Scope of Primary Care – Behavioral Health & Indications for Referral
advertisement
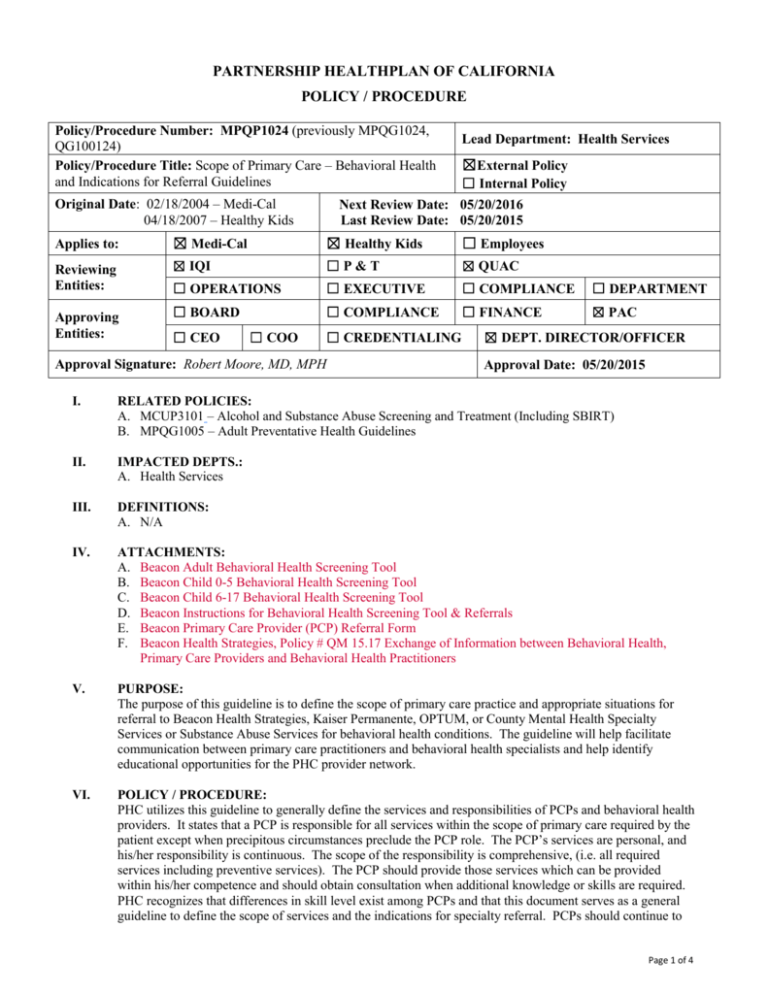
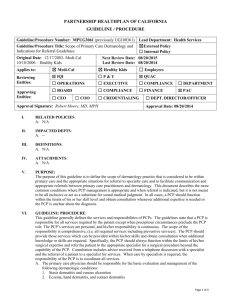
PARTNERSHIP HEALTHPLAN OF CALIFORNIA POLICY / PROCEDURE Policy/Procedure Number: MPQP1024 (previously MPQG1024, QG100124) Policy/Procedure Title: Scope of Primary Care – Behavioral Health and Indications for Referral Guidelines Original Date: 02/18/2004 – Medi-Cal 04/18/2007 – Healthy Kids Lead Department: Health Services ☒External Policy ☐ Internal Policy Next Review Date: 05/20/2016 Last Review Date: 05/20/2015 Applies to: ☒ Medi-Cal ☒ Healthy Kids ☐ Employees Reviewing Entities: ☒ IQI ☐P&T ☒ QUAC ☐ OPERATIONS ☐ EXECUTIVE ☐ COMPLIANCE ☐ DEPARTMENT ☐ BOARD ☐ COMPLIANCE ☐ FINANCE ☒ PAC Approving Entities: ☐ CEO ☐ COO ☐ CREDENTIALING Approval Signature: Robert Moore, MD, MPH ☒ DEPT. DIRECTOR/OFFICER Approval Date: 05/20/2015 I. RELATED POLICIES: A. MCUP3101 – Alcohol and Substance Abuse Screening and Treatment (Including SBIRT) B. MPQG1005 – Adult Preventative Health Guidelines II. IMPACTED DEPTS.: A. Health Services III. DEFINITIONS: A. N/A IV. ATTACHMENTS: A. Beacon Adult Behavioral Health Screening Tool B. Beacon Child 0-5 Behavioral Health Screening Tool C. Beacon Child 6-17 Behavioral Health Screening Tool D. Beacon Instructions for Behavioral Health Screening Tool & Referrals E. Beacon Primary Care Provider (PCP) Referral Form F. Beacon Health Strategies, Policy # QM 15.17 Exchange of Information between Behavioral Health, Primary Care Providers and Behavioral Health Practitioners V. PURPOSE: The purpose of this guideline is to define the scope of primary care practice and appropriate situations for referral to Beacon Health Strategies, Kaiser Permanente, OPTUM, or County Mental Health Specialty Services or Substance Abuse Services for behavioral health conditions. The guideline will help facilitate communication between primary care practitioners and behavioral health specialists and help identify educational opportunities for the PHC provider network. VI. POLICY / PROCEDURE: PHC utilizes this guideline to generally define the services and responsibilities of PCPs and behavioral health providers. It states that a PCP is responsible for all services within the scope of primary care required by the patient except when precipitous circumstances preclude the PCP role. The PCP’s services are personal, and his/her responsibility is continuous. The scope of the responsibility is comprehensive, (i.e. all required services including preventive services). The PCP should provide those services which can be provided within his/her competence and should obtain consultation when additional knowledge or skills are required. PHC recognizes that differences in skill level exist among PCPs and that this document serves as a general guideline to define the scope of services and the indications for specialty referral. PCPs should continue to Page 1 of 4 Policy/Procedure Number: MPQP1024 (previously Lead Department: Health Services MPQG1024, QG100124) ☒External Policy Policy/Procedure Title: Scope of Primary Care – Behavioral Health and Indications for Referral Guidelines ☐Internal Policy Original Date: 02/18/2004 – Medi-Cal Next Review Date: 05/20/2016 04/18/2007 – Healthy Kids Last Review Date: 05/20/2015 Applies to: ☒ Medi-Cal ☒ Healthy Kids ☐ Employees use their sound clinical judgment when considering the need for specialty evaluation. Consultation includes advice received from a telephone discussion with a specialist and the referral of a patient to a specialist for services. When care by specialists is required, it is the responsibility of the PCP and the specialist to coordinate all services. A. The primary care physician should be responsible for providing the following in regards to basic behavioral health conditions: 1. Obtain developmental and psychosocial histories and perform mental status examinations when indicated by psychiatric or somatic presentations. 