Path Page 79-108 Tissue Renewal, Regeneration, and Repair
advertisement
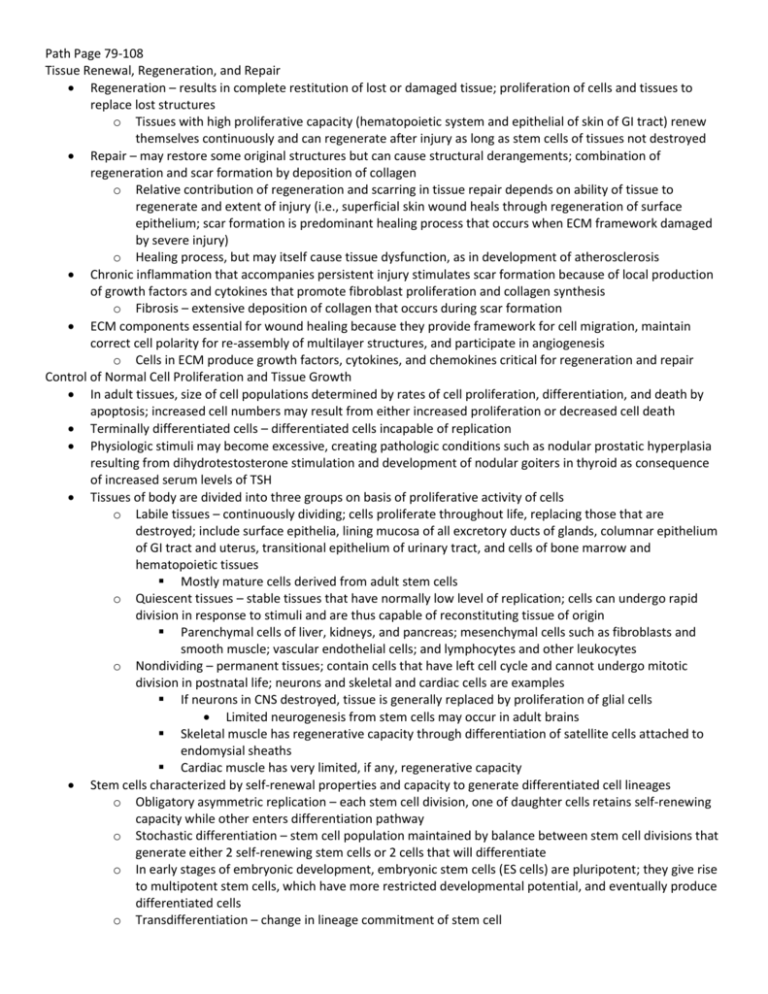
Path Page 79-108 Tissue Renewal, Regeneration, and Repair Regeneration – results in complete restitution of lost or damaged tissue; proliferation of cells and tissues to replace lost structures o Tissues with high proliferative capacity (hematopoietic system and epithelial of skin of GI tract) renew themselves continuously and can regenerate after injury as long as stem cells of tissues not destroyed Repair – may restore some original structures but can cause structural derangements; combination of regeneration and scar formation by deposition of collagen o Relative contribution of regeneration and scarring in tissue repair depends on ability of tissue to regenerate and extent of injury (i.e., superficial skin wound heals through regeneration of surface epithelium; scar formation is predominant healing process that occurs when ECM framework damaged by severe injury) o Healing process, but may itself cause tissue dysfunction, as in development of atherosclerosis Chronic inflammation that accompanies persistent injury stimulates scar formation because of local production of growth factors and cytokines that promote fibroblast proliferation and collagen synthesis o Fibrosis – extensive deposition of collagen that occurs during scar formation ECM components essential for wound healing because they provide framework for cell migration, maintain correct cell polarity for re-assembly of multilayer structures, and participate in angiogenesis o Cells in ECM produce growth factors, cytokines, and chemokines critical for regeneration and repair Control of Normal Cell Proliferation and Tissue Growth In adult tissues, size of cell populations determined by rates of cell proliferation, differentiation, and death by apoptosis; increased cell numbers may result from either increased proliferation or decreased cell death Terminally differentiated cells – differentiated cells incapable of replication Physiologic stimuli may become excessive, creating pathologic conditions such as nodular prostatic hyperplasia resulting from dihydrotestosterone stimulation and development of nodular goiters in thyroid as consequence of increased serum levels of TSH Tissues of body are divided into three groups on basis of proliferative activity of cells o Labile tissues – continuously dividing; cells proliferate throughout life, replacing those that are destroyed; include surface epithelia, lining mucosa of all excretory ducts of glands, columnar epithelium of GI tract and uterus, transitional epithelium of urinary tract, and cells of bone marrow and hematopoietic tissues Mostly mature cells derived from adult stem cells o Quiescent tissues – stable tissues that have normally low level of replication; cells can undergo rapid division in response to stimuli and are thus capable of reconstituting tissue of origin Parenchymal cells of liver, kidneys, and pancreas; mesenchymal cells such as fibroblasts and smooth muscle; vascular endothelial cells; and lymphocytes and other leukocytes o Nondividing – permanent tissues; contain cells that have left cell cycle and cannot undergo mitotic division in postnatal life; neurons and skeletal and cardiac cells are examples If neurons in CNS destroyed, tissue is generally replaced by proliferation of glial cells Limited neurogenesis from stem cells may occur in adult brains Skeletal muscle has regenerative capacity through differentiation of satellite cells attached to endomysial sheaths Cardiac muscle has very limited, if any, regenerative capacity Stem cells characterized by self-renewal properties and capacity to generate differentiated cell lineages o Obligatory asymmetric replication – each stem cell division, one of daughter cells retains self-renewing capacity while other enters differentiation pathway o Stochastic differentiation – stem cell population maintained by balance between stem cell divisions that generate either 2 self-renewing stem cells or 2 cells that will differentiate o In early stages of embryonic development, embryonic