Bordon et al. Outcomes & inflammatory responses in bacteremic
advertisement

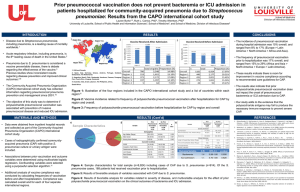
Bordon et al. Outcomes & inflammatory responses in bacteremic pneumococcal pneumonia DATA SUPPLEMENT Bacteremic Pneumococcal Pneumonia: Clinical Outcomes and Inflammatory Response MATERIALS AND METHODS FOR FUNCTIONAL STUDIES Study Design This was a pilot prospective observational study of hospitalized patients with pneumococcal CAP at the University of Louisville Hospital and the Louisville’s Veteran Administration Hospital from 01/04/2011 to 01/08/2012. The University of Louisville Human Subjects Program Protection Office and the Robley Rex Veterans Affairs Medical Center Institutional Review Boards approved this study prior to any data collection (Approvals #: 07.0182 and 0009, respectively). Inclusion Criteria/Criteria for CAP: CAP was defined based on evidence of a new pulmonary infiltrate at chest radiograph associated with at least one of the following: 1) new or increased cough; 2) fever or hypothermia; and 3) leukocytosis, left shift, or leucopenia. Patients with CAP were included in this study following previous written consent. The inclusion and exclusion criteria and full case report forms for this study can be found at the Community Acquired Pneumonia Organization study site at www.caposite.com. Exclusion Criteria: Patients were excluded if suffering from an unstable psychiatric or psychological condition rendering the subject unlikely to be cooperative or to complete the study requirements, or if they had a medical history that, in the investigator’s opinion, precluded subject compliance with the protocol. Patients that received corticosteroids were excluded from this study. 1 Bordon et al. Outcomes & inflammatory responses in bacteremic pneumococcal pneumonia Study groups: The study group included only pneumococcal CAP (CAP) patients. Pneumococcal CAP diagnosis was based on sputum or blood cultures positive for Streptococcus pneumoniae and/or positive urine pneumococcus antigen. The identification of microorganisms and susceptibility testing were performed according to standard methods as described in the main text of the manuscript. Out of a total of ten patients, four had positive blood cultures (all samples taken on admission) whereas the other six were diagnosed based on positive urinary pneumococcal antigen. Healthy Control Group: In order to compare results of the plasma cytokines and neutrophil functional assays from CAP patients with those of healthy individuals, blood samples were also obtained from a control group (n=12) of healthy adult donors (approved by the University of Louisville’s IRB #191.06). Plasma samples Blood samples were obtained on the day of admission and on every other day during the patients’ stay at the hospital. Venous blood was collected using sodium citrate Vacutainer tubes. Following centrifugation at 300 x g for 10 min, the plasma was separated by aspiration, aliquoted and stored frozen at -80oC until assayed. Cytokine measurements The concentrations of interleukin (IL)-1β, IL-1 Receptor Antagonist (IL-1RA), IL-6, CXCL8 (IL-8), IL-10, IL-12p40, IL-17, interferon (IFN)γ, tumor necrosis factor (TNF)α, CXCL10 (IP10) in plasma samples were determined using Milliplex MAP Multiplex kits (EMD Millipore, Billerica, MA). Following thawing, plasma and processed sputum samples were centrifuged at 10,000xg for 5 minutes and the supernatants used in the assay according to the manufacturer’s instructions. 2 Bordon et al. Outcomes & inflammatory responses in bacteremic pneumococcal pneumonia Neutrophil functional studies Neutrophil functional assays were performed using whole blood samples. Basal or formylmethionyl-leucyl-phenylalanine (fMLF)-stimulated exocytosis were determined by measuring the plasma membrane expression of secretory vesicles (CD35) and specific granules (CD66b) (antibodies E11 and G10F5, respectively, both from Biolegend, San Diego, CA) on a FACSCalibur instrument (Becton Dickinson, Franklin Lakes, NJ). Following antibody treatment, red cells were lysed with BD red cell lysis buffer (Beckton Dickinson), followed by two washes with 0.05% sodium azide, and fixation in 1% paraformaldehyde before analysis. Phagocytosis and phagocytosis-stimulated respiratory burst activity were measured using a flow cytometric assay based on the production of H2O2 stimulated by the phagocytosis of Staphylococcus aureus, as previously described [10]. Briefly, neutrophils (2 x 106 cells/ml) were incubated with 2’,7’-dichlorofluorescein diacetate (0.5 µM final concentration) for 10 min at 37oC. Then, 50 µl aliquots of the cell suspension were sampled before and 10 min after the addition of opsonized, propidium iodidide-labelled Staphylococcus aureus (at a final concentration of 108 bacteria/ml). After fixation in 1% paraformaldehyde, the cells were then analyzed for phagocytosis and H2O2 production by flow cytometry on a FACSCalibur instrument. Statistics Statistical analysis was performed using GraphPad Prism 5.0 (GraphPad Software, La Jolla, CA) and R version 2.15 (www.r-project.org). All cytokine and neutrophil data are presented as the medians ± SEM. 3 Bordon et al. Outcomes & inflammatory responses in bacteremic pneumococcal pneumonia Data supplement FIGURE 1a. Kaplan–Meier curve for length of hospital stay (LOS) for non-ICU patients among non-bacteremic and bacteremic patients with S. pneumoniae community-acquired pneumonia. 