Pediatric Preventive Health

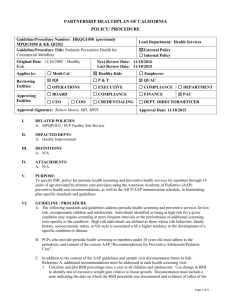
PARTNERSHIP HEALTHPLAN OF CALIFORNIA
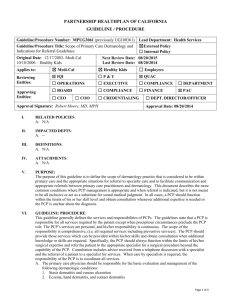
POLICY/ PROCEDURE
Guideline/Procedure Number: MCQG1015 (previously
MPQG1015 & QG100115)
Lead Department: Health Services
Guideline/Procedure Title:
Pediatric Preventive Health
☒
External Policy
☐ Internal Policy
Original Date : 04/25/1994
Applies to:
Reviewing
Entities:
☒
Medi-Cal
☒ IQI
☐ OPERATIONS
Next Review Date: 11/18/2016
Last Review Date: 11/18/2015
☐
Healthy Kids
☐
Employees
☐ P & T
☐ EXECUTIVE
☒ QUAC
☐ COMPLIANCE ☐ DEPARTMENT
☐ BOARD ☐ COMPLIANCE ☐ FINANCE ☒ PAC
Approving
Entities: ☐ CEO ☐ COO ☐ CREDENTIALING ☐ DEPT. DIRECTOR/OFFICER
Approval Signature:
Robert Moore, MD MPH
Approval Date: 11/18/2015
I.
RELATED POLICIES :
A.
MCQP1021 - Initial Health Assessment and Behavioral Risk Assessment
B.
MPQP1022 - PCP Facility Site Review Requirements and Guidelines
II.
IMPACTED DEPTS :
A.
Quality Improvement
III.
DEFINITIONS :
A.
N/A
IV.
ATTACHMENTS :
A.
CHDP Periodicity Schedule
V.
PURPOSE:
To specify PHC policy for periodic health screening and preventive health services for members through 20 years of age provided by primary care providers. The California Department of Health Services requires that all Medi-Cal managed care health plans, including PHC; utilize the current Child Health and Disability
Program (CHDP) and American Academy of Pediatrics (AAP) preventive health care recommendations, as well as the ACIP/AAP immunization schedule, in formulating plan specific standards and guidelines. Since all PHC primary care providers who care for children are expected to be enrolled as CHDP providers, all other CHDP policies related to the provision of pediatric preventive services are applicable as well.
VI.
GUIDELINE / PROCEDURE :
A.
The following standards and guidelines address periodic health screening and preventive services for low risk, asymptomatic children and adolescents. Individuals identified as being at high risk for a given condition may require screening at more frequent intervals or the performance of additional screening tests specific to the condition. High risk individuals are defined as those whose risk behaviors, family history, socioeconomic status, or life style is associated with a higher tendency to the development of a specific condition or disease.
B.
Where the AAP periodicity exam schedule is more frequent than the Child Health and Disability
Prevention (CHDP) periodicity examination schedule, the AAP scheduled assessment must include all components required by the CHDP program for the lower age nearest to the current age of the child. A physical examination is completed at each health assessment visit which includes:
1.
Anthropometric measurements of weight, length/height and head circumference of infants up to age
Page 1 of 4
Guideline/Procedure Number: MCQG1015 (previously
MPQG1015 & QG100115)
Lead Department: Health Services
Guideline/Procedure Title:
Original Date:
Applies to:
04/25/1994
☒
Medi-Cal
Pediatric Preventive Health
☒ External Policy
☐
Internal Policy
Next Review Date: 11/18/2016
Last Review Date: 11/18/2015
☐ Healthy Kids ☐ Employees
24 months.
2.
Physical examination/body inspection, including screen for sexually transmitted infection (STI) on sexually active adolescents.
3.
Follow up care or referral is provided for identified physical and behavioral health problems as appropriate.
C.
In addition to the content of the AAP guidelines in reference A, additional recommendations must be addressed at each health screening visit:
1.
Calculate and plot BMI once a year in all children and adolescents. Use change in BMI to identify rate of excessive weight gain relative to linear growth. Documentation must include a note indicating the date on which the BMI percentile was documented and evidence of either of the following: BMI percentile or BMI plotted on age growth chart. For adolescents 16-20 years on the date of service, documentation of a BMI value expressed as kg/m 2 is acceptable.
2.
Dental screening, including inspection of the mouth, teeth, and gums. PCPs must refer children to a dentist annually, starting at age one.
3.
Tobacco smoking history or exposure a.
Exposure to passive (second-hand) smoke b.
Tobacco used by patient c.
Counsel regarding, or referral, for tobacco use prevention or cessation.
4.
USPSTF (2010) recommends that providers screen children aged 6 years and older for obesity and offer them or refer them to comprehensive, intensive behavioral interventions to promote improvement in weight status.
5.
USPSTF ( 2009) recommends screening of adolescents (12-20) for major depressive disorder
(MDD) when systems are in place to ensure accurate diagnosis, psychotherapy (cognitive-behavioral or interpersonal) and follow–up.
6.
USPSTF (2011) recommends screening for all children at least once between the ages of 3 and 5 years to detect the presence of amblyopia or its risk factors.
D.