2. Routinely screening for common behavioral health and substance use conditions. The plan has adopted and PHC contracted providers are expected to follow the USPSTF Guide to Clinical Preventive Services. Routine screening for depression is recommended by the USPSTF. Please refer to the Adult Preventative Policy - MPQG1005 for further details. Screening for alcohol misuse is also recommended. Please refer to Alcohol and Substance Abuse Screening and Treatment (Including SBIRT) – MCUP3101 for details. 3. Determine whether high risk factors such as suicidal or homicidal ideation with active planning, threats of physical harm, or psychomotor agitation, or active substance abuse exist, and/or whether the member can be considered to be gravely disabled. 4. Evaluate and provide ongoing management for the following: a. Psychological factors affecting a medical condition and psychological symptoms precipitated by medications being used to treat medical conditions b. Psychological issues or problems which are conditions such as anxiety, depression and conduct problems that do not meet the criteria for a DSM diagnosable disorder c. Medical assessments of members to evaluate and treat general medical conditions causing or exacerbating psychiatric symptoms. d. Initial diagnosis and treatment of dementia. Differentiate delirium and depression from dementia. Manage general medical factors that improve or worsen dementia. B. The primary care physician should be responsible for the initial evaluation and referral for behavioral health services as follows: 1. Members with Healthy Kids Health Plan in Solano, Sonoma, Yolo, and Marin counties: All levels of mental health services and substance use disorder services are covered by PHC through a contractor: OPTUM. For information on accessing this behavioral health plan contact: 800-718-8430. 2. Members assigned to Kaiser Permanente: Kaiser will provide Mental Health Services in Solano, Sonoma, Napa, Yolo, and Marin counties for mild-to-moderate conditions. 3. Medi-Cal only Members (with no Medicare and not assigned to Kaiser Permanente nor to Healthy Kids Health Plan): All behavioral health services for these members are provided either by Beacon Health Strategies’ network of providers for mild to moderate behavioral health conditions or by County Mental Health Specialty Services or Substance Abuse Services for moderate to severe behavioral health conditions or substance abuse. 4. PCP should determine a provisional diagnosis for the following behavioral health conditions: schizophrenia/psychotic disorder, bipolar depression, depression, anxiety disorder, impulse control disorder, adjustment disorder, personality disorder (except anti-social), eating disorder, pervasive developmental disorder, disruptive behavior/attention deficit disorder, feeding and eating/elimination disorders, other disorders of infancy, childhood, or adolescence, somatoform disorders, factitious disorders, dissociative disorders, paraphilias, gender dysphoria. 