stem cells (ES cells) are pluripotent; they give rise to multipotent stem cells, which have more restricted developmental potential, and eventually produce differentiated cells o Transdifferentiation – change in lineage commitment of stem cell o Adult stem cells have more restricted capacity to generate different cell types; exist in lining of gut, cornea, and hematopoietic tissue Somatic stem cells reside in special microenvironments (niches) composed of mesenchymal, endothelial, and other cell types Niche cells generate or transmit stimuli that regulate stem cell self-renewal and generation of progeny cells Differentiated cells can be reprogrammed into pluripotent cells by transduction of genes encoding ES cell transcription factors; these called induced pluripotent stem cells (iPS cells) Inner cell mass of blastocysts in early embryonic development contains ES cells; these can be maintained in culture as undifferentiated cell lines or be induced to differentiate into specific lineages o ES cells used for study of specific signals and differentiation steps, knockout genes for disease models or knock-in models with a mutated DNA sequence replacing endogenous sequence Differentiated cells of adult tissues can be reprogrammed to become pluripotent by transferring their nucleus to an enucleated oocyte, which is then implanted in a surrogate mother and can generate cloned embryos that develop into complete animals (reproductive cloning; first demonstrated on Dolly the sheep) Therapeutic cloning – nuclear transfer to oocytes for treatment of diseases; nucleus of skin fibroblast from patient introduced into enucleated human oocyte to generate ES cells, which are kept in culture and induced to differentiate into various cell types Both forms of cloning are inefficient and often inaccurate because of deficiency in histone methylation in reprogrammed ES cells, which results in improper gene expression iPS cells – fibroblasts that have been reprogrammed into pluripotent cells by transduction of genes involved in pluripotency (Oct3/4, Sox2, c-myc, Kfl4, Nanog, Lin28); able to generate cells of any germ layer; may become source of cells for patient-specific stem cell therapy without involvement of nuclear transfer to oocytes o Kfl4 and c-myc are oncogenes, so probably not wise for long-term use Somatic stem cells – present in tissues that continuously divide; may also be present in organs that do not actively produce differentiated cell lineages o Transit amplifying cells – rapidly dividing cells generated by somatic stem cells; lost capacity of selfperpetuation and give rise to cells with restricted developmental potential (progenitor cells Developmental plasticity – capacity of a cell to transdifferentiate into diverse lineages o Hemopoietic stem cells (HSCs) experimented on for developmental plasticity; can migrate to sites of inflammation and injury, where they generate innate immune cells or release growth factors and cytokines that promote repair and cell replication through paracrine effect Bone marrow – contains HSCs and stromal cells (aka, multipotent stromal cells, mesenchymal stem cells, or MSCs) o HSCs generate all blood cell lineages, can reconstitute bone marrow after depletion caused by disease or irradiation, and are widely used for treatment of hematologic diseases; can be collected directly from bone marrow, from umbilical cord blood, and from peripheral blood of individuals receiving cytokines such as granulocyte-macrophage colony-stimulating factor, which mobilize HSCs o MSCs – multipotent; have potentially important therapeutic applications because they can generate chondrocytes, osteoblasts, adipocytes, myoblasts, and endothelial cell precursors depending on tissue to which they migrate; migrate to injured tissue and generate stromal cells or other cell lineages (don’t participate in normal tissue homeostasis) Liver – contains stem cells/progenitor cells in canals of Hering (junction between biliary ductular system and parenchymal hepatocytes; cells in this niche give rise to population of precursor cells (oval cells) which are bipotential