Normal Flora of the GIT - PBL-J-2015

Normal Flora of the GIT; LO’s
1.
Demonstrate an understanding of the concept of normal flora in the GIT by being able to describe the nature and function of these microorganisms.
Stomach
- Acidic environment so limited flora, less than 10 organisms per mL, some GPC can survive.
Heliobacter pylori in mucosal layer, protected from acid.
Small intestine
- Close to sterile, high flow rate, the lower end of the small intestine, the ileum has rich natural flora, including many GNR.
Large intestine
- large intestine has slow Q (flow rate) it is a fermenter (12h) and 400+ species of fungi, protozoa, but mainly bacteria. These organisms secrete enzymes important in digestion. The large intestine is almost exclusively anaerobic, fermentation organic products. Faeces are
50%+ microbes. Bacterioides are anaerobic G-ve non-sporeing rods there are 10^11 per mL in the L.I.. Facultative anaerobes are also important in maintaining ht anaerobic environment.
2. For each of the following infections, describe typical features, diagnosis and treatment.
- Bacterial infections including food poisoning, gastroenteritis, invasive gastroenteritis, enteric fevers, viral infection, parasitic diseases.
Some enteric antigens.
“ 1) 0 antigen: This is the most external component of the lipopolysaccharide (LPS) of gram-negative bacteria.
The 0 antigen differs from organism to organism, depending on different sugars and different side-chain substitutions. Remember O for Outer (see Fig. 1-6, for more information on LPS).
2) K antigen: This is a capsule (Kapsule) that covers the 0 antigen.
3) H antigen: This antigenic determinant makes up the subunits of the bacterial flagella, so only bacteria that are motile will possess this antigen. Shigella does not have an H antigen. Salmonella has H antigens that change periodically, protecting it from our antibodies. “
Food Poisoning
Staph aureus
Toxins; enterotoxins
(superantigens that stimulate mast cells causing vomiting and nausea.)
Lipid A
Bacillius cereus
Toxin A- emetic
(induces vomiting 1-6 hrs)
Toxin B – Diarrhoeal
(8-16 hrs)
C. perfringes
Features
GPC in grape like clusters
Coagulase +ve,
Catalase positive,
Complete haemolysis B,
Salt tolerant, protein A, Blactamase, hyaluronidase
(destroys connective tissue)
B-haemolysis,
Source is cereals, spices, rice, potatoes, soups and custard.
Exotoxins can be in food before consumption.
Endospore production.
Has no capsule but is motile
Large, rectangular GPR. Can produce spores.
Diagnosis
Toxin mediated food poisoning,
- early onset vomiting and nausea followed by diarrhoea.
Nausea, cramps, vomiting and/or diarrhoea.
Gram stain, anaerobic culture.
Enterotoxin causes diarrhoea.
Treatment
Resistant to Blactam antibiotics,
However, with food poisoning due to the toxin there is no treatment.
(symptomatic)
Rapid antibiotic treatment
Ubiquitous in soil and
GIT
C.botulinum
Botulin toxin on foods and ingestion of the toxin causes
paralysis.
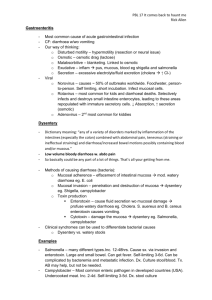
Gastroenteritis
E.Coli
Some non pathogenic strains aid digestion and synthesis vitimin
K
V. Cholera
Produces a heat sensitive enterotoxin.
Anaerobic GPR
Forms spores
Rare, however, the toxin can be present in un-treated honey, and infants are susceptible.
50% rate of death in untreated patients.
Features
GNR, varying strains and pathogenicity.
Most common GNR of the GIT
Microscopy reveals GPR in the absence of inflammatory cells due to cell lysis.
Paralysis,
Nausea vomiting
Fatigue
Dizziness
Double vision.
No fever associated
Diagnosis
Bloody or non- bloody diarrhoea, required.
Penicillin and clindamycin.
Treatment;
Botulism Immune
Globulin
Intravenous-
Human (BIG-IV)
Antitoxin and also may require hyperbaric oxygen, and intubation in infants.
