Scope of Primary Care Dermatology and Indications for Referral
advertisement
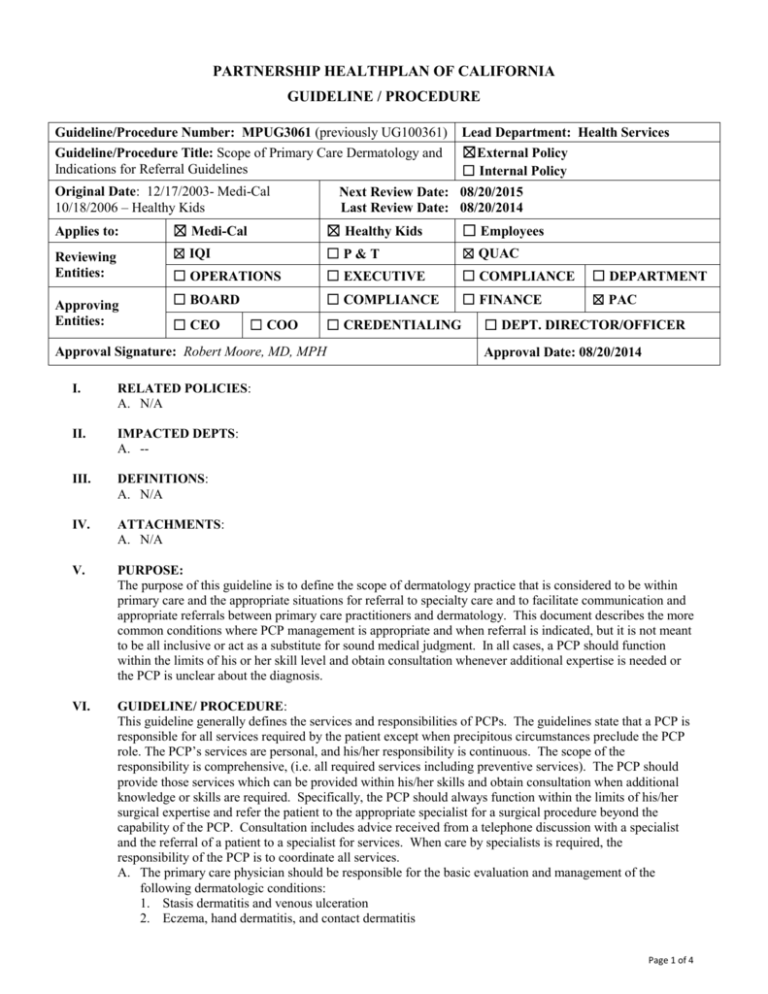
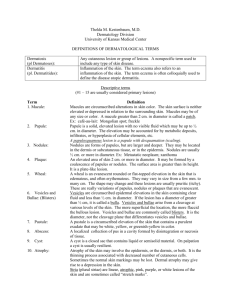
PARTNERSHIP HEALTHPLAN OF CALIFORNIA GUIDELINE / PROCEDURE Guideline/Procedure Number: MPUG3061 (previously UG100361) Guideline/Procedure Title: Scope of Primary Care Dermatology and Indications for Referral Guidelines Original Date: 12/17/2003- Medi-Cal 10/18/2006 – Healthy Kids Lead Department: Health Services ☒External Policy ☐ Internal Policy Next Review Date: 08/20/2015 Last Review Date: 08/20/2014 Applies to: ☒ Medi-Cal ☒ Healthy Kids ☐ Employees Reviewing Entities: ☒ IQI ☐P&T ☒ QUAC ☐ OPERATIONS ☐ EXECUTIVE ☐ COMPLIANCE ☐ DEPARTMENT ☐ BOARD ☐ COMPLIANCE ☐ FINANCE ☒ PAC Approving Entities: ☐ CEO ☐ COO ☐ CREDENTIALING Approval Signature: Robert Moore, MD, MPH ☐ DEPT. DIRECTOR/OFFICER Approval Date: 08/20/2014 I. RELATED POLICIES: A. N/A II. IMPACTED DEPTS: A. -- III. DEFINITIONS: A. N/A IV. ATTACHMENTS: A. N/A V. PURPOSE: The purpose of this guideline is to define the scope of dermatology practice that is considered to be within primary care and the appropriate situations for referral to specialty care and to facilitate communication and appropriate referrals between primary care practitioners and dermatology. This document describes the more common conditions where PCP management is appropriate and when referral is indicated, but it is not meant to be all inclusive or act as a substitute for sound medical judgment. In all cases, a PCP should function within the limits of his or her skill level and obtain consultation whenever additional expertise is needed or the PCP is unclear about the diagnosis. VI. GUIDELINE/ PROCEDURE: This guideline generally defines the services and responsibilities of PCPs. The guidelines state that a PCP is responsible for all services required by the patient except when precipitous circumstances preclude the PCP role. The PCP’s services are personal, and his/her responsibility is continuous. The scope of the responsibility is comprehensive, (i.e. all required services including preventive services). The PCP should provide those services which can be provided within his/her skills and obtain consultation when additional knowledge or skills are required. Specifically, the PCP should always function within the limits of his/her surgical expertise and refer the patient to the appropriate specialist for a surgical procedure beyond the capability of the PCP. Consultation includes advice received from a telephone discussion with a specialist and the referral of a patient to a specialist for services. When care by specialists is required, the responsibility of the PCP is to coordinate all services. A. The primary care physician should be responsible for the basic evaluation and management of the following dermatologic conditions: 1. Stasis dermatitis and venous ulceration 2. Eczema, hand dermatitis, and contact dermatitis Page 1 of 4 Guideline/Procedure Number: MPUG3061 (previously Lead Department: Health Services UG100361) Guideline/Procedure Title: Scope of Primary Care Dermatology ☒ External Policy and Indications for Referral Guidelines ☐ Internal Policy Original Date: 12/17/2003- Medi-Cal Next Review Date: 08/20/2015 10/18/2006 – Healthy Kids Last Review Date: 08/20/2014 Applies to: ☒ Medi-Cal ☒ Healthy Kids ☐ Employees 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. 20. 