progenitors (capable of differentiating into hepatocytes or biliary cells) o Liver stem cells function as secondary or reserve compartment activated only when hepatocyte proliferation blocked o Oval cell proliferation and differentiation prominent in livers of patients recovering from fulminant hepatic failure, in liver tumorigenesis, and in some cases of chronic hepatitis and advanced cirrhosis Brain – neurogenesis from neural stem cells (NSCs) occurs in brain of adults; NSCs capable of generating neurons, astrocytes, and oligodendrocytes o NSCs identified in subventricular zone (SVZ) and dentate gyrus of hippocampus Skin – stem cells located in hair follicle bulge, interfollicular areas of surface epidermis, and sebaceous glands o o Bulge area of hair follicle – constitutes niche for stem cells that produce all of cell lineages of hair follicle Interfollicular stem cells – scattered individually in epidermis and not contained in niches; divide infrequently but generate transit amplifying cells that generate differentiated epidermis o Bulge stem cells – contribute to replenishment of surface epidermal cells after skin wounding but not during normal homeostasis; activation regulated by stimulatory signals from Wnt pathway and inhibition of signaling from BMP system Intestinal epithelium – in small intestine, crypts are monoclonal structures derived from single stem cells (villus differentiated compartment that contains cells from multiple crypts o Wnt and BMP pathways important in regulation of proliferation and differentiation o Stem cells may be located immediately above Paneth cells in small intestine or at base of crypt (colon) Skeletal muscle – myocytes don’t divide even after injury; growth and regeneration of injured skeletal muscle occur by replication of satellite cells o Satellite cells located beneath basal lamina and can generate differentiated myocytes after injury o Active Notch signaling – triggered by upregulation of delta-like (Dll) ligands, stimulating proliferation of satellite cells Cornea – transparency of cornea depends on integrity of outermost corneal epithelium, which is maintained by limbal stem cells (LSCs), which are located at junction between epithelium of cornea and conjunctiva o LSC deficiency leads to corneal opacification and can be treated by limbal transplantation or LSC grafting o May be possible to correct loss of photoreceptors that occurs in degenerative diseases of retina by transplanting retinal stem cells Cell Cycle and Regulation of Cell Replication Replication of cells stimulated by growth factors or by signaling from ECM components through integrins o To achieve DNA replication and division, cell goes through cell cycle, which has presynthetic (G1), DNA synthesis (S), premitotic (G2), and mitotic (M) phases o G0 – quiescent cells that have not entered cell cycle o Each cell cycle phase dependent on proper activation and completion of previous one o G1 and S phases have activators and inhibitors and sensors responsible for checkpoints Quiescent cells must go through transition from G0 to G1 (first decision step which acts as a gateway to cell cycle); transition involves transcriptional activation of large set of genes, including various proto-oncogenes and genes required for ribosome synthesis and protein translation Cells in G1 progress through cycle and reach critical stage at G1/S transition (restriction point), which is ratelimiting step for replication o Progression tightly regulated by proteins (cyclins) and associated enzymes (cyclin-dependent kinases or CDKs); CDKs acquire catalytic activity by binding to and forming complexes with cyclins o Activated CDKs in complexes drive cell cycle by phosphorylating proteins critical for cell cycle transitions o Retinoblastoma susceptibility (RB) protein – normally prevents cells from replicating by forming tight, inactive complex with transcription factor E2F Phosphorylation of RB causes its release, which activates E2F and allows it to stimulate transcription of genes whose products drive cells through cycle o Activity of cyclin-CDK complexes regulated by CDK