Documenting Reporting Informatics - Health Information Technology
advertisement
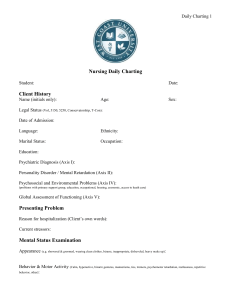
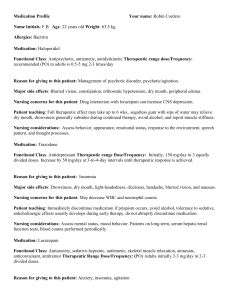
Communication is Vital! Technology is your friend! Accurate: Observations only Do not use subjective words Correct spelling, grammar & med terms Complete: New or changed information S/S, clients behavior Nursing interventions Meds given Physicians orders carried out Client teaching and response to therapy Consistent Objective Concise and brief using approved abbreviations Important when documenting psychosocial and mental health issues Legible Writing must be clear and easily read by others Line out errors: 100 cc clear yellow urine from foley Organization Use nursing process Timelines Document care, treatments, procedures and medications as soon as possible Purpose of documentation: Communication Assessment Care planning Quality assurance Reimbursement Legal documentation Research Education Technology in healthcare is advancing Information will be managed electronically Outcomes: Safe patient care Patient centered care Improved outcomes Ease of access to information Workflow Forms use a standardized language Radio buttons, drop-down boxes Data driven Mandatory fields Charting by exception Increases compliance Alerts to abnormal findings Able to document all aspects of nursing care EHR/EMR Monitoring Imaging Medication administration Pharmacy Clinical Decision Support Systems ADT CPOE Central supply ordering systems Elements that reduce human error: CPOE Bar Code High Alert Medication Documentation Point of Care Documentation Mandatory Fields Smart Pumps Communication Tool Admission History and Assessment Discharge Form Nursing Care Plans Flow Sheets/graphic sheets Kardex Clinical Pathways Medication Administration Records (MAR) Nursing Progress Notes Patient education form Acuity charting Incident report Does NOT go in pt chart! HIPAA Purpose Techniques Content Situation Background Pt What name Age Physician’s name Diagnois Hospital day/POD # brought them to the hospital Past medical history Situation Background Assessment Recommendation/ Request Often a framework for communicationcalling MD, giving report, etc Assessment State what you think is the problem Give review of symptoms Recommendation or Request What needs to be done What was done Plan for discharge Information written in sentences or phrases usually time sequenced Must Many write a narrative note q2 hrs combined with flow sheets Document only findings that fall outside of “normal” Flow sheet with check boxes Assessment findings, routine care activities Narrative notes only when there is an exception or abnormal finding Eliminates redundancy