- Sacramento - The California State University
advertisement

PHANTOM STUDIES OF MICRO-IMPULSE RADAR DETECTION OF CRANIAL
HEMATOMAS
A Thesis
Presented to the faculty of the Department of Electrical and Electronic Engineering
California State University, Sacramento
Submitted in partial satisfaction of
the requirements for the degree of
MASTER OF SCIENCE
in
Electrical and Electronic Engineering
by
Saul Sanchez
SUMMER
2013
PHANTOM STUDIES OF MICRO-IMPULSE RADAR DETECTION OF CRANIAL
HEMATOMAS
A Thesis
by
Saul Sanchez
Approved by:
__________________________________, Committee Chair
Warren D. Smith
__________________________________, Second Reader
Preetham B. Kumar
__________________________________, Third Reader
Russ Tatro
____________________________
Date
ii
Student: Saul Sanchez
I certify that this student has met the requirements for format contained in the University
format manual, and that this thesis is suitable for shelving in the Library and credit is to
be awarded for the thesis.
__________________________, Graduate Coordinator
Preetham B. Kumar, Ph.D.
Department of Electrical and Electronic Engineering
iii
___________________
Date
Abstract
of
PHANTOM STUDIES OF MICRO-IMPULSE RADAR DETECTION OF
INTRACRANIAL
HEMATOMAS
by
Saul Sanchez
Traumatic brain injury (TBI) is a serious health problem that can lead to permanent
disability or death. A TBI may cause two major types of intra-cranial hemorrhage:
subdural hematoma (SDH) and epidural hematoma (EDH). Subdural hematomas are the
most common. Acute SDH/EDHs are associated with a high mortality rate, thus
requiring immediate surgical treatment. Complications due to an SDH/EDH include
seizures, temporary or permanent numbness, dizziness, headaches, coma, and death. The
Glasgow Coma Scale (GCS) is the most commonly used method of diagnosis to
determine if a person needs to be hospitalized to test for the presence of an SDH/EDH.
Current technologies, computer tomography (CT) scans and magnetic resonance imaging
(MRI), to detect an SDH/EDH require the patient to be hospitalized.
Lawrence Livermore National Laboratory currently is developing a portable device
that uses micro-power impulse radar (MIR) to help in the rapid detection of SDH/EDHs.
The device, which is currently undergoing clinical trials, has successfully detected a large
EDH. This thesis describes a phantom study performed to determine the possibility of
iv
detecting an intracranial hematoma as small as 1 cc using the device. If a small
hematoma is diagnosed, the device would allow for constant monitoring for further
volume growth.
A bench top experiment used porcine brain tissue, blood, and the upper portion of a
human skull to simulate a human head. A latex pouch containing blood was used to
simulate an intracranial hematoma. The data obtained showed that the hematoma detector
was able to detect an SDH as small as 1 cc. The hematoma volume was incremented in
volume to observe the effects it had on the return signal. It was observed that as the
hematoma volume was increased, the detected return signal amplitude was altered in a
non-linear manner.
__________________________, Committee Chair
Warren D. Smith, Ph.D.
_______________________
Date
v
ACKNOWLEDGMENTS
I want to thank Dr. Warren Smith for his guidance, support, and for being such a
great professor and a magnificent mentor. I would like to thank all the people involved in
the hematoma detector project, especially Dr. John Chang, Amy Gryshuk, and Tony
Lazard. I would also like to thank professor Russ Tatro and Dr. Preetham Kumar for
providing valuable feedback and for being part of my thesis committee. I am enormously
grateful to my family for their unconditional love and support throughout the years.
Finally, I would like to thank my wife for all the support, love, and putting up with all the
engineering and programming nonsense (according to her).
vi
TABLE OF CONTENTS
Page
Acknowledgments ....................................................................................................... vi
List of Figures ............................................................................................................. ix
Chapter
1. INTRODUCTION …………… .............................................................................. 1
2. BACKGROUND .................................................................................................... 3
A. Medical Need ....................................................................................... 3
B. Ultra-Wideband Radar Technology ..................................................... 5
C. Medical Use of UWB Radar ................................................................ 6
D. Hematoma Detector .............................................................................. 8
3. METHODOLOGY ............................................................................................... 15
A. Materials ............................................................................................ 15
B. Hematoma Phantom ........................................................................... 17
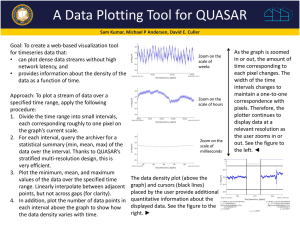
C. Hematoma Detector Computer Interface ........................................... 21
D. Procedure ............................................................................................ 22
4. RESULTS AND DISCUSSION .......................................................................... 24
A. Experimental Results .......................................................................... 24
B. Discussion .......................................................................................... 32
5. SUMMARY, CONCLUSIONS, AND RECOMMENDATIONS ...................... 34
vii
A. Summary ............................................................................................ 34
B. Conclusions ........................................................................................ 34
C. Recommendations .............................................................................. 35
Appendix A. MATLAB Code .................................................................................. 36
Appendix B. MATLAB Movie Code ........................................................................ 50
References .................................................................................................................. 52
viii
LIST OF FIGURES
Figure
1.
Page
Figure 1. Head computer tomography (CT) scan of a patient with an
epidural hematoma ............................................................................................ 4
2.
Figure 2. Electric field amplitude traveling along the z-axis ...........................12
3.
Figure 3. Results from previous hematoma phantom experiment ....................14
4.
Figure 4. Skull and antenna placement ............................................................18
5.
Figure 5. The investigator injecting blood into the latex pouch ......................19
6.
Figure 6. Experimental set-up showing the blood pouch positioned inside
the human skull .................................................................................................20
7.
Figure 7. Four average signals showing no significant change for brain
matter inside the skull with no latex pouch ......................................................25
8.
Figure 8. Return signals for the brain with and without the empty latex
pouch .................................................................................................................26
9.
Figure 9. Zoomed in portion of the affected signals from Figure 8 ..................27
10.
Figure 10. Average signals for the empty blood pouch, a 1-cc hematoma,
and a 2.5-cc hematoma phantom ......................................................................28
11.
Figure 11. Zoomed in portion of the affected signals from Figure 10 .............29
12.
Figure 12. Difference signals obtained by subtracting the signal for the
empty latex pouch from the signals for hematomas .........................................30
ix
13.
Figure 13. Compilation of return signals for incremented hematoma
volumes ............................................................................................................31
x
1
Chapter 1
INTRODUCTION
Traumatic brain injuries (TBIs) are a major cause of morbidity. According to the
Centers for Disease Control and Prevention, motor-vehicle accidents, assaults, firearms
use, falls, and sports are the most common causes of TBIs. Complications in TBIs can
lead to the development of an intracranial hemorrhage (hematoma), which can cause
intracranial pressure due to the collection of blood. If an intracranial hematoma is not
diagnosed and treated in a timely manner, it might cause seizures, memory loss, and even
death [1, 2, 3, 4, 5].
Visual inspection cannot be used to determine the severity of a TBI or occurrence
of an intracranial hematoma. The Glasgow Coma Scale (GCS) is a neurological scale
used in the assessment of TBI severity. Under current medical practices, anyone who has
suffered a major accident or has a GCS score of less than 13 needs to be hospitalized to
be observed for the development of intracranial hematoma [2, 6, 7]. However, the GCS
leaves room for interpretation, and factors such as cooperation from the person can alter
the diagnosis. Effective diagnosis of an intracranial hematoma requires the patient to be
hospitalized for head imaging using computer tomography (CT) or magnetic resonance
imaging (MRI) [2, 3, 4].
Lawrence Livermore National Laboratory currently is developing a micro-power
impulse radar (MIR) hematoma detector to help in the rapid detection of intracranial
hematomas. The detector has a potential advantage over current technologies because it is
2
portable and could provide valuable information to doctors or emergency personnel. It
could give a rapid diagnosis in situations where there is no access to a hospital, such as
the combat field or remote rural locations [8]. The device, which is undergoing clinical
trials, has successfully detected a large epidural hematoma (EDH).
The purpose of this work is to carry out a phantom study to determine the
hematoma detector’s ability to detect an intracranial hematoma and show how the
obtained return signal varies as the hematoma volume increases. Chapter 2 provides
background information on the medical need, as well as MIR technology applications in
medicine and how that technology led to the development of the hematoma detector.
Chapter 3 presents the methodology of the study, including material selection for the
creation of the intracranial hematoma phantom and the bench top experiment set-up used
to ensure repeatability. Chapter 4 gives the experimental results and describes how the
obtained data were used to determine the device’s ability to detect a hematoma phantom
as small as 1 cc. Chapter 5 summarizes the results, gives conclusions, and provides
recommendations for future work.
3
Chapter 2
BACKGROUND
A. Medical Need
In the United States, there are 1.7 million TBIs each year, of which 275,000 result
in hospitalization and 52,000 result in death [1]. Complications in TBIs can lead to the
development of an intracranial hematoma. Subdural hematomas (SDHs), the formation of
a blood pool between the dura mater and the brain, and epidural hematomas (EDHs), the
collection of blood between the inside of the skull and the outer covering of the brain, are
two major classifications of intracranial hematomas. In the United States, SDHs are the
most common type of intracranial lesion caused by TBIs [2]. Epidural hematomas usually
are observed in children and adolescents [6]. Figure 1 shows the CT scan of a patient’s
head with an EDH seen on the right side of the picture as a light gray region labeled as
“fresh and clotting blood.” Subdural/epidural hematomas are classified as acute if they
appear within hours after a TBI and as chronic if they slowly develop days after the TBI.