21. Atopic dermatitis Acute and chronic urticaria Acne, rosacea and related disorders. Psoriasis, seborrheic dermatitis and lichen planus Bacterial infections of the skin Sexually transmitted bacterial infections including gonorrhea, nongonococcal urethritis, and syphilis Sexually transmitted viral infections including genital warts, Molluscum contagiosum and genital herpes simplex Warts, herpes simplex and other viral infections of the skin Superficial fungal infections including dermatophyte fungal infections and candidiasis Exanthem and drug eruptions Infestations and bites including scabies, pediculosis and insect bites Diagnosis of bullous disorders Dermatologic manifestations of connective tissue disease Diagnosis of hypersensitivity reactions Diagnosis of benign skin tumors and surgical treatment localized to non-critical areas Diagnosis and treatment of premalignant and malignant nonmelanoma skin tumors and surgical treatment localized to non-critical areas Early recognition, biopsy, or referral of pigmented lesions suspicious for malignant melanoma Common hair and nail diseases Pediatric Dermatology – identification and referral as appropriate for common pediatric conditions including congenital skin and vascular lesions and refractory atopic dermatitis. B. A referral for dermatology conditions is considered appropriate in the following situations: 1. Acne a. No response in mild to moderate acne with the topical therapy. b. For mild to moderate acne without scarring the PCP should use at least three modalities over a three to six month period before considering referral. c. Active scarring d. Consideration of intralesional corticosteroids or procedures for scars e. Primary care physician is unfamiliar or uncomfortable with isotretinoin use. 2. Atopic Dermatitis a. Severe or persistent dermatitis or eczema b. Before starting any immunosuppressive therapy c. Erythroderma or extensive exfoliation d. Greater than a single use of systemic corticosteroids e. Identification of triggers and allergens f. Impaired quality of life g. Severe complications, e.g., infectious, ocular, or psychosocial 3. Actinic Keratoses a. When size or location of lesion requiring excision is beyond the capability of the PCP b. When widespread and or poorly controlled disease is present c. For extensive treatment of persistent actinic keratosis d. Immunocompromised patients: such as any transplant patients and pts with CLL e. When metastasis is suspected f. When standard treatments or surgery has failed 4. Basal Cell Carcinoma and Squamous Cell Carcinoma a. Lesions located on ANY ONE of the following - Nasolabial fold , All nasal lesions, Perioral region, Periauricular region, and Periocular region. Page 2 of 4 Guideline/Procedure Number: MPUG3061 (previously Lead Department: Health Services UG100361) Guideline/Procedure Title: Scope of Primary Care Dermatology ☒ External Policy and Indications for Referral Guidelines ☐ Internal Policy Original Date: 12/17/2003- Medi-Cal Next Review Date: 08/20/2015 10/18/2006 – Healthy Kids Last Review Date: 08/20/2014 Applies to: ☒ Medi-Cal ☒ Healthy Kids ☐ Employees 5. 6. 7. 8. 9. b. Difficult to excise scalp, forehead, hand, foot and genital lesions c. Lesions >2 cm d. More aggressive variants of basal cell such as morphea-like, sclerosing types, infiltrative, poorly differentiated, perineural invasion or baso-squamous types e. Lesions arising from scars or radiated skin f. Tumors with indistinct clinical margins g. Immunosuppressed patient h. Recurrences Dermatophytosis a. Diagnosis is unclear b. Unsatisfactory response to systemic treatment Malignant Melanoma and Pigmented Skin Lesions – to a dermatologist as appropriate a. Routine surveillance of high-risk patient if any one of the following applies 1) PCP not skilled or comfortable screening high-risk patient 2) Photographic mapping or microscopy is needed. 