inhibitors; some growth factors shut off by them Checkpoints – surveillance mechanisms embedded in cell cycle that are geared primarily at sensing damage to DNA and chromosomes o G1/S checkpoint monitors integrity of DNA before replication o G2/M checkpoint checks DNA after replication and monitors whether cell can safely enter mitosis o When cells sense DNA damage, checkpoint activation delays cell cycle and triggers DNA repair mechanisms; if DNA damage too severe to be repaired, cells eliminated by apoptosis or enter senescence (primarily through p53-dependent mechanisms) o Checkpoint defects that allow cells with DNA strand breaks and chromosome abnormalities to divide produce mutations in daughter cells that may lead to neoplasia Growth factors – polypeptides that drive proliferation of many cell types; can have restricted or multiple cell targets; can promote cell survival, locomotion, contractility, differentiation, and angiogenesis o o o o o o All growth factors function as ligands that bind to specific receptors, which deliver signals to target cells; signals stimulate transcription of genes that may be silent in resting cells, including genes that control cell cycle entry and progression Epidermal growth factor (EGF) and TGF-α – share common receptor (EGFR) and belong to EGF family EGF – mitogenic for variety of epithelial cells, hepatocytes, and fibroblasts; widely distributed in tissue secretions and fluids In healing wounds of skin, EGF produced by keratinocytes, macrophages, and inflammatory cells that migrate into area TGF-α – involved in epithelial cell proliferation in embryos and adults, and in malignant transformation of normal cells to cancer EGFR1 (best known EGFR) responds to EGF, TGF-α, HB-EGF (heparin-binding), and amphiregulin EGFR1 mutations and amplification detected in cancers of lung, head, neck, breast, glioblastomas, and other cancers ERB B2 receptor (main ligand not identified yet) is overexpressed in subset of breast cancers and is important therapeutic target Hepatocyte growth factor (HGF) – previously called scatter factor; has mitogenic effects on heaptocytes and most epithelial cells, including cells of biliary epithelium and epithelial cells of lungs, kidney, mammary gland, and skin Acts as morphogen in embryonic development, promotes cell scattering and migration, and enhances survival of hepatocytes Produced by fibroblasts and most mesenchymal cells, endothelial cells, and liver nonparenchymal cells Produced as inactive single-chain form (pro-HGF) that is activated by serine proteases released in damaged tissues Receptor (c-MET) often highly expressed or mutated in tumors, especially in renal and thyroid papillary carcinomas Signaling required for survival during embryonic development (without it, defects develop in muscles, kidney, liver, and brain) Platelet-derived growth factor (PDGF) – family of proteins, each consisting of 2 chains PDGF-AA, PDGF-AB, and PDGF-BB secreted as biologically active molecules PDGF-CC and PDGF-DD require extracellular proteolytic cleavage to release active growth factor All PDGF isoforms exert effects by binding 2 cell surface receptors (PDGFR α and β), which have different ligand specificities PDGF stores in platelet granules and released on platelet activation Produced by variety of cells, including activated macrophages, endothelial cells, smooth muscle cells, and many tumor cells Causes migration and proliferation of fibroblasts, smooth muscle cells, and monocytes to areas of inflammation and healing skin wounds PDGF-B and C participate in activation of hepatic stellate cells in initial steps of liver fibrosis and stimulate wound contraction Vascular endothelial growth factor (VEGF) – family of homodimeric proteins that include VEGF-A (VEGF), VEGF-B, VEGF-C, VEGF-D, and PIGF (placental growth factor) Potent inducer of vasculogenesis and has central role in angiogenesis in adults (promotes angiogenesis in chronic inflammation, healing of wounds, and tumors) Heterozygote VEGF knockouts die during embryonic development as result of defective vasculogenesis and hematopoiesis