Acute intracranial hematomas can be caused by severe or minor head injury and have a
high mortality rate if not treated immediately [3, 4, 5]. Symptoms due to an SDH/EDH
include seizures, temporary or permanent numbness, dizziness, and headaches [5]. The
increased intracranial pressure due to the collection of blood between the dura mater and
the brain or the dura mater and the skull can result in death or coma if the pressure is not
relieved via surgical decompression [2].
4
Figure 1. Head computer tomography (CT) scan of a patient with an epidural hematoma.
The hematoma is seen on the right side of the picture as a light coloration labeled as
“fresh and clotting blood” [8].
Early detection of an intracranial hematoma has proven to reduce the risk of
permanent brain damage [1]; unfortunately, visual inspection for damage cannot be used
to determine the severity of a TBI or occurrence of an SDH/EDH. The GCS is the most
widely-used method of prognosis to determine if a person needs to be hospitalized for
observation and head imaging. However, it leaves room for interpretation, and factors
such as cooperation from the person can alter the diagnosis. The GCS might not be easy
5
to use in all occasions, such as an accident where a person has suffered eye inflammation,
preventing medical personnel from assessing accurately eye responsiveness. Other factors
such as a patient speech disorder can influence the validity of a verbal assessment.
Current head imaging technologies, CT scans or MRI, employed to detect an
SDH/EDH require the patient to be hospitalized. Such resources are costly. Not all TBI
patients develop an SDH/EDH. In such cases, performing a CT/MRI scan would be
unnecessary. The limited availability of CT scanners, MRI machines, and medical
personnel to operate them augments the delay in detecting intracranial hematomas,
increasing the risk of severe brain damage [1].
B. Ultra-Wideband Radar Technology
Radar technology uses radiated and reflected electromagnetic waves to determine
the position and velocity of objects. The basic process in a radar system is the
transmission and detection of an electromagnetic wave or pulse. An antenna, usually
determined by the radar application, emits electromagnetic pulses/waves along the
antenna’s aperture direction that bounce back as the pulses/waves encounter an object [9,
10].
The term ultra-wideband refers to an electromagnetic signal having a bandwidth
bigger than 25% of its central frequency or any signal having a bandwidth greater than
500 MHz [11]. Ultra-wideband radar is characterized as utilizing carrier-free pulses with
6
very short duration. In the case of the UWB non-sinusoidal carrier-free system, the
normalized bandwidth (η) can be determined by [12]
fH fL
, 0 1,
fH fL
(1)
where f H and f L correspond to the highest and lowest frequency, respectively. The
UWB signal center frequency is obtained using
f0
( fH fL )
.
2
(2)
C. Medical Use of UWB Radar
The first radar applications were for military target detection and navigational
surveillance, but as radar technology has flourished, radar applications have broadened.
Some of the most common applications include flight control systems, motion detectors,
police traffic radar, and weather radar [10]. The idea of using radar to monitor human
physiology was first considered during the 1970s, but the available electronics during that
era were not cost-effective for such applications [13]. Advances in solid-state electronics
during the last decade have made possible ultra-wideband radar in medical applications
[14]. Medical applications implementing UWB have been restricted by the Federal
Communications Commission (FCC) to have a spectrum range from 3.1 to 10.6 GHz
7
[15]. One of the major concerns behind implementing UWB radar to monitor human
physiology is the biological effects of the emitted electromagnetic radiation, but research
has shown that the energy absorption, in terms of specific absorption rate (SAR), was not
significant enough to cause any evident biological and behavioral damage in primates
[16]. The SAR is a measure of the amount of radio frequency energy absorbed by living
tissue and can be calculated using
Ei
2
SAR
2
,
(3)
where E i is the magnitude of the incident electric field to the tissue, ρ is the tissue
density, and σ is the tissue conductivity [17]. Because UWB signals are non-ionizing,
they can be used for chronic non-invasive monitoring without causing adverse effects in
humans. Ultra-wideband radar is being considered to monitor respiration movement to
prevent sudden infant death syndrome and for heart monitors, fetal monitors, and even
for the detection of cancerous tumors [18, 19, 20]. Current UWB radar applications have
proven to be successful, as in the case of the pneumothorax detector developed by
Lawrence Livermore National Laboratory (LLNL), which is used to diagnose whether a
person has a collapsed lung [21]. Research on biomedical applications of UWB radar will
continue to grow, and one day it might replace current technologies used today, such as
ultrasound fetal monitoring [19].
8
D. Hematoma Detector
Lawrence Livermore National Laboratory is developing a non-invasive hematoma
detector to help in the rapid detection of an EDH/SDH. It uses an MIR system to
determine the presence of a blood pool inside the head. The MIR emits very short
electromagnetic pulses that are able to penetrate a variety of materials. The MIR system
was developed using low-cost components, thus making it cost-effective in medical
applications [8]. Its main components are a transmitter with a pulse generator [22], a
receiver with a pulse detector, timing circuitry, a signal processor, and a horn antenna
[23]. The horn antenna is suitable for MIR applications, since it can operate over a wide
range of frequencies, has no resonant elements, has a low standing wave ratio (SWR), has
high directivity, and is simple to construct. The advantage of having a high directivity
antenna translates to having more radiated power along the main lobe. The hematoma
detector produces pulses with a center frequency of 2 GHz and 200-ps pulse width at a 2MHz pulse repetition rate [8, 11].
The average power density emitted by the device is about 1 µW/cm², which is far
less than the average power density emitted by cellphones, 30 – 10,000 µW/cm². The
radiated average power density of 1 µW/cm² falls well below the guidelines for safety
level exposures of humans to radio frequency electromagnetic fields. According to the
safety standards recommended by the Institute of Electrical and Electronics Engineers
(IEEE), the maximum permissible power density exposure for radiated electromagnetic
fields in the range of the HIR hematoma detector is 130 µW/cm² [24]. The IEEE safety
9
level exposure recommendations take into consideration an average exposure time of 6
min., which is more than the average time needed to perform an MIR detector reading.
The process of placing the MIR hematoma detector adjacent to a patient head and
obtaining a reading takes an average of 15 s [25].
The electromagnetic pulses generated by the MIR are able to penetrate human
tissue, as well as inorganic materials. Each time a pulse encounters an interface, a portion
of the radiated pulse is transmitted through the interface, and a portion is reflected back.
The transmission and reflection of the pulse depend on the dielectric properties of the
materials. Biological tissues exhibit intrinsic dielectric properties that vary with
frequency over the entire electromagnetic spectrum. The materials used in the experiment
are considered to have lossy dielectric properties. The biological tissues used in the
experiment include porcine brain, blood, and human skull. Each tissue has a different
dielectric constant ( r ) and conductivity (σ), both being frequency dependent. The
phenomenon is attributed to the relaxation of water molecules within the tissue [26, 27].
It is because of the difference in the dielectric properties of each tissue that the MIR can
be used to determine the presence of different tissues as the radiated pulse encounters
various boundaries with different dielectric properties. At the boundaries between two
adjacent media, the transmitted ( Et ) and reflected ( Er ) UWB signal electric field
amplitudes can be evaluated respectively using [14]
Et Ei
(4)
10
and
Er Ei ,
(5)
where Ei is the electric field amplitude of the incident wave, τ is the transmission
coefficient, and Γ is the reflection coefficient. The transmission and reflection
coefficients can be calculated respectively by
2 r1
(6)
r1 r 2
and
r1 r 2
r1 r 2
,
(7)
where r1 is the dielectric property of the first medium encountered by the incident UWB
signal, and r 2 is the dielectric property of the second medium. The difference in the
dielectric properties of each tissue is what creates a unique reflected or transmitted pulse.
As the electromagnetic pulse radiated from the MIR antenna penetrates the tissue,
its magnitude is attenuated exponentially. Techniques to simulate the propagation of
11
electromagnetic waves in biological tissue have been developed using the finite
difference time domain (FDTD) [28, 29]. The amount of attenuation the signal suffers as
it travels thru the medium depends on the dielectric properties of the material. Even
though the hematoma detector radiates electromagnetic pulses that can travel thru
inorganic material, the project focuses on the ability of the MIR to travel thru organic
material. According to Maxwell’s equation for electromagnetic wave propagation in a
lossy medium, the wave decays as it propagates according to the equation
Ex ( z ) Ex0e z Ex0e z ,
(8)
where Ex0 and Ex0 are constants, and the propagation constant (γ) is given by
j .
Figure 2 shows the electric field amplitude as it propagates in a lossy medium. The
electric field amplitude is reduced in amplitude as it travels along the z-axis. The
electromagnetic wave loses power as it propagates in a lossy medium due to poor
conduction.
(9)
12
Figure 2. Electric field amplitude traveling along the z-axis. The electric field amplitude
is plotted at t = 0 and t = Δ t. The arrows indicate instantaneous electric field amplitudes
[14].
The attenuation constant (α) and the phase constant (β) can be calculated,
respectively, using
2
0
1 1
2
2
(10)
13
and
0
,
2
(11)
where 0 is the permeability of free space, ε is the relative permittivity, ω is the angular
frequency, and σ is the conductivity of the tissue. Waves are functions of both space and
time; thus, the electromagnetic wave traveling along the z-axis as a function of time is
defined as
E( z, t ) E0 e z cos(t z )a x ,
(12)
where a x is the Cartesian coordinate vector component for the electric field intensity ( E )
in the x-axis. Equation (12) shows that, as the wave propagates along the z-axis ( a z ), its
amplitude is attenuated by the factor e z [30].