3) Patient has a personal history of melanoma and has multiple pigmented lesions b. Evaluation of suspicious lesions c. Biopsy or removal of lesions located in body areas felt to be beyond the PCP’s skill level to remove with good surgical and cosmetic results d. Wider excision needed e. Regional lymph node dissection f. Metastatic disease amenable to excision g. Consideration of chemotherapy or immunotherapy h. Radiation treatment of metastatic disease Psoriasis a. Chronic plaque psoriasis when all of the following are present: 1) Unsatisfactory response to topical treatment 2) Consideration of systemic treatments or phototherapy, e.g., UVB or PUVA b. Generalized pustular or erythrodermic psoriasis c. Psoriatic arthritis Skin ulcers, diabetic, ischemic, pressure or venous – Referral to dermatologist or vascular surgeon, or podiatrist as appropriate a. Debridement of calluses or ingrown toenails b. Periodic evaluation according to risk profile if the PCP is unable to monitor 1) No neuropathy: annual evaluation 2) Neuropathy present: semiannual evaluation 3) Neuropathy, either peripheral vascular disease or deformity present: quarterly evaluation 4) Previous ulcer or amputation: monthly to quarterly evaluation 5) Periodic monitoring of the feet, if the PCP is not skilled c. Evaluation and performance of pressure-relieving foot surgeries or transmetatarsal amputation d. Persistent ulcer e. Recurrent ulcer f. Complicated ulcer g. Evaluation and performance of pressure-relieving foot surgeries or amputation. h. Refer to vascular surgeon for abnormal noninvasive studies or nonhealing ulcer i. Refer to plastic surgeon for nonhealing pressure ulcers. Unusual cutaneous conditions and tumors a. Mycosis Fungoides b. Merkel Cell Carcinoma Page 3 of 4 Guideline/Procedure Number: MPUG3061 (previously Lead Department: Health Services UG100361) Guideline/Procedure Title: Scope of Primary Care Dermatology ☒ External Policy and Indications for Referral Guidelines ☐ Internal Policy Original Date: 12/17/2003- Medi-Cal Next Review Date: 08/20/2015 10/18/2006 – Healthy Kids Last Review Date: 08/20/2014 Applies to: ☒ Medi-Cal ☒ Healthy Kids ☐ Employees c. d. e. f. Leiomyosarcoma Dermatofibrosarcoma Protuberans Sebaceous Carcinoma Keratoacanthoma VII. REFERENCES: A. Clinical Dermatology: A Color Guide to Diagnosis and Therapy VIII. DISTRIBUTION: A. PHC Provider Manual B. PHC Department Directors IX. POSITION RESPONSIBLE FOR IMPLEMENTING PROCEDURE: X. REVISION DATES: Medi-Cal 10/20/04; 10/19/05; 10/18/06; 10/17/07; 10/15/08; 11/18/09; 10/01/10; 08/20/14 Healthy Kids 10/18/06; 10/17/07; 10/15/08; 11/18/09; 10/01/10; 08/20/14 PREVIOUSLY APPLIED TO: PartnershipAdvantage: MPUG3061 – 10/18/2006 to 01/01/2015 Healthy Families: MPUG3061 – 10/01/2010 to 03/01/2013 ********************************* In accordance with the California Health and Safety Code, Section 1363.5, this policy was developed with involvement from actively practicing health care providers and meets these provisions: Consistent with sound clinical principles and processes Evaluated and updated at least annually If used as the basis of a decision to modify, delay or deny services in a specific case, the criteria will be disclosed to the provider and/or enrollee upon request The materials provided are guidelines used by PHC to authorize, modify or deny services for persons with similar illnesses or conditions. Specific care and treatment may vary depending on individual need and the benefits covered under PHC. Page 4 of 4