5. PCP should determine the level of functional impairment in the following life domains resulting from the behavioral health condition: a. Independent living skills b. Social relations c. Physical condition (chronic medical condition) Page 2 of 4 Policy/Procedure Number: MPQP1024 (previously Lead Department: Health Services MPQG1024, QG100124) ☒External Policy Policy/Procedure Title: Scope of Primary Care – Behavioral Health and Indications for Referral Guidelines ☐Internal Policy Original Date: 02/18/2004 – Medi-Cal Next Review Date: 05/20/2016 04/18/2007 – Healthy Kids Last Review Date: 05/20/2015 Applies to: ☒ Medi-Cal ☒ Healthy Kids ☐ Employees d. Vocational/Employment e. Sexuality f. Self-care g. Decision making h. Legal i. Residential instability 6. PCP should determine the probability of deterioration/risk factors linked to the behavioral health condition such as: a. Psychiatric hospitalization b. Criminal behavior c. Suicidal/homicidal behavior d. Transitional age youth with acute psychotic episode e. Self-injurious behavior that required medical attention f. Sexual aggression with acute risk of re-offending 7. PCP should refer Medi-Cal only members to Beacon Health Strategies when a provisional diagnosis (from III.B.4) is present or the diagnosis is uncertain, where functional impairment is considered to be in mild to moderate range (from III.B.5), and where there are no deterioration/risk factors (from III.B.6) a. PCP may refer for Outpatient Behavioral Health Services for therapy or medication management via Beacon’s network of providers by calling (855)765-9703 or providing the member with this referral number. PCP can also fax a Beacon PCP Referral Form to Beacon at 866-422-3413 or use secure email: medi-calreferral@beaconhs.com Licensed Mental Health Providers at Beacon will screen the patient and determine the appropriate level of care needed and make the actual referrals. b. PCP may request decision support related to member diagnostic and medication clarification, the PCP may request a telephone consultation with a Beacon psychiatrist at (855)765-9703. Before phone consult with Beacon fax medication list and last 2 PCP progress notes for Psychiatrist review. FAX (866) 422-3413 or secure email: medi-calreferral@beaconhs.com c. PCP may refer for Beacon Care Management: local behavioral health care coordination services to help link members to mental health providers, support their transition between levels of care, or engage members with history of non-compliance and link them to community services. FAX (855) 371-2279 or email: Medi-Cal_PHP@beaconhs.com d. Primary care sites with integrated behavioral health, whose mental health professionals are credentialed with Beacon, may co-manage patients that would qualify for the “mild-moderate” mental health benefit. e. After initial evaluation and/or referral the PCP may continue to follow and treat a PHC member based on his/her current clinical competence and in collaboration with the behavioral health specialist as appropriate. 8. PCP should refer members (primarily Medi-Cal only) to County Mental Health Specialty Services when a provisional diagnosis (from III.B.4) is present and when functional impairment is considered to be in the moderate to severe range (from III.B.5), and/or when any risk factor (from III.B.6) is present. a. The process of accessing mental health services in each county may be different. PCPs should consult the PHC website for county-specific details. b. Patients with emergency psychiatric conditions should be referred for emergency