A previous bench-top experiment to test the concept of detecting an EDH/SDH
hematoma was done [8]. However, the device used in this experiment was still at an early
stage of development. Figure 3 shows several signals obtained using this early MIR to
detect hematoma phantoms of different thicknesses. Figure 3a shows the signal obtained
versus normalized time for the experimental set-up in which there is no hematoma
phantom. Figures 3b-3d show the signal obtained versus normalized time for the set-up
14
containing hematoma phantoms having thicknesses of 10 mm, 24 mm, and 33 mm,
respectively. The oval marking shows how the amplitude of a particular peak increased as
the hematoma size increased.
Figure 3. Results from previous hematoma phantom experiment. The oval marking shows
a time interval where the peak amplitude changed as the hematoma thickness increased
from 0 mm to 10 mm, 24 mm, and 33 mm. The figure was modified by increasing font
size and adding the x-axis and y-axis labels to include time and amplitude labels to the
axes [8].
15
Chapter 3
METHODOLOGY
A. Materials
In order to simulate blood hemorrhage in the brain and in turn simulate the
presence of an intracranial hematoma phantom, it was necessary to consider different
materials for the simulation of a human brain, skull, and blood. Brain-tissue like
materials, such as agarose gels, silicone, and a two-part epoxy resin, have been used in
the creation of phantoms simulating brain tissue due to texture and light absorption
similarities [31, 32]. However, those materials were not used in this phantom study
because they do not simulate the electromagnetic absorption properties of the brain
tissue. Kainz et al. experimentally determined a combination of various materials to
create a gel-like substance that closely simulated the brain’s dielectric properties in the
frequency range of 100 MHz to 1 GHz for the study of electromagnetic interference of
Global System for Mobile Communications (GSM) mobile phones with a implantable
deep brain stimulator. The dielectric properties of the phantom gel used to simulate brain
tissue were measured with the commercially available HP-85070M Dielectric Probe
Measurement System from Hewlett Packard [33]. Hartsgove et al. [34] provide a similar
gel-like substance method to simulate brain and muscle tissue for the study of
electromagnetic dosimetry. In both studies, the permittivity and conductivity properties of
the phantom tissue were documented to be closely similar to those reported by Gabriel et
al. for brain tissue at room temperature [26]. Even though both papers well document the
16
material ratios used in the creation of their respective gel-like phantom materials, the
need to test the resulting gel would require a dielectric probe measurement system that is
unavailable at the California State University, Sacramento.
Porcine brain tissue has been used in biomedical research [35] because of its
resemblance to human brain tissue in anatomy, growth, composition, and distribution of
white and gray matter. However, what makes porcine brain tissue perfect for this study is
that dielectric properties of porcine brain tissue have been already documented. The SAR
in porcine brain tissue was determined using radio frequencies ranging from 800 to 1900
MHz [36]. The investigators measured both relative permittivity ( r ) and equivalent
conductivity (σ) of the tissue. Results showed that the porcine brain dielectric properties
are similar to those of the human brain. It was also shown that the tissue’s dielectric
properties are affected by temperature, pressure, blood content, and physiological factors
in ways similar to those of human brain tissue. Similarities in the tissue response to
frequency are important, since the hematoma detector emits ultra-wide band pulses. The
electromagnetic pulse generated by the MIR interacts with the brain tissue and is
attenuated according to its dielectric property. Similarities in the dielectric properties and
physiological composition between the human brain and the porcine brain were the main
reason it was decided to use pig brain tissue instead of previously discussed materials.
In order to simulate human blood, sheep blood with heparin was used. The
heparin was used as an anticoagulant to prevent blood clotting during the experiment.
The similarities between sheep blood and human blood have been established in
17
biological experiments, such as those by Satzke et al. [37]. There was no need to simulate
human skull since the top portion of the human skull was used.
B. Hematoma Phantom
The equipment used in the experiment consisted of two mechanisms: a firmly
stabilized mechanism without any moving parts and the other with only one moving part
that consisted of the plunger in the syringe. Figure 4 shows the top portion of a human
skull held upside down by two clamps attached to two ring stands to provide stability.
The skull top was placed with the inside surface upward in a way to allow the brain
matter to be placed inside the cavity. The hematoma detector antenna was clamped
underneath the skull. The horn antenna’s aperture was placed in direct contact and normal
to the external surface of the skull. The skull-top contained a hole that needed to be cover
by a plastic wrap in order to stop brain matter leakage. It was also observed that the
inside surface of the skull had some grooves that might cause air pockets. Pouring
isotonic saline solution, observed in Figure 4, into the skull cavity and pressing the plastic
against the skull inner wall prevented air pockets in the grooves.
The antenna was placed against the outer surface of the skull at a location with the
fewest grooves on the inner skull surface. There are no moving parts to the mechanism
once the clamps were firmly tightened and the saline solution was removed.
18
Plastic wrap
Top portion of a
human skull
Hematoma detector
horn antenna
MIR hematoma
detector
0.9% isotonic saline
solution
Figure 4. Skull and antenna placement. The skull is held in place by two clamps for
stability. The MIR antenna is clamped beneath the upside down top portion of a human
skull with its aperture normal to the skull surface.
Figure 5 shows the investigator testing the apparatus. The figure shows the latex
pouch (on lab bench) used to simulate the hemorrhage caused by a TBI and the apparatus
(50-cc syringe and plastic tubing) used to inject desired volumes of blood into the pouch.
The syringe was held in place by a clamp attached to a ring stand to provide stability
while pushing down on the plunger. The latex material allowed the pouch to stretch as the
blood was injected.
19
Syringe
Plastic Tubing
Latex Pouch
Figure 5. The investigator injecting blood into the latex pouch. The injection apparatus
consists of a 50-cc syringe and plastic tubing and is connected to the latex pouch.
The position of the latex pouch containing 40 cc of blood can be observed in
Figure 6. The latex pouch, which was in contact with the inner wall of the skull, was
placed directly opposite to the antenna’s aperture surface, which was in direct contact
with the outer wall of the skull. In order to remove air bubbles from the tubing and the
latex pouch, the sheep’s blood was injected into the pouch, then extracted while holding
the syringe in a vertical position to allow all the air to collect at the top of the syringe
barrel. The air pocket stayed at the top of the barrel as long as the syringe maintained a
20
vertical position. The removal of any air pockets within the blood pouch was extremely
important, because they would have created other interfaces along the path of the radiated
electromagnetic pulse.
50 cc plastic syringe
Blood pouch containing 40
cc of blood
MIR hematoma detector
antenna
Figure 6. Experimental set-up showing the blood pouch positioned inside the human
skull.
21
The syringe was far enough from the antenna that it did not affect the signal
detected by the hematoma detector. Movement caused by the investigator pressing
against the plunger to push blood into the latex pouch did not affect the obtained signal.
C. Hematoma Detector Computer Interface
The hematoma detector created by LLNL personnel records the digitized values
of the return signal into a comma-separated values (CSV) file. The computer interface is
written in Laboratory Virtual Instrument Engineering Workbench (LabVIEW) 2009
software (National Instruments Corp., Austin, Texas). The number of return signal traces
recorded can be specified using the program interface. The computer interface
continuously displays the return signal. A specific trace can be recorded, or traces can be
recorded over an extended period. Each trace recorded for this phantom study contains
1000 data points. For each of the hematoma phantoms of various volumes, 200 traces
were recorded and saved into a CSV file. Matrix Laboratory (MATLAB) R2011a
(MathWorks, Inc., Natick, Massachusetts), which is a technical computing language, was
used to analyze the recorded CSV files. The MATLAB program reads each CSV file as a
matrix. In the case of this phantom study, each CSV file is converted into a matrix
containing 1000 columns and 200 rows, because each CSV file contains 200 traces
(rows) and 1000 sample points (columns).
22
D. Procedure
Once the apparatus was assembled and firmly stabilized in order to ensure the
only moving part is the plunger in the syringe, the pig tissue was placed inside the skull
cavity. The pig brain tissue, which was stored in a refrigerator, needed to reach room
temperature, 22º Celsius, in order to avoid changes in its dielectric properties as indicated
by Schmid et al. [36]. A baseline recording was made for the pig brain tissue inside the
skull with no blood pouch present. The continuous output display on the computer
interface was observed to confirm that a stable signal was obtained with no detected
change. In order to test for repeatability, four averaged traces were recorded.
The pig brain tissue was removed from the skull cavity in order to place the
empty blood pouch directly above the antenna’s aperture. The brain tissue then was
placed back on top of the empty blood pouch. A second baseline reading was taken with
the empty blood pouch between the pig brain tissue and the inner wall of the skull cavity
covered by the thin plastic wrap. It was verified that the computer displayed a stable
signal but, as expected, the addition of the blood pouch modified the return signal.
Once the hematoma detector was able to detect the presence of the empty blood
pouch, and the stability of the signal was established as confirmation that nothing on the
apparatus was changing, the blood was injected into the pouch via the injection
apparatus, shown in Figure 5. The volumes injected into the blood pouch from the 50-cc
syringe were: 1 cc, 2.5 cc, 5 cc, 8 cc, 11 cc, 17 cc, 27 cc and 40 cc. The hematoma
detector recorded the return signal for each of the indicated volumes.
23
The blood was drained back into the syringe and injected back into the pouch as
the hematoma detector continuously read the signal, and the computer recorded it.