VEGFR-1, VEGFR-2, and VEGFR-3 are tyrosine kinase receptors VEGFR-2 located in endothelial cells and is main receptor for vasculogenic and angiogenic effects of VEGF VEGFR-1 has role in inflammation VEGF-C and VEGF-D bind to VEGFR-3 and act on lymphatic endothelial cells to induce production of lymphatic vessels (lymphangiogenesis) Fibroblast growth factor (FGF) – FGF-1 is acidic and FGF-2 is basic (20+ members total) FGFs transduce signals through tyrosine kinase receptors (FGFRs 1-4) FGF-1 binds to all receptors FGF-7 – keratinocyte growth factor Released FGFs associate with heparan sulfate in ECM, which can serve as reservoir for storage of inactive factors FGFs contribute to wound healing responses, hematopoiesis, angiogenesis, development, and other processes Wound repair – FGF-2 and FGF-7 contribute to epithelialization of skin wounds Angiogenesis – FGF-2 has ability to induce new blood vessel formation Hematopoiesis – differentiation of specific lineages of blood cells and development of bone marrow stroma Development – skeletal and cardiac muscle development, lung maturation, and specification of liver form endodermal cells o TGF-β and related growth factors – 3 isoforms of TGF-β and many other factors with wide-ranging functions (BMPs, activins, inhibins, and müllerian inhibiting substance) TGF-β1 has most widespread distribution and is often called just TGF-β; produced by platelets, endothelial cells, lymphocytes, and macrophages Native TGF-β synthesized as precursor protein, which is proteolytically cleaved to yield biologically active growth factor and second latent component Active TGF-β binds to 2 cell surface receptors (types I and II) with serine/threonine kinase activity and triggers phosphorylation of cytoplasmic transcription factors (Smads) Smads form heterodimers with Smad 4, which enter nucleus and associate with other DNAbinding proteins to activate or inhibit gene transcription TGF-β is pleiotropic (has multiple effects) Growth inhibitor for most epithelial cells – blocks cell cycle by increasing expression of cell cycle inhibitors of Cip/Kip and INK4/ARF families; can promote invasion and metastasis during tumor growth; loss of TGF-β receptors frequently occurs in tumors, providing proliferative advantage to tumor cells; TGF-β expression may increase in tumor microenvironment, creating stromal-epithelial interactions that enhance tumor growth and invasion Stimulates fibroblast chemotaxis and enhances production of collagen, fibronectin, and proteoglycans; TGF-β inhibits collagen degradation by decreasing matrix proteases and increasing protease inhibitor activities; TGF-β involved in development of fibrosis in variety of chronic inflammatory conditions particularly in lungs, kidney, and liver; high TGF-β expression occurs in hypertrophic scars, systemic sclerosis, and Marfan syndrome Strong anti-inflammatory effect but may enhance some immune functions; knockouts have defects in regulatory T cells leading to widespread inflammation with abundant Tcell proliferation and CD4+ differentiation into TH1 and TH2 helper cells; TGF-β enhances development of IL-17-producing T cells (TH17) that are involved in autoimmune tissue injury; TGF-β stimulates production of IgA in gut mucosa o Cytokines – some can be considered growth factors because they have growth-promoting activities for variety of cells TNF and IL-1 participate in wound healing reactions TNF and IL-6 involved in initiation of liver regeneration Receptor-mediated signal transduction – activated by binding of ligands (such as growth factors) and cytokines to specific receptors o Different classes of receptor molecules and pathways initiate cascade of events by which receptor activation leads to expression of specific genes o Paracrine signaling affects adjacent cells, and endocrine signaling is across the body o Signaling typically involves clustering of 2 or more receptor molecules by ligand o Receptors typically located on surface of target cell but can be found in cytoplasm or nucleus Receptors with intrinsic tyrosine kinase activity – ligands include EGF, PDGF, VEGF, FGF, TGF-α, and