (elderly and predisposed individuals) Hodgkin disease and multiple myeloma pts (at risk) don’t make adequate antibody to vaccine Contains capsular polysaccharide o Pneumococcal conjugate vaccine = use in children (contains bacteria itself)