Contrary to the previous settings where the simulated hematoma phantom had a specified
volume, the continuous flow of blood into the pouch simulating a hemorrhage would
provide valuable information on how the signal would react to the constant grow of a
hematoma. A continuous recording was made during this procedure.
24
Chapter 4
RESULTS AND DISCUSSION
A. Experimental Results
The traces displayed in the following sections are averages of 200 traces.
Appendix A contains the MATLAB program code used to analyze and display the
hematoma traces. As stated in the previous section, each time the hematoma volume was
increased, the hematoma detector recorded 200 traces that contained 1000 data points.
The average values were calculated using the MATLAB mean value array function. The
resulting matrix contained 1 trace of 1000 averaged data points. For future discussions,
the term average trace refers to such an average.
Figure 7 shows the four average traces obtained for the pig’s brain tissue inside
the skull with no hematoma. The brain tissue at room temperature, 22º Celsius, molded
perfectly to the inside cavity of the skull. There was very good repeatability in the signal,
because the positions of the antenna and the brain tissue were not changed. The ring
stands and clamps provided the needed stability of the skull and antenna. The little
change observed in the traces between data points 300 and 400 is due to the removal of
the pig brain tissue from the skull cavity. That difference was no longer observed once
the brain tissue was brain matter was not moved. The resulting averaged signal can be
observed in Figure 7 as a solid line trace. The average of these four average traces is used
in future comparisons during the discussion of the results.
25
Comparison of the brain tissue average signals
2
First brain tissue only signal
Second brain tissue only signal
Third brain tissue only signal
Fourth brain tissue only signal
Average brain tissue only signal
Normalized Amplitude
1.5
1
0.5
0
-0.5
0
100
200
300
400
500
600
Normalized Time
700
800
900
1000
Figure 7. Four average signals showing no significant change for brain matter inside the
skull with no latex pouch.
Figure 8 shows the resulting average trace for the latex pouch placed between the
inner wall of the human skull and the brain tissue together with the average signal
recorded for no latex pouch from Figure 7. As expected, the addition of the empty latex
pouch altered the return signal. The outbound pulse signal now encounters the latex
boundary going from skull to latex. As can be observed in Figure 8, the change in the
signal amplitude caused by the latex pouch is most prominent between data points 200
and 600.
26
Comparison between pouch and no pouch
2
Porcine brain with empty latex pouch
Porcine brain without latex pouch
Normalized Amplitude
1.5
1
0.5
0
-0.5
0
100
200
300
400
500
600
Normalized Time
700
800
900
1000
Figure 8. Return signals for the brain with and without the empty latex pouch.
In order to best observe the difference in the to signals, Figure 9 shows a zoomedin version of Figure 8 for the data range of 100 to 700 data points. The greatest peak
differences occur at data points 325 and 430. The peak at data point 325 increases in
amplitude. At data point 430, the valley is lowered in amplitude. Comparisons now are
made of signals for different blood volumes with the signal for the empty latex pouch
control (shown by dashed line in Figure 8).
27
Comparison between pouch and no pouch
Porcine brain with empty latex pouch
Porcine brain without latex pouch
Normalized Amplitude
0.6
0.4
0.2
0
-0.2
-0.4
200
250
300
350
400
450
Normalized Time
500
550
600
Figure 9. Zoomed in portion of the affected signals from Figure 8.
Figure 10 shows the average signals for the empty latex pouch, 1 cc of blood, and
2.5 cc of blood. The only thing changing in the experiment settings is the amount of
blood being injected into the latex pouch. The figure shows that the addition of the blood
caused the greatest changes between data points 250 and 650. It was observed that the
signal remained unchanging once the blood flow stopped.
28
Normalized Amplitude
Comparisons among the hematoma phantom volumes 0 cc, 1 cc, and 2.5 cc
2
0-cc Empty latex pouch
1.0-cc Hematoma phantom
2.5-cc Hematoma phantom
1.5
1
0.5
0
-0.5
0
100
200
300
400
500
600
Normalized Time
700
800
900
1000
Figure 10. Average signals for the empty blood pouch, a 1-cc hematoma, and a 2.5-cc
hematoma phantom.
Figure 11 is a zoomed-in version of Figure 10 to best observe the changes caused
by the increase in blood volumes in the latex pouch. From Figure 11, it can be observed
that a peak is created at data point 375. The other major change occurs at the peak located
at data point 510. The peak diminished in amplitude as the hematoma phantom increased
in volume. As the hematoma phantom volume was increase, the return signal display was
observed to have a small shift to the right as can be observed in Figure 11.
29
Comparisons among the hematoma phantom volumes 0 cc, 1 cc, and 2.5 cc
0-cc Empty latex pouch
1.0-cc Hematoma phantom
2.5-cc Hematoma phantom
0.6
Normalized Amplitude
0.4
0.2
0
-0.2
-0.4
200
250
300
350
400
450
Normalized Time
500
550
600
Figure 11. Zoomed in portion of the affected signals from Figure 10. A new peak is
created around data point 375.
Figure 12 highlights the difference in amplitude by subtracting the amplitudes of
the baseline signal, empty pouch signal, from the signals obtained for the 1 cc, 2.5 cc and
5 cc hematoma phantoms. The biggest difference in amplitude occurs near the 400 data
point. The amplitude difference signals also show that the biggest difference in amplitude
belongs to the biggest jump in hematoma volume, 0 cc to 5 cc, shown by the dashed line
in Figure 12.
30
Difference Signals
0.4
0 cc to 1.0 cc Difference
0 cc to 2.5 cc Difference
0 cc to 5.0 cc Difference
0.3
Normalized Amplitude
0.2
0.1
0
-0.1
-0.2
-0.3
-0.4
0
100
200
300
400
500
600
Normalized Time
700
800
900
1000
Figure 12. Difference signals obtained by subtracting the signal for the empty latex pouch
from the signals for hematomas.
.
A compilation of all the signals obtained for the incremented hematoma volume
size can be observed in Figure 13. It shows that the signal is affected not only in
amplitude but also in delay. The signal displays peaks that change size as the volume of
the hematoma phantom is incremented, with the most prominent change in the waveform
occurring in the amplitude at the 400 data point. It was observed that the signal started to
display a new peak at data point 390 as the hematoma phantom volume increased. For
31
each of the volumes displayed in Figure 13, once the determined volume was injected
into the pouch the signal recording was taken.
Obtained returned signals
3.5
3
2.5
40 cc
2
27 cc
1.5
17 cc
11 cc
8 cc
5 cc
2.5 cc
1 cc
1
0.5
0 cc
0
-0.5
0
100
200
300
400
500
600
Normalized Time
700
800
900
1000
Figure 13. Compilation of return signals for incremented hematoma volumes. The
waveforms are offset vertically for clarity.
In order to observe how the return signal changed due to continuous flow of blood
into the latex pouch, a MATLAB code in Appendix B was created. The continuous
display of the return signal showed that the signal still detected the blood interface at
point 300, and that the peak created at data point 390 increased in continuous manner.
32
Furthermore, the signal stays constant from data point 0 to 250, then start to change in
amplitude and shift throughout.
B. Discussion
In all the signals obtained it can be inferred that the emitted pulse encountering
the skull interface causes the first peak in the return signal. It is the peak with the highest
amplitude due to the immediate encounter of the signal with the bone matter. Most of the
change in the signal is located between data points 200 and 700 depending on the
presence of the latex pouch and the simulated hematoma phantoms.
The addition of the latex pouch between the skull and the brain tissue changed the
return signal amplitude between data points 200 and 600. The addition of the latex
interface creates a peak in the return signal around data point 325 as seen in Figure 9. The
addition of the latex pouch does not affect the signal after the second peak located at data
point 430. Once the latex pouch was placed, the only thing that changed in the
experiment was the addition of the blood using the injection apparatus.
The injection of 1 cc of blood into the pouch created a difference in the recorded
signal between the 250 to 700 data points. The most prominent change in the signal
amplitude was observed around data point 400. Figure 11 clearly show that the peak at
data point 375 broadens as well as increases in amplitude .As the hematoma phantom
increased in volume, the peak broadened as well. The differences in amplitudes from the
baseline signal for different hematoma volumes are best seen in Figure 12. It shows how
33
the amplitude change increases around data point 400 with respect to the volume of the
hematoma phantom. It was observed that increasing the blood volume not only increased
the signal peak amplitude but also shifted the peak to the right.
Appendix B shows the MATLAB code used to create a video of how the return
signal changes as the there is a continuous flow of blood into the latex pouch. The video
showed that the signal remained unchanged until the blood reached the latex pouch. The
signal started to change in amplitude around data point 300, and as the volume increased
the peak located at data point 325 decreased in amplitude at the same time a new peak
was created at data point 390. The video showed that there were other changes in the
return signal for later data points, but those changes might have been caused by how the
signal was affected by the volume of blood contained within the pouch. The latex pouch
changed in shape from a flat surface to an egg-like shape as the blood volume increased
beyond 30 cc. Such change in shape might have caused changes in the return signal.
34
Chapter 5
SUMMARY, CONCLUSIONS, AND RECOMMENDATIONS
A. Summary
Traumatic brain injury is a serious health problem that can lead to SDH/EDHs.
This thesis describes a study to determine if an MIR device developed by LLNL can
detect an intracranial hematoma as small as 1 cc. Using a hematoma phantom consisting
of the top portion of a human skull, porcine brain tissue, and a latex pouch containing
sheep blood, MIR recordings were made as the amount of blood in the latex pouch was
increased.
