Through the Eyes of the Client - Client Journey
advertisement
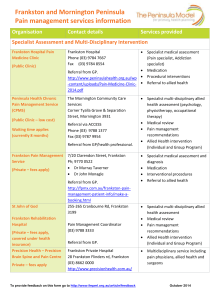
Service System Redevelopment “Through the Eyes of the Client” Client Journey Experiential Study From the client’s perspective From the service providers perspective Presenters: Lyn McKay, Service System Redevelopment Coordinator, FMPPCP Julie White, ICDM Support Officer, FMPPCP/ICDM , Peninsula Health Community Health What am I going to get out of this session? • An understanding of the: – Client Journey processes & challenges that went into the undertaking • Information about: – planning a service system redesign approach – A general framework for the project – Methodologies & tools used – Strategic outcomes Approach • System Wide • Systematic – Start broad – Finish targetted • Well developed implementation plans • Use of robust project management approach/tools • Practical/doable – delivering tangible results at the end • Factual information – not just ‘intuition’ The Study • Documents and analyses the experiences of the service system from the perspectives of both: –Clients –Service Providers • Provides a comparative Study Objectives • Empower clients to: – navigate the service system – manage their needs across the continuum of care • Identify gaps/areas and changes needed to improve the client journey & outcomes • Enable improvements to be made in the health system across the FMP catchment Focus • Central Focus (in keeping with the SSR Plan) –Aging –Anxiety & Depression –Dementia Study – Target Sectors & Populations Mental Health Aged Local Government GPs Drug and Alcohol Acute Sub Acute Community Disability Neighbourhood/ Community Renewal Indigenous Culturally And Linguistically Diverse (CALD) Client Inclusion Criteria • • • • • • • • • Primarily between the ages of 50-80 Multiple agency involvement Multiple co-morbidities Met the profile for the anxiety & depression/dementia focus of the study CALD group Indigenous person Family carer or have a personal/family carer Relevant and current experience of the health system Ability/assisted capacity to express how they think the system could improve Study Scope • 147 Clients • 87 Services / PCP Member agencies Client Sources • • • • • • • • • Brotherhood of St Laurence Frankston Senior Citizens Seagull Day Club – Frankston Baptcare Positive Aging Group, Frankston City Council Access & Mobility Group, Somerville Greek Women’s Group, Rye Indigenous Group, Hastings Villa Maria (home visits) - case managed clients • Telephone Interviews – Peninsula Support Services • Age Strong Study Inclusions • Assessment of: – – – – – – – – Access/intake Exit/discharge Assessment and care planning Referral Care coordination Self management Chronic disease Capacity of organisations – limitations to go beyond presenting issue or service programs – Communication between providers – Strengths and weaknesses of client journey processes for client feedback and quality improvement Methodology • Clients – Focus groups – Questionnaires – Open group discussion – Individual client interviews • Service Providers – Questionnaire – via Survey Monkey • Supported by – clear governance structures – Use of System Frameworks • Victorian Service Coordination Practice Manual • Wagner Model – Project management processes & tools Project Management Processes & Tools • Initial Project Information & Discussion Paper - issues for consideration • Letters to service providers • Service provider project information template • Consultant project discussion information & for quotation template • Working Group Terms of Reference (inc. work-plan) • Project brief • Task team brief • Detailed Implementation Plans and Gantt Chart • • • • • • • • Issues Register Risk Register Learning’s Register Project budget and implementation estimates Reporting frameworks (minutes, actions sheets, SSRC /OMC /SDC Implementation Plan Activity and Outcomes Reports) Project Evaluation Framework Service Providers Questionnaire Clients Questionnaire Study Findings Clients were asked about: • Client demographics • Managing their condition • Getting into services • What has been done to manage their condition • Their experiences of the health system Service Providers were asked about: • Service provider demographics • Service provider client demographics • About structures & processes • Service accessibility • Assessment & Care Coordination • Referral & feedback • Client pathway information Key Themes • Service Access • Listening, noticing & follow up • Effective Communication between Services & Clients • Carers – Involvement • Waiting times and time management • Social Groups • Case Management Key Findings • Clients expect to: –be able to access the services they require in a reasonable period of time –receive help and be looked after –be given information appropriate to their situation "QUESTION: Do you feel you have been given sufficient