Complicated Pneumonia in the Developed World

Complicated Pneumonia in the developed world
Eitan Kerem
Department of Pediatrics and CF Center, Hadassah University Hospital, Jerusalem,
Israel
Community- acquired pneumonia (CAP) is a leading cause of morbidity and mortality, especially in children under 5 years of age. The annual incidence of pneumonia in North American and European children under 5 years of age is approximately 36 per 1000. The microbiological diagnosis of pneumonia in childhood is complex and in most cases the cause is unknown. There is no standard diagnostic test for an etiologic agent in childhood pneumonia. Young children often cannot produce sputum, and tracheal aspirate or lung biopsies are not practical or necessary for the routine evaluation of pneumonia. Viral etiology is most common in young children and decreases with age. Streptococcus pneumoniae is the single most common bacterial cause across all age groups. Haemophilus influenzae ,
Staphylococcus aureu s and Moraxella catarrhalis are less commonly identified as causative organisms.
In the recent years there are reports of increasing incidence of community acquired methicillin resistance Staph as an important cause of pneumonia and complicated pneumonia in children. Atypical organisms present similarly across all age groups and may be more common than previously recognized. The use of new diagnostic methods such as immunological techniques and polymerase chain reaction has proven invaluable for specific diagnosis and epidemiological investigation, showing adequate sensitivity, specificity and promptness of results, with the aim of guiding therapy properly. Therefore, it is not possible yet to differentiate between viral and bacterial pneumonia by chest radiography or inflammatory markers, so the clinician has to treat this group of children empirically with antibiotics.
Complications associated with pneumococcal pneumonia include the development of necrotizing pneumonia, pleural effusion, pleural empyema, and lung abscess.
An increase in the incidence of pleural empyema was reported for the first time in a retrospective cohort study of 50 children hospitalized in Ohio between 1988 and 1994, showing that 34% of cases had occurred in the last 12 months. The same
phenomenon was then reported by many studies in the United States and in Europe.
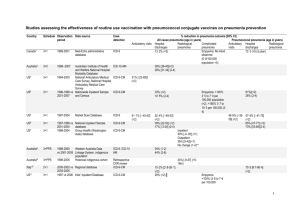
Although the incidence of invasive pneumococcal disease has decreased since the use of pneumococcal conjugated vaccine (PCV), developed countries such as USA have seen an emergence of empyema and necrotizing pneumonia episodes caused by nonvaccine serotypes . Between 1995 and 2003, the rate of pleural empyema steadily rose from 14 to 26 per million pediatric hospital admissions in the UK. The prevalence of parapneumonic empyema was shown to increase from 22% in 1994 to
53% in 1999 amongst pneumonia cases caused by S. pneumoniae in eight American hospitals. Of the 50 cases of pleural empyema that occurred from 1988 to 1994 at a pediatric hospital in Cincinnati 17 (34%) occurred within the last 12 months of the study, 40% of the cases were caused by S pneumoniae . Many authors also reported an increase in pneumonia associated lung abscesses and cavitations. The reasons for this increase in the prevalence of suppurating complications in children with pneumonia have not been clearly identified. Suppurating complications were associated with age, recent chicken pox, infection with S. pneumoniae (especially serotype 1), and therapy with antibiotics and non-steroidal anti-inflammatory drugs (NSAIDs) prior to hospital admission.
Necrotizing pneumonia, also termed massive ulmonary gangrene, is a sequela of pneumonia in which the lung tissue becomes necrotic. Recent attention has focused on pneumococcal pneumonia as a causative agent in children, where with limited intervention the prognosis is good. Accumulation of fluid in the pleural space may follow the development of pneumonia in as many as 28% of children. The successful management of such fluid—which may either represent a parapneumonic effusion or be contaminated with micro-organisms, leukocytes, and fibrin to form an empyema, is a crucial component of the overall care of these patients. Controversy exists regarding the appropriate management strategy for empyema or complicated parapneumonic effusion in children. Current options include primary chest tube placement (either open or with radiologic guidance) or video-assisted thoracoscopic surgery (VATS) with removal of pleural fluid and exudate. Primary chest tube drainage may be favored by some clinicians because of the perceived advantages of radiographic drainage for localized fluid collections, avoidance of general anesthesia, and the smaller thoracostomy tubes used. However, the fibrinous pleural fluid in the setting of empyema often clogs these small drains, resulting in inadequate drainage. Intrapleural
administration of fibrinolytics may augment drainage, although this measure is not helpful in all cases. Open placement may lead to suboptimal placement of the tip of the tube. These shortcomings have led to the use of primary VATS-assisted drainage of the pleural space in pediatric patients with empyema and parapneumonic effusion.