B. Conclusions
The results show that it is possible to use the MIR to detect an intracranial
hematoma as small as 1 cc. Being able to detect a hematoma as small as 1 cc shows that
the hematoma detector can be used to monitor small size hematomas that might develop
into potentially deadly hematomas as in the case of chronic subdural hematomas.
Increasing the hematoma volume causes increasing changes in the MIR traces.
The return signal traces showed that, as the hematoma volume was increased, the signal
started to create a new peak around the data points where the initial 1 cc hematoma was
first detected. The signal displayed other amplitude changes after the range where the 1
cc hematoma was detected, but the shape of the hematoma pouch might have created
35
such changes as it changed from planar shape to oval-like shape for higher blood
volumes.
C. Recommendations
More research needs to be done in the development of the hematoma detector.
The experimental set-up did not show the effects of pressure, as would be caused by a
hematoma inside an intact human skull. Research has shown that the dielectric properties
of material tend to change with pressure. Thus, it is recommended to test the pressure
effects on the return signal.
The brain tissue proved to be hard to control, as the brain matter was mushy.
Another major issue that arose using brain matter in our in vitro experiment was the rapid
deterioration of the porcine brain tissue and sheep blood. The use of a gel like substance
and a saline solution would have allowed for a better control over the materials. The gellike substance could have been molded to the cavity of the skull and allowed the blood
pouch to be placed under pressure.
As the volume of the hematoma was increased, the return signal changed beyond
the data points where the hematoma phantom was initially detected. Such changes might
have been caused by how the signal interacts with the blood. The results need to be
compared with the results from future hematoma MIR in vivo testing.
36
APPENDIX A
MATLAB Code
%Saul Sanchez
%CSUS Electrical Engineering Department
%Dr. Smith Warren
%Date: April 12, 2012
%Last Day Modified: April 27, 2013
%Purpose: Analysis and Comparison between the obtained signals in the
%hematoma phantom experiment
clc
close all
clear all
% the first part will read and output a matrix containing the data
% points obtained for the saline solution inside the skull
saline01=csvread('SS04012011saline01.csv',0,2);
saline02=csvread('SS04012011saline02.csv',0,2);
saline03=csvread('SS04012011saline03.csv',0,2);
%the program starts to read the matrix from row 0, column 2
%column 1 only contains index points
Maxrownumb=min(size(saline01));%the number of rows
Maxcolnumb=max(size(saline01));%the number of columns
maxElement=max(max(saline01));%the maximum element in the whole matrix
minElement=min(min(saline01));%the minimum element in the whole matrix
xAxis=0:Maxcolnumb-1;% the number of rows used to determine the size of
%x-axis
sm01=mean(saline01); %saline01 is a matrix, mean(saline01) treats the
%columns of mean(saline01) as vectors, returning a row vector of mean
%values
sm02=mean(saline02);
sm03=mean(saline03);
%the following takes all the values from all the 200 values and
37
%averages them using the mean formula and puts them into a final saline
%mean(fsm) containing the mean values into a matrix
fsm=[sm01; sm02; sm03];
mfsm=mean(fsm); %average return signal for the 3 saline readings
figure(101);
hold on;
title('Signal for the saline solution inside skull')
plot(xAxis, sm01, '-- blue', 'LineWidth',2);
plot(xAxis, sm02, '-- red', 'LineWidth',2);
plot(xAxis, sm03, '-- green', 'LineWidth',2);
plot(xAxis, mfsm, 'black', 'LineWidth',2);
legend('First signal recorded','Second signal recorded', 'Third signal
recorded');
ylabel('Normalized Amplitude');
xlabel(‘Normalized Time’);
grid on;
hold off;
figure(102);
title('Averaged signal for the saline solution inside the skull');
plot(xAxis, mfsm, 'LineWidth',2);
legend('Return signal for saline');
ylabel('Normalized Amplitude');
xlabel('Normalized Time');
grid on;
%%%%% THE FOLLOWING SECTION ANALYSES THE BRAIN INSIDE THE SKULL WITHOUT
%%%%% THE HEMATOMA PHANTOM
brain01=csvread('SS04012011brain01.csv',0,2);
brain02=csvread('SS04012011brain02.csv',0,2);
brain03=csvread('SS04012011brain03.csv',0,2);
brain04=csvread('SS04012011brain03.csv',0,2);
%the program starts to read the matrix from row 0, column 2
%column 1 only contains index points
mb01=mean(brain01);
mb02=mean(brain02);
mb03=mean(brain03);
mb04=mean(brain04);
fbm=[mb01; mb02; mb03; mb04];
mfbm=mean(fbm); %The average values for the brain inside the skull
38
figure(200)
hold on
title('Return signal for porcine brain tissue inside skull');
ylabel('Normalized Amplitude');
xlabel('Normalized Time');
plot(xAxis, mb03, '-- red','LineWidth',2);
plot(xAxis, mb04, '-. black','LineWidth',2);
legend('First porcine brain tissue only signal','Second porcine brain
tissue only signal');
axis([0 1000 -0.5 2]);
grid on
hold off
figure(201)
plot(xAxis, mfbm, 'LineWidth',2)
title('Returned signal for brain tissue inside skull');
ylabel('Normalized Amplitude');
xlabel(‘Normalized Time’);
legend('Averaged signal for the porcine brain inside the skull');
axis([0 1000 -0.5 2]);
grid on
figure(203)
hold on
title('Comparison of the brain tissue average signals');
ylabel('Normalized Amplitude');
xlabel('Normalized Time');
plot(xAxis, mb01, '-- red','LineWidth',2);
plot(xAxis, mb02, ': black','LineWidth',2);
plot(xAxis, mb03, '-- blue','LineWidth',2);
plot(xAxis, mb04, '-. blue','LineWidth',2);
plot(xAxis, mfbm, '- black','LineWidth',2);
legend('First brain tissue only signal','Second brain tissue only
signal','Third brain tissue only signal','Fourth brain tissue only
signal','Average brain tissue only signal');
axis([0 1000 -0.5 2]);
grid on
hold off
%NOTE: there is no difference between brain03 and brain04.
%it shows that the biggest difference is located along the 300 to 600
%points
%%%% comparing the saline solution, brain only and brain with latex
%pouch
%%%% THE FOLLOWING SECTION ANALYSES THE HEMATOMA PHANTOM SETTINGS
39
hematoma01=csvread('SS04012011brainblood01.csv',0,2);%
hematoma02=csvread('SS04012011brainblood02.csv',0,2);
hematoma03=csvread('SS04012011brainblood03.csv',0,2);
%hematoma04=csvread('SS04012011brainblood04.csv',0,2); The file was not
%found due to naming repetition during the experiment
%%%%%%%%Incrementing hematoma phantom volume from 0-cc to 40-cc
hematoma05=csvread('SS04012011brainblood05.csv',0,2);%control signal
%brain and empty pouch
hematoma06=csvread('SS04012011brainblood06.csv',0,2);%1cc phantom
hematoma07=csvread('SS04012011brainblood07.csv',0,2);%2.5cc phantom
hematoma08=csvread('SS04012011brainblood08.csv',0,2);%5cc phantom
hematoma09=csvread('SS04012011brainblood09.csv',0,2);%8cc phantom (400
traces instead of 200)
hematoma10=csvread('SS04012011brainblood10.csv',0,2);%11cc phantom
hematoma11=csvread('SS04012011brainblood11.csv',0,2);%17cc phantom
hematoma12=csvread('SS04012011brainblood12.csv',0,2);%27cc phantom
hematoma13=csvread('SS04012011brainblood13.csv',0,2);%40cc phantom
%%%%%%%Reducing hematoma phantom volume from 40-cc to 0-cc
%%%%%%% The following measurements were taken when extracting the blood
%from the latex pouch in order to simulate continuous bleeding in a
%increasing the hematoma
hematoma14=csvread('SS04012011brainblood14.csv',0,2);%25cc phantom
hematoma15=csvread('SS04012011brainblood15.csv',0,2);%20cc phantom
hematoma16=csvread('SS04012011brainblood16.csv',0,2);%15cc phantom
hematoma17=csvread('SS04012011brainblood17.csv',0,2);%10cc phantom
hematoma18=csvread('SS04012011brainblood18.csv',0,2);%5cc phantom
hematoma19=csvread('SS04012011brainblood19.csv',0,2);%1cc phantom
hematoma20=csvread('SS04012011brainblood20.csv',0,2);%0cc phantom
%the program starts to read the matix from row 0, column 2
%column 1 only contains index points
%brain hematoma mean----bhm
