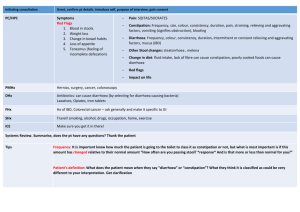
social management of chronic disease + gastroenteritis
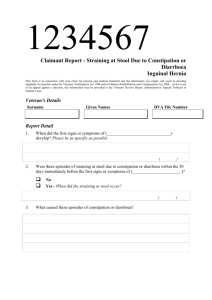
advertisement
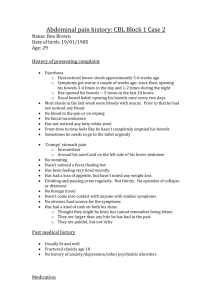
PBL 17 It comes back to haunt me Rick Allen Gastroenteritis - - Most common cause of acute gastrointestinal infection CF: diarrhoea w/wo vomiting Our way of thinking: o Disturbed motility – hypermotility (resection or neural issue) o Osmotic – osmotic drag (lactose) o Malabsorbitive – blanketing. Linked to osmotic o Exudative – inflam pus, mucous, blood eg shigella and salmonella o Secretion – excessive electrolyte/fluid excretion (cholera ↑ Cl-) Viral o Norovirus – causes ~ 50% of outbreaks worldwide. Food/water, personto-person. Self limiting, short incubation. Infect mucosal cells. o Rotavirus – most common for kids and diarrhoeal deaths. Selectively infects and destroys small intestine enterocytes, leading to these areas repopulated with immature secretory cells. ↓ Absorption, ↑ secretion (osmotic) o Adenovirus – 2nd most common for kiddies Dysentery - - - Dictionary meaning: “any of a variety of disorders marked by inflammation of the intestines (especially the colon) combined with abdominal pain, tenesmus (straining or ineffectual straining) and diarrhoea/increased bowel motions possibly containing blood and/or mucous.” Low volume bloody diarrhoea w. abdo pain So basically could be any part of a lot of things. That’s all your getting from me. Methods of causing diarrhoea (bacteria): o Mucosal adherence – effacement of intestinal mucosa mod. watery diarrhoea eg. E. coli o Mucosal invasion – penetration and destruction of mucosa dysentery eg. Shigella, campylobacter o Toxin production Enterotoxin – cause fluid secretion wo mucosal damage profuse watery diarrhoea eg. Cholera. S. auereus and B. cereus enterotoxin causes vomiting. Cytotoxin – damage the mucosa dysentery eg. Salmonella, campylobacter Clinical syndromes can be used to differentiate bacterial causes o Dysentery vs. watery stools Examples - - Salmonella – many different types.Inc. 12-48hrs. Cause sx. via invasion and enterotoxin. Large and small bowel. Can get fever. Self-limiting 3-6d. Can be complicated by bacteremia and metastatic infection. Dx. Culture stool/blood. Tx. AB may help, but not be needed. Campylobacter – Most common enteric pathogen in developed countries (USA). Undercooked meat. Inc. 2-4d. Self-limiting 3-5d. Dx. stool culture PBL 17 It comes back to haunt me Rick Allen - - Shigella – enterocyte invasion macrophage invasion inflam. Inc. 24-48 hrs. DYSENTRY, fever. Self limiting 7-10d. AB. Humans only known reservoir. E.coli – some nasty varients out there Cholera – raw fish/shellfish. “explosive diarrhoea”. Activates CFTR channels Cl secretion HCO3, H2O and Na into lumen S.aureus – enterotoxin Clostridium difficile – inc. 2d to 1 mth after AB use!!! Psuedomembranous colitis (psuedomembrane: neutrophil, dead epithelial cells and inflam. debris) RF. 3rd gen cephlasporins. Whipple disease – bacteria ingested by macrophages which accumulate in lamina propria + mesenteric lymph nodes lymphatic obstruction malabsorptive diarrhoea. Other - Giardia lamblia, cryptosporidium (basically like giardia), entamoeba histolytica, all types of worms (ascaris [nematode - round worm], cestodes [tapeworms], schistosomiasis [trematode - blood fluke], pinworms, hookworms) Prevention - HYGIENE BITCHES!!!! Stay clear of suspect food, water and people Stay clear of day care facilities, institutions or homes for the mentally ill Treatment - Rehydration – either orally or via IV as appropriate Ix. – blood/stool culture, stool toxins (difficile), electrolytes, urea. AB as deemed suitable. May not always be necessary. Determine the source Notifiable disease? Watch for pt. complications (septicaemia, renal failure, perforation) AVOID anti-motility drugs. PBL 17 It comes back to haunt me Rick Allen Management of chronic disease - - - - Chronic Disease o Features: persistent, complex causality, multiple RF, insidious onset (not always), not immediately life threatening (but complications may be) o Dimensions: Disease = clinical. Anatomical/physiological manifestations Illness = social. Impact/response of interactions w family, friends, co-workers, HCP, community. = Personal. Psychological, se;f perception and the perception of others o Pervasive uncertainty, no cure and ‘shared’ knowledge & expertise w Doc Dealing with it o Self management – gives a sense of control, confidence and responsibility to the pt., keeps them involved in the decision making process, gives them ownership. Increases efficacy and adherence. o Communication/partnerships with HCP o Focus beyond the condition – look at health promotion and lifestyle. Peoples capacity to manage chronic illness involves: o Individual factors: willpower, age, education, finance, attitude, beliefs… o Doc/HCP: approach o Family and friends: level of influence and support o Community organisations: self-help, peer support, role models o Work colleagues: support and acceptance o Community: support services, transport, attitude o Media/policy: information, laws, access to services, discrimination Docs role o Collaboratively defined probs: Doc and pt view. o Goal setting and planning: realistic considering pt. current position o Organise or assist with support services or education/training for effective self management o Active follow-up: specified intervals, monitor, reinforce progress.