A VATS-based approach offers the potential for better lung expansion after removal of pleural debris and exudate, excellent magnified vision, optimization of the location of the chest tube, and reduced chest wall and muscle trauma compared with traditional thoracotomy.
The management of children with pneumonia is generally based on the age of the patient and the clinical presentation. Initial antibacterial therapy for CAP is usually empirical, as culture and antibacterial sensitivity test results are rarely available at initial diagnosis. Any agent selected for empirical therapy should have good activity against the pathogens commonly associated with CAP, a favorable tolerability profile, and be administered in a simple dosage regimen for good compliance. Because S. pneumoniae is the most common bacterial cause of pneumonia and its associated complications, current guidelines for antibacterial of
CAM recommend that the initial treatment will be directed to eradicate this microorganism. Narrow-spectrum antibiotics are advocated in the first instance.
Inappropriate use of antibiotics can result in treatment failure and adverse drug reactions, and contribute to emerging pathogen resistance. Consideration of a drug's pharmacodynamic and pharmacokinetic properties is also important. Agents with low maximum plasma or tissue concentrations and long half-lives may be more likely to expose bacteria to resistance-selective concentrations. The strategy of administration is also important; low doses of beta-lactams and long treatment duration are risk factors for the carriage of pneumococci non-susceptible to penicillin, whereas shortcourse, high-dose therapy minimizes this risk. Convenience and tolerability are also essential considerations in pediatrics.
For non-severe pneumonia, oral amoxicillin is the antibacterial of choice with low failure rates reported. Randomized controlled trials in children in the developing and in the developed countries showed that in previously well children oral amoxicillin and IV benzyl penicillin have equivalent efficacy for the treatment of pneumonia. Both were successful in curing children with CAP.
Pneumococcal isolates not susceptible to penicillins and third-generation cephalosporins have been well described in vitro, and rates between 10% and 40%
have been reported from worldwide surveillance. There is significant geographical variation, with high rates in Spain, France and parts of south-east Asia and the USA.
Furthermore, macrolide resistance is also a problem in some communities. The main mechanism of resistance is via the alteration of penicillin-binding proteins, which can be overcome by achieving adequate local drug levels; i.e. it is a decreased sensitivity rather than an absolute resistance. There is as yet no evidence of clinical treatment failure of infections outside the central nervous system using high-dose penicillin.
Since most pneumococci remain sensitive to high-dose penicillin-based antibacterials amoxicillin or penicillin remains the antibiotic of choice in pneumococcal pneumonia.
The emergence and spread of resistance to commonly used antibiotics has challenged the management of CAP. Multiple sets of CAP guidelines have been published to address the continued changes in this complex disease. Severely ill children are traditionally treated with parenteral antibacterials. It has been shown that penicillin resistant pneumococci were not associated with more severe disease. It has been shown that penicillin resistance is not a factor in outcome from invasive S. pneumoniae community-acquired pneumonia.
Pneumococcal macrolide resistance is mediated via alteration of the 50S ribosomal binding site, thereby preventing binding and the subsequent inhibition of bacterial protein synthesis. A second mechanism is via the presence of efflux pumps for the antibiotic. It is often associated with penicillin non-susceptibility. Rates of usage and resistance of the newer macrolides have substantially increased over recent times and vary by geographical region. There are reports of treatment failure of pneumococcal disease using macrolides alone; thus, this approach is not recommended.
If parenteral therapy is required and pneumococcus is the likely pathogen, benzylpenicillin or an aminopenicillin can be used. Broader-spectrum agents have no additional benefit. For the severely unwell, toxic child with or without effusions, where rarer pathogens are a possibility, or in the rare scenario of high pneumococcal penicillin resistance (mean inhibitory concentration >2 mg/l), therapy should include a third-generation cephalosporin (e.g. ceftriaxone) with a macrolide if atypical agents are potential pathogens, or a penicillinase-resistant beta-lactam (e.g. oxacillin) or vancomycin if Staphylococcus aureus or MRSA infection is likely. However, treating all children with CAM with these antibiotics may change the micrflora of pneumonia
causing bacteria and increase the rate of infections with other less common and more resistant microorganisms.