4 Bordon et al. Outcomes & inflammatory responses in bacteremic pneumococcal pneumonia Data supplement FIGURE 1b. Kaplan–Meier curve for length of hospital stay (LOS) for ICU patients among non-bacteremic and bacteremic patients with S. Pneumoniae community-acquired pneumonia. 5 Bordon et al. Outcomes & inflammatory responses in bacteremic pneumococcal pneumonia Data supplement FIGURE 2. Neutrophil functional studies in bacteremic and nonbacteremic patients with pneumococcal CAP. Neutrophil function profiles in bacteremic (open squares) and non-bacteremic (closed circles) pneumococcal CAP patients. Peripheral blood neutrophils were assayed for basal and fMLF-stimulated expression of CD35 and CD66b, as well as for phagocytosis and respiratory burst activity. 6 Bordon et al. Outcomes & inflammatory responses in bacteremic pneumococcal pneumonia Data supplement TABLE 1. Demographic and clinical characteristics of S. pneumoniae CAP patients with and without bacteremia used in inflammatory responses and biomarker studies. Bacteremia No Bacteremia Total n =4 n=6 n = 10 Age> 65 1 (25) 4 (67) 5 (50) Age, Median (IQR) 60 (22) 72 (21) 64 (22) Male Gender 3 (75) 6 (100) 9 (90) Nursing Home Resident 0 (0) 0 (0) 0 (0) Smoking 1 (25) 3 (50) 4 (40) Neurologic Diseases 1 (25) 0 (0) 1 (10) Cerebrovascular Diseases 2 (50) 0 (0) 2 (20) CHF 2 (50) 2 (33) 4 (40) COPD 3 (75) 2 (33) 5 (50) Diabetes mellitus 1 (25) 4 (67) 5 (50) HIV 0 (0) 0 (0) 0 (0) Acute Renal Diseases 0 (0) 0 (0) 0 (0) Chronic Renal Diseases 0 (0) 2 (33) 2 (20) Hepatic Diseases 0 (0) 0 (0) 0 (0) Neoplastic Diseases 0 (0) 1 (17) 1 (10) Hyperlipidemia 2 (50) 2 (33) 4 (40) Statin Therapy 1 (25) 2 (33) 3 (30) Immunosuppression 0 (0) 0 (0) 0 (0) Variable Demographics Past Medical History Vaccination 7 Bordon et al. Outcomes & inflammatory responses in bacteremic pneumococcal pneumonia Previous Flu vaccine 1 (25) 4 (67) 5 (50) Previous Pneumococcal vaccine 1 (25) 4 (67) 5 (40) Altered Mental Status 0 (0) 1 (50) 1 (10) Pleural Effusion 2 (50) 2 (33) 4 (40) ICU Admission 4 (100) 2 (33) 6 (60) Prior CAP 1 (25) 1 (17) 2 (20) PSI ≥ 4 3 (75) 3 (50) 6 (60) Macrolide Therapy 1 (25) 2 (33) 3 (30) Early TCS (< 3 days) 2 (50) 6 (100) 8 (80) In-Hospital Mortality 0 (0) 0 (0) 0 (0) 30-day Mortality 0 (0) 0 (0) 0 (0) 30-day Rehospitalization 0 (0) 0 (0) 0 (0) Clinical Findings TCS, Time to Clinical Stability; IQR, Interquartile; PSI, Pneumonia Severity Index; CAP, Community Acquired Pneumonia. Results expressed as number (%) or median (interquartile). 8 Bordon et al. Outcomes & inflammatory responses in bacteremic pneumococcal pneumonia Data supplement TABLE 2. Clinical and laboratory findings of S. pneumoniae CAP patients with and without bacteremia used in inflammatory responses and biomarker studies. Bacteremia No Bacteremia Total n =4 n=6 n = 10 98.4 (1.9) 98.8 (3.8) 98.6 (2.5) Respiratory Rate 20 (5) 20 (9) 20 (5) Heart Rate 80 (30) 94 (28) 93 (26) Systolic BP 128 (71) 118 (61) 125 (53) ABG PaO2 60.8 (35) 65.9 (16) 61.5 (11.3) ABG Ph 7.4 (0.2) 7.5 (0.1) 7.5 (0.1) Albumin 3.5 (1.6) 3.6 (0.9) 3.6 (0.9) BUN 25 (41) 17 (22) 22 (19) Glucose 109 (223) 114 (92) 112 (92) BNP 524 (1003) 68 (127) 94 (502.7) CRP 277 (368) 85 (84) 110 (322) Procalcitonin 50 (14.3) 0.6 (1.0) 22 (53.2) 83 (7) 92 (13) 87 (12) 187 (51) 252 (82) 216 (74) 12.4 (12.3) 12.9 (6.7) 12.9 (6.7) Na 133 (9) 136 (6) 134 (6) Hematocrit 39 (11) 38 (5) 39 (5) Hemoglobin 13.0 (4.2) 12.6 (2.5) 13.0 (2.5) Variable Clinical Findings Temperature (oral) Laboratory Findings Neutrophils Platelets WBC 9 Bordon et al. Outcomes & inflammatory responses in bacteremic pneumococcal pneumonia Time to Clinical Stability (TCS) 4 (5) 2 (0) 2 (1) Length of hospital stay 4 (4) 4 (11) 4 (5) Pneumonia severity index 4 (2) 4 (2) 4 (2) Results expressed as median (interquartile range). ABG, Arterial Blood Gas; PaO2, partial oxygen pressure; BNP, brain natriuretic peptide; BUN, blood urea nitrogen; CRP, C-reactive protein; WBC, white cell blood count; RR, respiratory rate; HR, heart rate; BP, blood pressure; TCS, time to clinical stability; LOS, length of stay; PSI, pneumonia severity index 10