bhm01=mean(hematoma01);
bhm02=mean(hematoma02);
bhm03=mean(hematoma03);
%%%%%%NOTE:
%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%
%%%NOTE:
40
%%%FOR THE ANALYSIS AND COMAPARISON THE READINGS FOR
%%%SS04012011brainblood01.csv, SS04012011brainblood02.csv,
%%%SS04012011brainblood03.csv, SS04012011brainblood20.csv ARE NOT USED
%%%SINCE THOSE READINGS WERE OBTAINED UNDER A METHOD THAT WAS ABORTED
%%% AT 3-CC DUE TO REPEATIBILITY ISSUES. THERE IS NOT FILE FOR
SS04012011brainblood04.csv SINCE WE STARTED
%%%TO DO ALL THE READINGS AT SS04012011brainblood05.csv
%brain hematoma mean (bdm#) averages the 200 traces taken per setting
and
%provides a single row matrix with the mean of each column. The mean
% values for each setting will be used for comparison
bhm05=mean(hematoma05);
bhm06=mean(hematoma06);
bhm07=mean(hematoma07);
bhm08=mean(hematoma08);
bhm09=mean(hematoma09);
bhm10=mean(hematoma10);
bhm11=mean(hematoma11);
bhm12=mean(hematoma12);
bhm13=mean(hematoma13);
bhm14=mean(hematoma14);
bhm15=mean(hematoma15);
bhm16=mean(hematoma16);
bhm17=mean(hematoma17);
bhm18=mean(hematoma18);
bhm19=mean(hematoma19);
bhm20=mean(hematoma20);
%final brain hematoma mean matrix contains all the mean values for each
% of the hematoma phantom volumes
fbhm=[bhm05; bhm06; bhm07; bhm08; bhm09; bhm10; bhm11; bhm12; bhm13;
bhm14; bhm15; bhm16; bhm17; bhm18; bhm19; bhm20];
figure(301)
title('Obtained Signals all Hematoma Volumes');
ylabel('Normalized Amplitude');
xlabel(‘Normalized Time’);
hold on
plot(xAxis, bhm05, 'blue');
plot(xAxis, bhm06, 'red');
plot(xAxis, bhm07, 'green');
plot(xAxis, bhm08, 'yellow');
plot(xAxis, bhm09, 'black');
plot(xAxis, bhm10, 'blue');
plot(xAxis, bhm11, 'red');
plot(xAxis, bhm12, 'green');
41
plot(xAxis,
plot(xAxis,
plot(xAxis,
plot(xAxis,
plot(xAxis,
plot(xAxis,
plot(xAxis,
plot(xAxis,
bhm13,
bhm14,
bhm15,
bhm16,
bhm17,
bhm18,
bhm19,
bhm20,
'yellow');
'black');
'blue');
'red');
'green');
'yellow');
'black');
'black');
axis([0 1000 -0.5 2]);
grid on
hold off
figure(303)
title('Obtained signal for various increments in hematoma volume');
ylabel('Normalized Amplitude');
xlabel(‘Normalized Time’);
hold on
plot(xAxis, bhm05, 'blue','LineWidth',2);
plot(xAxis, bhm06, 'red','LineWidth',2);
plot(xAxis, bhm07, 'green','LineWidth',2);
plot(xAxis, bhm08, 'black','LineWidth',2);
plot(xAxis, bhm09, '-- blue','LineWidth',2);
plot(xAxis, bhm10, '-- red','LineWidth',2);
plot(xAxis, bhm11, '-- green','LineWidth',2);
plot(xAxis, bhm12, '-- black','LineWidth',2);
plot(xAxis, bhm13, '-. blue','LineWidth',2);
axis([0 1000 -0.5 2]);
grid on
hold off
figure(304)
title('Obtained signal for decrements in hematoma volume');
ylabel('Normalized Amplitude');
xlabel(‘Normalized Time’);
hold on
plot(xAxis, bhm14, 'black','LineWidth',2);
plot(xAxis, bhm15, 'blue','LineWidth',2);
plot(xAxis, bhm16, 'red','LineWidth',2);
plot(xAxis, bhm17, 'green','LineWidth',2);
plot(xAxis, bhm18, '-- black','LineWidth',2);
plot(xAxis, bhm19, '-- red','LineWidth',2);
plot(xAxis, bhm20, '-- blue','LineWidth',2);
axis([0 1000 -0.5 2]);
grid on
hold off
%%%%%THE FOLLOWING SECTION WILL COMPARE THE SKULL AND BRAIN ONLY
%SETTING
42
%%%%%WITH THE BRAIN AND LATEX POUCH WITHOUT BLOOD
figure(401)
title('Comparison between pouch and no pouch);
ylabel('Normalized Amplitude');
xlabel (‘Normalized Time’);
hold on
plot(xAxis, bhm05, '-- blue','LineWidth',2);
plot(xAxis, mfbm, 'red','LineWidth',2);
legend('Porcine brain with empty latex pouch','Porcine brain without
latex pouch');
axis([0 1000 -0.5 2]);
grid on
hold off
%%%the obtained graph shows that the baggy affects the signal amplitude
%%%from the 100 point to the 800 in the x-axis. The setup for the brain
%%%containing the latex pouch will be used for comparison for the
%%%increasing hematoma volume
figure(501)
title('Obtained signal: saline solution, porcine brain matter, porcine
brain matter with pouch');
ylabel('Normalized Amplitude');
xlabel('Normalized Time');
hold on
plot(xAxis, mfsm, '-- blue', 'LineWidth',2);
plot(xAxis, mfbm, ': black', 'LineWidth',2);
plot(xAxis, bhm05, 'red','LineWidth',2);
legend('Saline solution signal','Porcine brain matter', 'Porcine brain
matter with latex pouch');
axis([0 1000 -0.5 2]);
grid on
hold off
figure(502)
title(‘Comparisons among hematoma phantom volumes 0cc, 1cc, and
2.5cc');
ylabel('Normalized Amplitude');
xlabel(‘Normalized Time’);
hold on
plot(xAxis, bhm05, 'red', 'LineWidth',2);
plot(xAxis, bhm06, 'green', 'LineWidth',2);
plot(xAxis, bhm07, '-- blue', 'LineWidth',2);
legend('0-cc Empty blood pouch','1.0-cc Hematoma phantom', '2.5-cc
Hematoma phantom');
axis([0 1000 -0.5 2]);
grid on
hold off
43
%%%%comparing equal volume values after the blood has been injected
%%%% then extracted
figure(503)
title('Comparison between the brain hematoma between of equal values
0cc');
ylabel('Normalized Amplitude');
xlabel(‘Normalized Time’);
hold on
plot(xAxis, bhm05, '-- blue','LineWidth',2);
plot(xAxis, bhm20, '-- red','LineWidth',2);
legend('0-cc phantom before increasing size','0-cc phantom after
removing blood');
axis([0 1000 -0.5 2]);
grid on
hold off
figure(504)
title('Comparison between the brain hematoma of equal values 1cc');
ylabel('Normalized Amplitude');
xlabel(‘Normalized Time’);
hold on
plot(xAxis, bhm06, '-- blue','LineWidth',2);
plot(xAxis, bhm19, '-- red','LineWidth',2);
legend('1-cc phantom increasing size','1-cc phantom decreasing size');
axis([0 1000 -0.5 2]);
grid on
hold off
%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%
%NOTE: It was observed that the signals are not similar. This is due to
%the position of the latex pouch. The latex pouch changed position as
%the blood was drained. The change in position, relative to the MIR
%radar, was due to the brain tissue pushing to a different passion as
%the shape of the latex pouch changed for high volumes of blood.
%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%
%%%%Difference between the control 0cc signal and the returned hematoma
phantom signals
figure(506)
title('difference between the hematoma phantom volume 0cc, 1cc');
ylabel('Normalized Amplitude');
xlabel(‘Normalized Time’);
hold on
differencein0to1= bhm06 - bhm05;
plot(xAxis, differencein0to1 , 'red', 'LineWidth',2);
44
axis([0 1000 -0.4 0.4]);
grid on
hold off
%figure(507)
%title('Difference between the hematoma phantom volume 0cc, 2.5cc');
%ylabel('Normalized Amplitude');
%xlabel(‘Normalized Time’);
%hold on
differencein0to2= bhm07 - bhm05;
%plot(xAxis, differencein0to25 , 'red', 'LineWidth',2);
%axis([0 1000 -0.4 0.4]);
%grid on
%hold off
%figure(508)
%title('Difference between the hematoma phantom volume 0cc, 5cc');
%ylabel('Normalized Amplitude');
%xlabel(‘Normalized Time’);
%hold on
differencein0to5= bhm08 - bhm05;
%plot(xAxis, differencein0to5 , 'red', 'LineWidth',2);
%axis([0 1000 -0.4 0.4]);
%grid on
%hold off
%figure(509)
%title('Difference between the hematoma phantom volume 0cc, 8cc');
%ylabel('Normalized Amplitude');
%xlabel(‘Normalized Time’);
%hold on
differencein0to8= bhm09 - bhm05;
%plot(xAxis, differencein0to8 , 'red', 'LineWidth',2);
%axis([0 1000 -0.4 0.4]);
%grid on
%hold off
figure(510)
title('Difference between the hematoma phantom volume 0cc, 11cc');
ylabel('Normalized Amplitude');
xlabel(‘Normalized Time’);
hold on
differencein0to11= bhm10 - bhm05;
plot(xAxis, differencein0to11 , 'red', 'LineWidth',2);
axis([0 1000 -0.4 0.4]);
grid on
hold off
45
figure(511)
title('Difference between the hematoma phantom volume 0cc, 17cc');
ylabel('Normalized Amplitude');
xlabel(‘Normalized Time’);
hold on
differencein0to17= bhm11 - bhm05;
plot(xAxis, differencein0to17 , 'red', 'LineWidth',2);
axis([0 1000 -0.4 0.4]);
%figure(512)
%title('Difference between the hematoma phantom volume 0cc, 17cc');
%ylabel('Difference Absolute Amplitude');
%xlabel(‘Normalized Time’);
%hold on
%plot(xAxis, abs(differencein0to17) , 'red', 'LineWidth',2);
%axis([0 1000 -0.4 0.4]);
%grid on
%hold off
differencein0to27= bhm12 - bhm05;