Treatment
Usually self limiting
C. difficile
Curved GNR with a single polar flagellum.
Associated with faeces infected waters and monsoon seasons.
Anaerobic GP spore forming.
Associated with hospitals and nursing homes
Cholera toxin causes abrupt onset of watery diarrhoea.
An A-B toxin, A enters epithelial cell and activates cAMP, secreting Na Cl, so water follow.
Toxin A; diarrhoea
Toxin B; cytotoxin to colonic epithelial cells.
Immunoassay test
ELISA for toxin
Hydration therapy, risk of up to 1L of fluid loss per hour.
Onset of C.difficle infection often related to use of antibiotics.
Terminate use of causative antibiotic and can try oral vancomycin or metronidazole.
Invasive
Gastroenteritis
Features
Campylobacter jejuni Aerobic or mocroaerophilic spirillia. Cytotoxin and invasive proteins.
Shigella
Shigellosis = dysentry
EHEC
Enterhaemorrhagic
E.coli
GNR, facultative anaerobe.
Lipid A endotoxin.
Highly infectious, outbreaks in crowded conditions
Attachs mucosa of colon (Large intestine)
GNR, animal faeces contamination.
Expresses A-B shiga
Diagnosis
Bloody diarrohea, fever, abdominal cramps.
Bloody stools, cramping, fever, headache, watery stools associated with pus and blood.
Very Painful
Bloody Diarrhoea, fever.
Complications include renal failure, CNS symptoms in children under 5.
Treatment
Complication is HUS
(Hemolytic uremic syndrome) with anemia, and renal failure.
Patients with a
toxin. Acute enterocolitis with fever, diarrhoea and abdominal pain
Watery diarrhoea positive blood culture should be treated with antibiotics.
Yersinia Enterocolitica Rare, GNR
Enteric Fevers
Typhoid
Salmonella typhi
Invades through the
Peyer’s patches
Features
Enteric fever. Invades to the regional lymphnodes after invaiding intestinal wall.
A facultative intracellular parasite.
Diagnosis
Salmonellosis starts
1-3 weeks after exposure. Fever, headaches and abdominal pain.
Enlargement of spleen and diarrhoea.
Culture blood urine or stool.
Treatment
Ciprofloxacin or caftriaxone are considered appropriate therapy.
Paratyphoid
V.parahaemolyticus Marine organism that causes gastroenteritis after ingestion of uncooked seafood.
Viral infections
Rotavirus
Norovirus
Also refereed to as
Norwalk or small round virus.
Parasites
Entamoeba histolytica
Giardia intestinalis
Features
Diarrhoea associated with young children.
Day care centers.
Can be symptomatic or asymptomatic however both shed virus.
Features
Cryptosporidium parvum
No documented toxin
Environmentally stable cyst and trophozoite stage. Tends to infect parents of infected children, from swimming pools, water supply.
Enveloped
Oocysts
10 oocysts to initiate infection.
Affects immunocompromised patients severely.
Cryptosporidium parvum.
Symptoms NON aids
Voluminous water diarrhoea
Cramps
Fatigue, anorexia
Nausea, vomiting
Fever,chills, and sweats
Diagnosis
Projectile vomiting and fever >39*C v. infectious, nursing homes and restarants and hotels.
Violent and perfuse vomiting and duarrhoea at 15-24 hours after exposure.
Diagnosis
Diarrhoea, gas flatulence, greasy stools that float (fat malabsorption).
Stomach cramps, nausea.
Autoinfection occurs due to the 20% of
Treatment
5-8 days of hydratrion therapy.
Vaccine now available
Hydration therapy. 2-
3 days single unit membranes.
Malabsortion in the small bowel and villus damage. (bacterial overgrowth.)
Treatment
Infection onset 1-2 weeks after contact and symptoms 2-6 weeks. Antibiotics and also hydration therapy.
Routine disinfectants are not effective for cleaning, chlorination is not effective,
Symptoms AIDS
Chronic Diarrhoea, with insidious onset, sever protracted diarrhoea, watery motions 1-25 L per day.
Profound weight loss
Electrolyte disturbances.
Duration 2-14 days
Mean max no. stools/day is 19