insulin; receptors in this family have extracellular ligand-binding domain, transmembrane region, and cytoplasmic tail that has intrinsic tyrosine kinase activity Binding of ligand induces dimerization of receptor, tyrosine phosphorylation, and activation of receptor tyrosine kinase Active kinase phosphorylates (activates) many downstream effector molecules (molecules that mediate effects of receptor engagement with ligand) Activation of effector molecules can be direct or through involvement of adapter proteins; prototypical adapter protein is GRB-2, which binds GTP-GDP exchange factor (SOS); SOS acts on GTP-binding (G) protein RAS and catalyzes formation of RAS-GTP, which triggers MAP kinase cascade Active MAP kinases stimulate synthesis and phosphorylation of transcription factors, such as FOS and JUN; transcription factors activated by cascade stimulate production of growth factors, receptors for growth factors, and proteins that directly control entry of cells into cell cycle Effector molecules activated by these receptors are PLCγ and PI3K o PLCγ catalyzes breakdown of membrane inositol phospholipids into inositol 1,4,5-triphosphate (IP3), which functions to increase concentrations of calcium, and diacylglycerol, which activates serine-threonine kinase protein kinase C that activates various transcription factors o PI3K phosphorylates membrane phospholipid, generating products that activate Akt, which is involved in cell proliferation and cell survival through inhibition of apoptosis Alterations in tyrosine kinase activity and receptor mutations detected in cancer Receptors lacking intrinsic tyrosine kinase activity that recruit kinases – ligands include IL-2, IL-3, other interleukins; interferons α, β, and γ; erythropoietin; granulocyte colony-stimulating factor; GH; and prolactin Receptors transmit extracellular signals to nucleus by activating members of JAK family of proteins; JAKs link receptors with and activate cytoplasmic transcription factors (STATs), which directly shuttle into nucleus and activate gene transcription Cytokine receptors can also activate MAP kinase pathways and other pathways G-protein-coupled receptors – transmit signals into cell through trimeric GTP-binding proteins (G proteins); contain 7 transmembrane α helices and constitute largest family of receptors Ligands include chemokines, vasopressin, serotonin, histamine, epinephrine and norepinephrine, calcitonin, glucagon, PTH, corticotropin, and rhodopsin Lots of pharmaceutical drugs target these receptors Binding of ligand induces conformational changes in receptor, causing activation and allowing interaction with many different G proteins Activation of G proteins occurs by exchange of GDP with GTP Many branches of signal transduction pathway involve calcium and 3’,5’-cAMP as second messengers Activation of G protein-coupled receptors can produce IP3, which releases calcium from ER, and calcium signals have target cytoskeletal proteins, chloride and potassiumactivated ion pumps, enzymes such as calpain, and calcium-binding proteins such as calmodulin cAMP activates protein kinase A and cAMP-gated ion channels, important in vision and olfactory sensing Inherited defects associated with retinitis pigmentosa, corticotropin deficiencies, and hyperparathyroidism Steroid hormone receptors – generally located in nucleus and function as ligand-dependent transcription factors Ligands diffuse through PM and bind inactive receptors, causing their activation Activated receptor binds to specific DNA sequences (hormone response elements) in target genes or can bind to transcription factors Other ligands that bind to this receptor family include thyroid hormone, vitamin D, and retinoids Peroxisome proliferator-activated receptors – nuclear receptors involved in adipogenesis, inflammation, and atherosclerosis Transcription factors that regulate cell proliferation include products of growth-promoting genes (such as c-MYC and c-JUN), and products of cell cycle-inhibiting genes (such as p53) o Transcription factors have modular design and contain domains for DNA binding and for