differencein0to40= bhm13 - bhm05;
differencein25to0= bhm14 - bhm05;
differencein20to0= bhm15 - bhm05;
differencein15to0= bhm16 - bhm05;
differencein10to0= bhm17 - bhm05;
differencein5to0= bhm18 - bhm05;
differencein1to0= bhm19 - bhm05;
differencein0to0= bhm20 - bhm05;
differenceinbaggyNobaggy = bhm05-mfbm;
%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%
figure(513)
title('Difference Signals');
ylabel('Normalized Amplitude');
xlabel(‘Normalized Time’);
hold on
plot(xAxis, differencein0to1 , 'red', 'LineWidth',2);
plot(xAxis, differencein0to2 , 'blue', 'LineWidth',2);
plot(xAxis, differencein0to5 , 'black', 'LineWidth',2);
legend('0cc to 1.0cc Difference','0cc to 2.5cc Difference', '0cc to
5.0cc Difference');
46
axis([0 1000 -0.4 0.4]);
grid on
hold off
figure(514)
title('Signal differences');
ylabel('Normalized Amplitude');
xlabel(‘Normalized Time’);
hold on
plot(xAxis, differencein0to1 , 'red', 'LineWidth',2);
plot(xAxis, differencein0to2 , 'blue', 'LineWidth',2);
plot(xAxis, differencein0to5 , 'black', 'LineWidth',2);
legend('0cc to 1.0cc Difference','0cc to 2.5cc Difference', '0cc to
5.0cc Difference');
axis([0 1000 -0.4 0.4]);
grid on
hold off
figure(515)
title('Signal differences for incrementing phantom volume');
ylabel('Normalized Amplitude');
xlabel(‘Normalized Time’);
hold on
plot(xAxis, differencein0to1 , 'red', 'LineWidth',2);
plot(xAxis, differencein0to2 , 'blue', 'LineWidth',2);
plot(xAxis, differencein0to5 , 'black', 'LineWidth',2);
plot(xAxis, differencein0to8 , 'green','LineWidth',2);
plot(xAxis, differencein0to11 ,'-- red', 'LineWidth',2);
plot(xAxis, differencein0to17 , '-- blue', 'LineWidth',2);
plot(xAxis, differencein0to27 , '-- green', 'LineWidth',2);
plot(xAxis, differencein0to40 , '-- black', 'LineWidth',2);
legend('0cc to 1.0cc Difference','0cc to 2.5cc Difference', '0cc to
5.0cc Difference','0cc to 8.0cc Difference','0cc to 11.0cc Difference',
'0cc to 17.0cc Difference', '0cc to 27.0cc Difference','0cc to 40.0cc
Difference');
axis([0 1000 -0.6 0.6]);
grid on
hold off
figure(516)
title('Signal differences for decreasing phantom volume');
ylabel('Normalized Amplitude');
xlabel(‘Normalized Time’);
hold on
plot(xAxis, differencein25to0 , 'red', 'LineWidth',2);
plot(xAxis, differencein20to0 , 'black', 'LineWidth',2);
plot(xAxis, differencein15to0 , 'blue', 'LineWidth',2);
plot(xAxis, differencein10to0 , 'green','LineWidth',2);
plot(xAxis, differencein5to0 ,'-- blue', 'LineWidth',2);
47
plot(xAxis, differencein1to0 , '-- black', 'LineWidth',2);
%plot(xAxis, differencein0to0 , '-- yellow', 'LineWidth',2);
legend('25.0cc to 0cc Difference','20.0cc to 0cc Difference', '15.0cc
to 0cc Difference','10.0cc to 0cc Difference','5.0cc to 0cc
Difference', '1.0cc to 0cc Difference');
axis([0 1000 -0.6 0.6]);
grid on
hold off
figure(517)
title('Signal difference between porcine brain with and without latex
pouch');
ylabel('Normalized Amplitude');
hold on
plot(xAxis, differenceinbaggyNobaggy , 'black', 'LineWidth',2);
legend('difference between brain with and without latex pouch');
axis([0 1000 -0.4 0.4]);
grid on
hold off
%%%%%%%%% PLOTING THE DETECTED SIGNAL WITH OBTAINED FOR EACH BLOOD
VOLUME
%In order to best be able to look at all the signals in one graph the
%following compilation of the return signals was created:
figure(601)
title('Obtained return signals');
xlabel('Normalized Time');
set(gca,'ycolor', 'w')
hold on
plot(xAxis, bhm05, 'blue','LineWidth',2);
plot(xAxis, bhm06 + 0.15, 'green', 'LineWidth',2);
plot(xAxis, bhm07 + 0.30, 'red', 'LineWidth',2);
plot(xAxis, bhm08 + 0.50, 'black', 'LineWidth',2);
plot(xAxis, bhm09 + 0.65, '-- blue', 'LineWidth',2);
plot(xAxis, bhm10 + 0.80, '-- green', 'LineWidth',2);
plot(xAxis, bhm11 + 0.95, '-- red', 'LineWidth',2);
plot(xAxis, bhm12 + 1.15, '-- black', 'LineWidth',2);
plot(xAxis, bhm13 + 1.30, '-- blue', 'LineWidth',2);
grid on
hold off
figure(602)
title('Obtained signals for incrementing hematoma phantom volume');
%ylabel('Normalized Amplitude');
xlabel('Normalized Time');
set(gca,'ycolor', 'w')
hold on
plot(xAxis, bhm05, 'blue','LineWidth',2);
48
plot(xAxis, bhm06 + 0.15, 'green', 'LineWidth',2);
plot(xAxis, bhm07 + 0.375, 'red', 'LineWidth',2);
plot(xAxis, bhm08 + 0.75, 'black', 'LineWidth',2);
plot(xAxis, bhm09 + 1.2, '-- blue', 'LineWidth',2);
plot(xAxis, bhm10 + 1.65, '-- green', 'LineWidth',2);
plot(xAxis, bhm11 + 2.55, '-- red', 'LineWidth',2);
plot(xAxis, bhm12 + 4.05, '-- black', 'LineWidth',2);
plot(xAxis, bhm13 + 6, '-- blue', 'LineWidth',2);
%legend('Brain with empty blood pouch','Brain with 1-cc blood pouch');
%axis([0 1000 -0.5 2]);
grid on
hold off
figure(603)
title('Obtained signals for incrementing hematoma phantom volume');
%ylabel('Normalized Amplitude');
xlabel('Normalized Time');
set(gca,'ycolor', 'w')
hold on
plot(xAxis, bhm05, 'blue','LineWidth',2);
plot(xAxis, bhm06 + 0.25, 'green', 'LineWidth',2);
plot(xAxis, bhm07 + 0.50, 'red', 'LineWidth',2);
plot(xAxis, bhm08 + 0.75, 'black', 'LineWidth',2);
plot(xAxis, bhm09 + 1.0, '-- blue', 'LineWidth',2);
plot(xAxis, bhm10 + 1.25, '-- green', 'LineWidth',2);
plot(xAxis, bhm11 + 1.50, '-- red', 'LineWidth',2);
plot(xAxis, bhm12 + 1.75, '-- black', 'LineWidth',2);
plot(xAxis, bhm13 + 2.0, '-. blue', 'LineWidth',2);
grid on
hold off
figure(701)
title('Return signal for porcine brain with and without the latex
pouch');
set(gca,'ycolor', 'w')
hold on
plot(xAxis, bhm05, '-- blue','LineWidth',2);
plot(xAxis, mfbm + 0.29, 'red','LineWidth',2);
legend('Porcine brain with empty latex pouch','Porcine brain without
latex pouch');
axis([0 1000 -0.5 2]);
grid on
hold off
figure(702)
title('Obtained signal: saline solution, porcine brain matter, porcine
brain matter with pouch');
set(gca,'ycolor', 'w')
hold on
49
plot(xAxis, mfsm, 'black', 'LineWidth',2);
plot(xAxis, mfbm + 0.5, 'blue', 'LineWidth',2);
plot(xAxis, bhm05 + 1, 'red','LineWidth',2);
legend('Saline solution signal','Porcine brain matter', 'Porcine brain
matter with latex pouch');
grid on
hold off
50
APPENDIX B
MATLAB MOVIE Code
%Saul Sanchez
%CSUS Electrical Engineering Department
%Dr. Smith Warren
%Date: April 12, 2012
%Last Day Modified: April 27, 2013
%Purpose: To output the display of the MIR hematoma detector as a
continuous
% flow of blood is injected into the hematoma phantom pouch
clc
%close all
%clear all
hematoma20=csvread('SS04012011brainblood20.csv',0,2);%size 200x1000
hematoma21=csvread('SS04012011brainblood21.csv',0,2);%size 1000x1469
Maxrownumb20=min(size(hematoma20));%the number of rows
Maxcolnumb20=max(size(hematoma20));%the number of columns
%Maxrownumb21=min(size(hematoma21));%the number of rows
%Maxcolnumb21=max(size(hematoma21));%the number of columns
maxElement20=max(max(hematoma20));%the maximum element in the whole
matrix
minElement20=min(min(hematoma20));
%maxElement21=max(max(hematoma21));%the maximum element in the whole
matrix
%minElement21=min(min(hematoma21));
axis([0 1000 -0.5 2]);
%xAxis=linspace(0,Maxcolnumb-1,Maxcolnumb);
xAxis=0:1000-1;%we are using 1000 instead of specifying the column size
since the change in the max and min can change
RowZeros=zeros(1,1000);
%nframes=1469; %the number of frames
51
nframes= Maxcolnumb20;
%nframes= Maxcolnumb21;
lim=axis;
M=moviein(nframes);
for i=1:nframes%loop to form the movie frames
for h=1:1000
RowZeros(1,h)=hematoma21(i,h);
end
plot(xAxis,RowZeros,'LineWidth',2);
title('Continious Blood Injection');
ylabel('Normalized Amplitude');
xlabel('Normalized Time');
grid on;
axis(lim);
M(:,i)=getframe;
drawnow;%flushes the event queue and updates the figure window
end
movie(M,0,96); %12
%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%
%NOTE: The movie showed that the MIR hematoma detector was able to
detect the hematoma phantom, and that the peak around data point 390 is
the data point where the signal starts to show most change. The signal
also changes in amplitude and shifts after the hematoma is detected
which might be due to the effects caused by the blood volume.