PCP’s must endeavor to complete an initial health assessment on all new members within 120 days of enrollment to PHC. If the member was already enrolled in the PCP’s practice and only the insurance coverage changed then any physical, containing all the elements that were done within the previous 12 months may be counted.
E.
Immunizations must be provided according to the current schedule of the Advisory Committee on
Immunization Practices (ACIP), AAP, and the American Academy of Family Physicians (AAFP), as provided in “Recommended Childhood Immunization Schedule,” reference B.
1.
When immunizations are provided at sites other than the PCP’s office, the provider should notify the
PCP’s office of the immunization given and the date.
2.
If this is not possible, the member or parent/guardian of the member must be advised to provide this information to the PCP at the next visit.
3.
PCP office should be requesting previous medical record(s) to show a complete history.
F.
Unless the member has received a periodic health screening visit within the periodicity schedule in reference A, the member, or the member’s parent/guardian, must be informed at the time of each nonemergency primary care visit of the availability of services through the PCP’s practice. If the needed exam qualifies for services through the CHDP program, the member’s parent/guardian should be informed that services are available at the PCP’s practice, or at another site offering CHDP services.
1.
This requirement may be met through the provision of the PHC document Recommendations for
Page 2 of 4
Guideline/Procedure Number: MCQG1015 (previously
MPQG1015 & QG100115)
Lead Department: Health Services
Guideline/Procedure Title:
Original Date:
Applies to:
04/25/1994
☒
Medi-Cal
Pediatric Preventive Health
☒ External Policy
☐
Internal Policy
Next Review Date: 11/18/2016
Last Review Date: 11/18/2015
☐ Healthy Kids ☐ Employees
Preventive Adolescent/Pediatric Care in reference A, or by providing a document of equivalent content.
2.
Should the member not receive periodic health screening services according to the attached schedule, either: a.
The voluntary refusal of the member (or the parent/guardian) regarding the use of CHDP services should be documented in the member’s medical record, or: b.
There should be documentation of an outbound phone call or written communication from the provider to the member advising of the need to schedule a periodic health screening appointment.
3.
In the case where a child scheduled for a periodic health screening visit is not seen as scheduled, the
PCP’s staff should contact the member (or parent/guardian) to reschedule the visit, and document same in the medical record.
G.
Diagnosis and treatment of any medical conditions identified through the periodic health screening
(CHDP) process, either by the PCP or through referral to a specialist, must be initiated within 60 days of identification. Justification for delays beyond 60 days must be entered into the member’s medical record.
H.
Providers must enter their findings in the member’s medical record and complete the CHDP Assessment
Form (PM-160-Information Only). It is not acceptable to use the PM-160 form as the sole medical record of the visit.
1.
A copy of the form must be given to the member or parent/guardian after completion of the visit.
Upon request by the member, or the parent/guardian of the member, the PCP must provide additional discussion or consultation regarding the results of the health assessment.
2.
Completed PM-160 forms must be submitted to PHC within 6 months of the member’s visit.
I.
Parents of children found to have conditions which could constitute eligibility for the California
Children’s Services (CCS) Program must be informed. The PCPs staff should initiate a referral to the county CCS office for eligibility determination.
J.
Monitoring and Quality management
1.
Timeliness and appropriateness of pediatric preventive health will be monitored annually by completing designated HEDIS measures (Childhood Immunization, Adolescent Immunization, Well
Child Visits in the third, fourth, fifth and sixth years of life).
2.
Documentation of children’s/adolescent preventive services will be reviewed periodically as a component of the Facility Site Review.
VII.
REFERENCES:
A.
AAP Recommendations for Preventive Adolescent/Pediatric Care: Access all recommendations on line for free from the links found on: http://brightfutures.aap.org/3rd_Edition_Guidelines_and_Pocket_Guide.html
B.
CDC Recommended Childhood and Adolescent Immunization and Catch-Up Schedule, access current version from link found at: http://www.cdc.gov/vaccines/schedules/hcp/child-adolescent.html
C.
United States Preventive Services-Task Force (USPSTF) current recommendations, American Academy of Pediatrics (AAP) current recommendations, Center for Disease Control (CDC) 2011 Immunization
Schedule
VIII.
DISTRIBUTION :
A.
PHC Department Directors
Page 3 of 4
Guideline/Procedure Number: MCQG1015 (previously
MPQG1015 & QG100115)
Lead Department: Health Services
Guideline/Procedure Title:
Original Date:
Applies to:
04/25/1994
☒
Medi-Cal
Pediatric Preventive Health
☒ External Policy
☐
Internal Policy
Next Review Date: 11/18/2016
Last Review Date: 11/18/2015
☐ Healthy Kids ☐ Employees
B.
PHC Provider
C.
Practitioner Manual
IX.
POSITION RESPONSIBLE FOR IMPLEMENTING PROCEDURE : QI Staff: HEDIS and Facility Site
Review
X.
REVISION DATES:
Medi-Cal
10/13/95; 10/10/97 (name change only); 03/11/98; 5/17/00; 02/20/02; 10/30/02 vs. 10/16/02; 10/20/04;
04/20/05; 10/19/05; 06/21/06; 09/19/07; 03/18/09; 02/17/10; 03/16/11; 10/17/12; 10/16/13; 11/19/14;
11/18/15
PREVIOUSLY APPLIED TO:
PartnershipAdvantage:
MPQG1015 - 09/19/2007 to 10/16/2013
Page 4 of 4