A Nursing Teams Journey to Implement Teach
advertisement

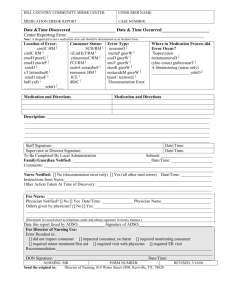
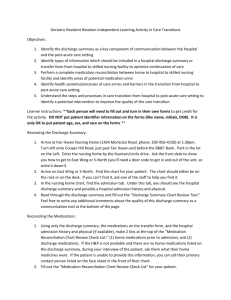
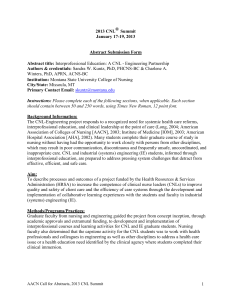
Striving for Patient Centered Education: A Nursing Teams Journey to Implement TeachBack in an Urban Acute Care Hospital Myra L Couch, MSN, RN-BC, CNL, Mary Rudy, MN, RN, NEA-BC, Ellesha McCray, MBA, MSN, RN, NE-BC, Darlene Dietrich, MBA, MSN, RN, Roseanne Zawinski, MSN, RN-BC, Kelly White, MSN, RNBC Veterans Administration Pittsburgh Healthcare System Pittsburgh, PA Email: myra.couch@va.gov Background : U.S. Department of Health and Human Services (HHS) defines health literacy as the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions. The HHS reports that nearly nine out of ten adults may lack the literacy and numeracy skills needed to manage their health and prevent disease. Low literacy has been linked to poor health outcomes, increased likelihood of having chronic conditions which patients are less able to manage, higher rates of hospitalization and excessive usage of emergency services as opposed to preventive care. Aim: Teach-Back is a patient-centered approach for health education which stresses the importance of confirming comprehension of all critical self-care activities. To improve patients understanding of their medications and common side effects, and to increase effectiveness of our discharge process, Teach Back was implemented as standard practice for patient teaching on all inpatient acute care units. Teach Back allows nurses to consistently offer clear, concise instructions as we strive to improve patient knowledge and satisfaction as determined during follow-up discharge phone calls. Methods/Programs/Practices: Implementation of Teach-Back was initiated by the Clinical Nurse Leader (CNL), with full support of the Chief Nurse Executive. The CNL is a master's prepared generalist with experience in evidence based practice programs, team building and quality improvement. The literature and resource review included a recent National Quality Forum report that identified teaching back as one of 50 essential “safe practices” to improve health care and improve efficiency in clinical practice. Our interdisciplinary team, lead by the CNL included nurse managers and nurse educators working collaboratively to plan strategies for classroom education, poster development, just-in-time follow-up training and evaluation. Nurses received video, written, verbal and hands on training in Teach-Back. The American Medical Associations Clinician’s Manual titled “Health Literacy and Patient Safety: Help Patients Understand, was chosen as our primary teaching resource. Medication reconciliation was the primary focus and included patient teaching on right medication, right time, right amount, medication side effects and appropriate responses to adverse events. Teach Back training emphasized reducing the tendency to ask closed ended question like “Do you understand?," provides time for verification of patient comprehension, and promotes using easily understood plain language. Most importantly, Teach Back creates a dialogue between professionals and patients by allowing time for patients to repeat the information in their own words and if needed receive additional teaching. Implementation followed the Plan-Do-Study-Act process. After studying staff and patient responses, plans were updated to include Teach Back in new nursing orientation and as an annual nursing competency beginning in 2013. Outcome Data: Implementation of the Teach Back initiative has spread to 3 nursing units with data analyzed for the past 9 months. Dimensions of care evaluated were “nursing communication about medication” with rates initially increased from 80.6% to 87% and “discharge instructions” with rates increased from 84.6% to 92%. The inpatient acute care units continue to now meet expected goals and show sustainable improvement in these metrics. Please see attached graph. 95 90 85 80 75 70 Apr-12 Mar-12 Feb-12 Jan-12 Dec-11 Nov-11 Jul-11 Aug-11 Sep-11 11-Oct Teach Back Outcomes BLUE=Communication at Discharge RED=Medication Comprehension