- Flintbox
advertisement

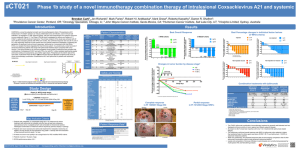
Epidermal Growth Factor and Checkpoint Blockade Therapy of Cancer (Case #: 2014-105) Background Melanoma is the most aggressive form of skin cancer, projected to cause over 9,500 deaths in the United States this year. Effective immune-based treatments and molecularly targeted therapies have improved the overall outcome of patients. A new approach to cancer therapy is the use of checkpoint blockade monoclonal antibodies, such as ipilimumab, which enhances the immune response to cancer. Ipilimumab is a fully humanized antibody directed against cytotoxic T-lymphocyte antigen-4 (CTLA-4), which serves as an immune checkpoint that functionally removes a key modulator of the immune system. Tumorspecific cellular immunity is thereby enhanced by promotion of the T cells and, possibly, a reduction of intratumoral regulatory T cells. Ipilimumab is approved at a dose of 3 mg/kg for use against melanoma in more than 40 countries, and was approved for use in the US in March 2011. Two important unmet areas of need related to checkpoint blockade therapy include the need to predict which patients will respond to checkpoint blockade, and the ability to enhance patient responsiveness and sensitivity. Description Researchers at The University of Iowa have been working to explore these unmet needs. Using serum samples of melanoma patients, elevated levels of Epidermal Growth Factor (EGF) were discovered. EGF is a cytokine that correlates with a clinical response to ipilimumab. The researchers found adding EGF to lymphocytes increased CTLA-4 expression, a molecule which is a target for ipilimumab, by T regulatory cells (Tregs). CTLA-4 is an immune-inhibitory molecule expressed in activated T cells and in suppressor T regulatory cells. Interaction of the monoclonal antibody with CTLA-4 blocks inhibitory signals generated through this receptor and enhances T cell activation, leading to increased antitumor responses. The research findings suggest elevated levels of EGF increases CTLA4 expression by Tregs, which allows binding in greater amounts of ipilimumab to Tregs, ultimately enhancing efficacy of checkpoint blockade therapy – and therefore cancer treatment. Advantages This discovery could have a significant impact on cancer immunotherapy in two ways: (1) Elevated levels of EGF could be used as a biomarker to indicate the likelihood that a given cancer patient will respond to ipilimumab or other checkpoint blockade antibodies. These antibodies have significant toxicities and are very expensive, so predicting whether or not a patient is likely to respond to ipilimumab or other antibodies could be very valuable; (2) The ability to induce increased expression of CTLA4 by Tregs could enhance sensitivity to ipilimumab. This could be done by signaling through the EGF receptor that is expressed by the Tregs. Thus, treatment with EGF or another agonist could be used to improve response to checkpoint blockade therapy. Relevant Research/Publications 1) Kaehler, K.C., Piel, S., Livingstone, E., Schilling, B., Hauschild, A., & Schadendorf, D. Update on immunologic therapy with anti–CTLA-4 Antibodies in Melanoma: Identification of clinical and biological response patterns, immune-related adverse events, and their management. Seminars in Oncology, Vol 37, 5: 485-498 (2010). 2) Graziani, G., Tentori, L. & Navarra, P. Ipilimumab: A novel immunostimulatory monoclonal antibody for the treatment of cancer. Pharmacological Research 65 9– 22 (2012). 3) Giulio Tosti, G., Cocorocchio, E., & Pennacchioli, E. Anti-cytotoxic T lymphocyte antigen-4 antibodies in melanoma. Clinical, Cosmetic and Investigational Dermatology 6: 245–256 (2013). 4) Wolchok, J.D., Hodi, F.S., Weber, J.S. et al. Development of ipilimumab: A novel immunotherapeutic approach for the treatment of advanced melanoma. Ann. N.Y. Acad. Sci. 1291: 1–13 (2013). *Many other references available upon request