information about your condition/ illness to manage it? medically yes-well informed / practically-NO" • Clients’ Best experiences of the system were those that: –involved timely responses to clients’ concerns –related to particular programs where the leader provided friendly/appropriate service tailored for the individual client’s needs • Clients’ Worst experiences of the system were those that included: – slow responses/lack of timeliness – apparent lack of concern/interest in individual client – service providers not taking the time to listen or pay proper concern to the client needs and issues Most Important to Clients • Being treated with decency, courtesy, respect • Receiving timely follow through • Being listened to ‘Really heard’, Important Factor • Being involved in social & worthwhile activity together (social inclusion) Who do clients go to as a priority? 1. 2. 3. 4. 5. GP Hospital Pharmacists Community Health Local Government First Priority Second Priority Third Priority Of Interest • Many clients did not see that they actually had a ‘condition’ • Raises issues about the terms used in consultation with clients Key Findings Service Providers • Lack of awareness - internal processes for identification of clients with dementia, depression or anxiety. • More work required to further integrate/streamline access to services for clients. • Many service providers are unsure about, or do not know if their organisation has a monitoring/reminder /recall system • Wide range of timeframes for practitioners seeing clients from when clients first access services • There is evidence of a lack of clarity by service providers around what is ‘Client Focused Care’ • Diverse communication practice exists between service providers and GPs. • Extensive service provider practice variations between referral timeframes & transmission of referral acknowledgements. Perception (by Service Providers) • monitoring of client risk at presentation is supported by consistent practice across service providers regarding: • effective communication of timeframes • eligibility and prioritisation across services …….in accordance with good practice Example Care Plans Service Providers Responses Are your clients actively involved in developing their treatment/care plans? Client Responses Have you been actively involved in developing your treatment/care plan(s)? 20 no. of res pondents 18 16 14 12 10 8 6 4 2 0 V ery involved all of the Involved mos t of the time Involed s ome of the time Not Told w hat involved to do at any no. of res pondents 19 17 1 4 8 % of res pondents 24% 22% 1% 5% 10% Client’s Responses 5% 32% Y es No Uns ure 63% Do you have a treatment/care plan(s)? 4% 38% Y es No Uns ure 58% If Yes, do you have a written copy of your treatment/car e plan(s)? “My ex-wife may have it. There is a written contract but I don’t have it” “My own plan - I belong to a Bushwalking Group and walk 10 km /week” Example - Consent • Most service providers ask for clients consent to share personal details & information – Client perception - they (52%) had not been asked to give consent prior to service providers sharing their information with other services Service Providers Responses Client’s Responses What did we learn? • Processes always take longer than expected • Analysis of data & information generally more complex than often anticipated in early stages of project/data collection phases • Timelines need to be realistic and flexible Project Evaluation • • • • • • • • Governance/Leadership Planning and scoping Stakeholder engagement Risk management Resource management Quality management Reporting System-wide/organisational change management • Impact evaluation • Outcomes/achievements evaluation • Learnings dissemination Outcomes/Impacts of the Client Journey Study • Informed the development of numerous service improvement initiatives such as: – Development & piloting of Broader Needs Assessment tool through the PCP – “Working Together for Better Diabetes Care” Catchment planning initiative • • Informed individual agency service planning Informed Medicare Local discussions & included in MLO submission • Project Review -lessons learned log • Being used for SSR planning – identification of key work priorities for remainder 2011-2012 • PCP strategic planning evidence base • Service providers using for QI purposes • Benchmarking resource for various entities Back to the Future Challenges • Address findings - prioritising • Developing & implementing models of care, access, etc. client focussed care • Affect appropriate change at all levels of organisation & the system • Resourcing FMPPCP Lyn McKay Tel: 9788 1544 Email: lmckay@phcn.vic.gov.au Julie White Tel: 9784 7764 Email: jwhite@phcn.vic.gov.au Copies of the Client Journey Report available at: http://www.peninsulahealth.org.au/healthprofessionals/frankston-morningtonpeninsula-primary-care-partnership/