% The initial signal for the continuous hematoma phantom is different
from the initial signal obtained for the predetermined phantom volumes
due to the placement of the latex pouch. The pouch moved after the
initial settings due to deflation effects of removing the blood. For
the continuous recording, the latex pouch was surrounded by the pig
brain matter and no longer in direct contact with the inner surface of
the skull wall.
52
REFERENCES
1. M. Faul, L. Xu, M.M. Wald, V.G. Coronado. “Traumatic brain injury in The United
States: emergency department visits, hospitalizations and deaths 2002-2006.”
Internet: http://www.cdc.gov/TraumaticBrainInjury, Mar. 10, 2010 [Mar. 20, 2011].
2. M.R. Bullock, D. Gordon, F. Servadei, R. Chesnut, R. Hartl, B.C. Walters, J. Ghajar,
D.W. Newell, J.E. Wilberger. “Guidelines for the surgical management of traumatic
brain injury.” Neurosurgery, vol. 58, pp. S2:1-S2:111, 2006.
3. G. Teasdale, S. Galbraith, L. Murray, P. Ward, D. Gentleman, M. McKean.
“Management of traumatic intracranial haematoma.” British Medical Journal, vol.
285, pp. 1695-1697, 1982.
4. E.Z. Kapsalaki, T.G. Machinis, J.S. Robinson III, B. Newman, A.A. Grigorian, K.N.
Fountas. “Spontaneous resolution of acute cranial subdural hematomas.” Clinical
Neurology and Neurosurgery, vol. 109, pp. 287-291, 2007.
5. D. Soloniuk, L.H. Pitts, M. Lovely, and H. Bartkowski. “Traumatic intracerebral
hematomas: timing of appearance and indications for operative removal.” The
Journal of Trauma, vol. 26, pp. 787-794, 1986.
6. J.L. Heller. “Extradural hemorrhage.” Internet:
http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0002385/, June 29, 2010 [May 5,
2011].
53
7. M.A. Vogelbaum, B.A. Kaufman, T.S. Park, A.L. Winthrop. “Management of
uncomplicated skull fractures in children: is hospital admission necessary?” Pediatric
Neurosurgery, vol. 29, pp. 96-101, 1998.
8. W. Haddad, J. Chang, T. Rosenbury, G. Dallum, P. Welsch, D. Scott, D. Duarte, V.
Acevedo-Bolton. “Microwave Hematoma Detector for the Rapid Assessment of Head
Injuries.” Lawrence Livermore National Laboratory, Technical Information
Department Digital Library. Internet: https://e-reports-ext.llnl.gov/pdf/237649.pdf,
Feb. 11, 2000 [Mar. 20, 2011].
9. R.M. Page. The Origin of RADAR. Garden City, NY: Anchor Books Doubleday,
1962.
10. N. Levanon. Radar Principles. New York: John Wiley, 1988.
11. J.D. Taylor. Introduction to Ultra-Wideband Radar Systems. Boca Raton, FL: CRC
Press, 1995.
12. M.G.M. Hussain. “Ultra-wideband impulse radar - an overview of the principles.”
Aerospace and Electronic Systems Magazine, IEEE, vol. 13, no. 9, pp. 9-14, 1998.
13. C.I. Franks, B.H. Brown, D.M. Johnson. ”Contactless respiration monitoring of
infants.” Medical and Biological Engineering and Computing, vol. 14, pp. 306-312,
1976.
14. C.N. Paulson, J.T. Chang, C.E. Romero, J. Watson, F.J. Pearce, N. Levin. “Ultrawideband radar methods and techniques of medical sensing and imaging,” presented
at SPIE International Symposium on Optics, Boston, MA, Oct. 23, 2005.
54
15. Code of Federal Regulations: Part 15 Subpart F Ultra-Wideband Operation, Federal
Communications Commission, May 2002.
16. C.J. Sherry, D.W. Blick, T.J. Walters, G.C. Brown, M.R. Murphy. “Lack of
behavioral effects in non-human primates after exposure to ultrawideband
electromagnetic radiation in the microwave frequency range.” Radiation Research,
vol. 143, pp. 93-97, 1995.
17. K. Caputa, M. Okoniewski, M.A. Stuchly. “An algorithm for computations of the
power deposition in human tissue.” IEEE Antennas and Propagation Magazine, vol.
41, pp. 102-107, Aug. 1999.
18. C.G. Bilich. “Bio-medical sensing using ultra wideband communications and radar
technology: a feasibility study,” in Pervasive Health Conference and Workshops,
2006, pp. 1-9.
19. E.M. Staderini. “UWB radars in medicine.” IEEE AESS Systems Magazine, vol. 15,
pp. 13-18, 2002.
20. X. Li, E.J. Bond, B.D. Van Veen, S.C. Hagness. “An overview of ultra-wideband
microwave imaging via space-time beamforming for early-stage breast-cancer
detection.” Antennas and Propagation Magazine, vol. 47, pp. 19-34, 2005.
21. J. Chang. “Fast Detection of a Punctured Lung.” Internet:
https://www.llnl.gov/str/Oct07/pdfs/10_07.1.pdf , Nov. 6, 2007 [Feb. 18, 2012].
22. T.E. McEwan. “Ultra-short pulse generator.” U.S. Patent 5 274 271, Dec. 28, 1993.
55
23. S. Azevedo, T.E. McEwan. “Micropower impulse radar,” in Potentials, IEEE, vol.
16, pp. 15-20, Apr. 1997.
24. IEEE Standard for Safety Levels with Respect to Human Exposure to Radio
Frequency Electromagnetic Fields, 3 kHz to 300 GHz. Internet:
http://ieeexplore.ieee.org/stamp.jsp?tp=&arnumber=STDPD95398&isnumber, Mar.
20, 2010 [Feb. 20, 2012].
25. J. Chang, C. Paulson, P. Welsh. “Development of micropower ultrawideband impulse
radar medical diagnostic systems for continuous monitoring applications and austere
environments,” Radar Conference (RADAR), 2012 IEEE, May 2012, pp. 699-704.
26. C. Gabriel, S. Gabriel, E. Corthout. “The dielectric properties of biological tissues: I.
Literature survey.” Physics in Medicine and Biology, vol. 41, pp. 2231-2249, 1996.
27. E. Pancera. “Medical applications of the ultra wideband technology,” Antennas and
Propagation Conference, 2010. Loughborough, United Kingdom, pp. 52-56. Nov.
2010.
28. M. O’Halloran, M. Glavin, E. Jones. “Comparison of a planar and finite difference
time domain technique to simulate the propagation of electromagnetic waves in
biological tissue,” in International Conference on microwaves, Radar and Wireless
Communications, 2006, pp.1037-1040.
56
29. S.C. Hagness, A. Taflove, J.E. Bridges. “Two-dimensional FDTD analysis of a
pulsed microwave confocal system for breast cancer detection: fixed-focus and
antenna-array sensors.” IEEE Transactions on Biomedical Engineering, vol. 45,
pp.1470-1479, 1998.
30. M.N.O. Sadiku. Elements of Electromagnetics. Oxford University Press, NY: New
York, 2001.
31. D.C. Ng, T. Tokuda, A. Yamamoto, M. Matsuo, M. Nunoshita, H. Tamura, Y.
Ishikawa, S Shiosaka, J. Ohta. “On-chip biofluorescence imaging inside a brain tissue
phantom using a CMOS image sensor for in vivo brain image verification.” Sensors
and Actuators, vol. 119, pp. 262-274, 2006.
32. M. Firbank, M. Oda, D.T. Delpy. “An improved design for a stable and reproducible
phantom material for use in near-infrared spectroscopy and imaging.” Physics in
Medicine and Biology, vol. 40, pp. 955-961, 1995.
33. W. Kainz, F. Alesch, D.D. Chan. “Electromagnetic interference of GSM mobile
phones with the implantable deep brain stimulator, ITREL-III.” Biomedical
Engineering Online, vol. 11, pp. 1-9, 2003.
34. G. Hartsgrove, A. Kraszewski, A. Surowiec. “Simulated biological materials for
electromagnetic radiation absorption studies.” Bioelectromagnetics, vol. 8, pp. 29-36,
1987.
57
35. N.M. Lind, A. Moustgaard, J. Jelsing, G. Vajita, P. Cumming, A.K. Hansen. “The use
of pigs in neuroscience: modeling brain disorders.” Neuroscience and Biobehavioral
Reviews, vol. 31, pp. 728-751, 2007.
36. G. Schmid, G. Neubauer, U.M. Illievich, F. Alesch. “Dielectric properties of porcine
brain tissue in the transition from life to death at frequencies from 800 to 1900 MHz,”
Bioelectromagnetics, vol. 24, pp. 413-422, 2003.
37. C. Satzke, A. Seduadua, R. Chandra, J.R. Carapetis, E.K. Mulholland, F.M. Russell.
“Comparison of citrated human blood, citrated sheep blood, and defibrinated sheep
blood Muller-Hilton agar preparations for antimicrobial susceptibility testing of
streptococcus pneumoniae isolates.” Journal of Clinical Microbiology, vol. 48, pp.
3770-3772, 2010.