evaluation, calling the county-designated crisis phone number to arrange for services. c. After initial evaluation and/or referral the PCP may continue to follow and treat a PHC member based on his/her current clinical competence and in collaboration with the behavioral health specialist as appropriate. Page 3 of 4 Policy/Procedure Number: MPQP1024 (previously Lead Department: Health Services MPQG1024, QG100124) ☒External Policy Policy/Procedure Title: Scope of Primary Care – Behavioral Health and Indications for Referral Guidelines ☐Internal Policy Original Date: 02/18/2004 – Medi-Cal Next Review Date: 05/20/2016 04/18/2007 – Healthy Kids Last Review Date: 05/20/2015 Applies to: ☒ Medi-Cal ☒ Healthy Kids ☐ Employees 9. 10. 11. 12. d. Federally qualified health centers with integrated mental health may provide outpatient services for patients who would otherwise qualify for County Specialty Mental Health Services. These services are billed directly to the state. PCP should screen and refer Medi-Cal only Members with Substance Abuse problems as follows: a. Screening and Brief Intervention for Alcohol misuse should be performed by PCP. b. The process of accessing substance abuse services in each county may be different. First point of contact for substance abuse referrals for each county is found on the PHC website at: http://www.partnershiphp.org/Members/MC_MbrEN.htm#mental toward the bottom of the page under the heading “HELP FOR SUBSTANCE ABUSE.” c. For details on substance abuse screening and referral, see MCUP3101 – Alcohol and Substance Abuse Screening and Treatment (Including SBIRT). d. Provide ongoing follow-up as jointly determined by the PCP and County Substance Abuse provider for members whose substance abuse conditions have reached a high degree of stability. Psychiatric manifestations of neurologic disorders, developmental neurologic disorders, traumatic brain injury, and encephalopathy. A specialist in neuropsychiatry is ideally suited to assist with these cases. Behavioral Health Treatment (BHT) for Medi-Cal only Members: BHT is covered by PHC for Members between the ages of 0-21 years old who have Autism Spectrum Disorder (ASD), including Asperger’s and pervasive developmental disorders. If a child was receiving BHT services through a Regional Center prior to September 15, 2014, these services will continue to be provided through a Regional Center until further notice. Contact PHC’s Member Services Department for further information. School aged children may also have some assessment and treatment covered through their schools. School-based mental health services include a broad range of services, settings, and strategies. These services may include academic counseling, brief interventions to address behavior problems, family counseling, suicide prevention, and assessment and referral to other systems. Further information available through your County mental health department. VII. REFERENCES: A. USPSTF 2014 Guide to Clinical Preventive Services VIII. DISTRIBUTION: A. PHC Provider Manual, B. PHC Directors IX. POSITION RESPONSIBLE FOR IMPLEMENTING PROCEDURE: Senior Health Services Director X. REVISION DATES: Medi-Cal 05/18/05; 04/19/06; 04/18/07; 04/16/08; 03/18/09 11/17/10; 01/16/13; 02/19/14; 05/20/15 Healthy Kids 04/18/07; 04/16/08; 03/18/09 11/17/10; 01/16/13; 02/19/14; 05/20/15 PREVIOUSLY APPLIED TO: PartnershipAdvantage: MPQG1024 – 04/18/2007 to 11/17/2010 MPQP1024 – 11/17/2010 to 01/01/2015 Healthy Families: MPQP1024 - 11/17/10 to 03/01/2013 Page 4 of 4