transcriptional regulation; transactivating domain stimulates transcription of gene o Growth factors induce synthesis or activity of transcription factors o Cellular events requiring rapid responses rely on post-translational modifications that lead to activation Heterodimerization – used by dimerization of product of proto-oncogenes c-FOS and c-JUN to form transcription factor AP-1, which is activated by MAP kinase signaling pathways Phosphorylation – used by STATs Release of inhibition to permit migration into nucleus – used for NF-κB Release from membranes by proteolytic cleavage – used by Notch receptors Mechanisms of Tissue and Organ Regeneration Inadequacy of true regeneration in mammals is due to absence of blastema formation (source of cells for regeneration) and rapid fibroproliferative response after wounding o Wnt/β-catenin pathway functions instead to modulate stem cell functions in intestinal epithelium, bone marrow, and muscle; participate in liver regeneration after partial hepatectomy; and stimulate oval cell proliferation after liver injury Liver regeneration is not true regeneration because resection of tissue does not cause new growth but instead triggers process of compensatory hyperplasia in remaining parts of organ Kidney, pancreas, adrenal glands, thyroid, and lungs of very young can undergo compensatory growth o New nephrons cannot be generated in adult kidney, so growth of contralateral kidney after unilateral nephrectomy involves nephron hypertrophy and some replication of proximal tubule cells o Pancreas has limited capacity to regenerate exocrine components and islets; regeneration of beta cells involves beta-cell replication, transdifferentiation of ductal cells, or differentiation of putative stem cells that express transcription factors Oct4 and Sox2 Resection of about 60% of liver results in doubling of liver remnant in about a month o Portions of liver that remains after partial hepatectomy constitute intact mini-liver that rapidly expands and reaches mass of original liver o Restoration of liver mass achieved without regrowth of lobes that were resected at operation; growth occurs by enlargement of lobes that remain after operation (compensatory hyperplasia) o Almost all hepatocytes replicate during liver regeneration; takes several hours to enter cell cycle and get to S phase of DNA replication (normally quiescent); wave of hepatocyte replication synchronized and is followed by synchronous replication of nonparenchymal cells (Kupffer cells, endothelial cells, and stellate cells) o Hepatocyte proliferation triggered by combined actions of cytokines and polypeptide growth factors With one exception, strictly dependent on paracrine effects of growth factos and cytokines (HGF and IL-6) produced by hepatic nonparenchymal cells Major restriction points are G0/G1 transition and G1/S transition o Takes more than 70 genes to start replication, including proto-oncogenes (c-FOS and c-JUN, whose products dimerize to form transcription factor AP-1), c-MYC (encodes transcription factor that activates other genes), and other transcription factors (NF-κB, STAT-3, and C/EBP) o Quiescent hepatocytes become compentent to enter cell cycle through priming phase mostly mediated by cytokines (TNF and IL-6) and components of complement system Priming signals activate signal transduction pathways Under stimulation of HGF, TGFα, and HB-EGF, primed hepatocytes enter cell cycle and undergo DNA replication Norepinephrine, serotonin, insulin, thyroid hormone, and GH facilitate entry of hepatocytes into cell cycle o Individual hepatocytes replicate once or twice during regeneration then return to quiescence o Intrahepatic stem or progenitor cells do not play role in compensatory growth o Endothelial cells and other nonparenchymal cells may originate from bone marrow precursors Extracellular Matrix and Cell-Matrix Interactions ECM regulates growth, proliferation, movement, and differentiation of cells living in it ECM synthesis and degradation accompanies morphogenesis, regeneration, wound healing, chronic fibrotic processes, tumor invasion, and metastasis