Patient Safety
advertisement

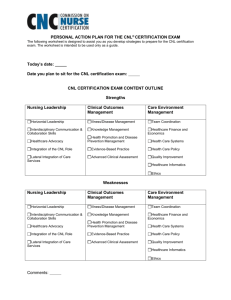
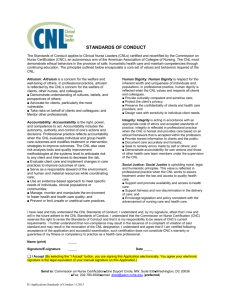
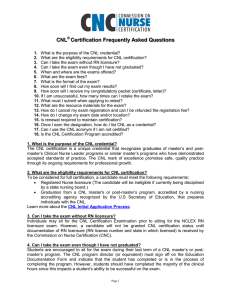
Clinical Nurse Leader Workshop: Leadership/Systems Dr. Kia James, EdD, RN, CNL CLINICAL NURSE LEADER • How did the role come about? • What were precipitating factors/studies/reports that helped innovate this new role? • What is this role supposed to do? • Define the role 10 Assumptions for cnl role 1. 2. 3. 4. 5. Practice at the microsystems level Client care outcomes are measure of quality practice Practice guidelines are evidence-based Client centered practice is INTRA- and INTER-discplinary Information will maximize self-care and client decisionmaking 6. Nursing assessment is the basis for theory and knowledge development 7. Good fiscal stewardship is a condition of quality care 8. Social justice is an essential nursing value 9. Communication technology will facilitate the continuity and comprehensiveness of care 10. The CNL must assume guardianship for the nursing profession. 10 Assumptions for cnl role 1. 2. 3. 4. 5. Practice at the microsystems level Client care outcomes are measure of quality practice Practice guidelines are evidence-based Client centered practice is INTRA- and INTER-discplinary Information will maximize self-care and client decisionmaking 6. Nursing assessment is the basis for theory and knowledge development 7. Good fiscal stewardship is a condition of quality care 8. Social justice is an essential nursing value 9. Communication technology will facilitate the continuity and comprehensiveness of care 10. The CNL must assume guardianship for the nursing profession. HEALTH CARE SYSTEMS AND ORGANIZATIONS • Systems theory • Traditional organizational theory • Hierarchy • Scientific management • Traditional role of nursing in health care system • New theories to attend to growing complexities of health care system System Levels Example Frontline Patient Care Units Microsystem Nursing Divisions Mesosystem Nursing Services Macrosystem Source: Henriks, Bojestig, Jonkoping CC Sweden Key functions as a leader in the CNL Role • Horizontal leadership • Effective use (and knowledge) of self in caring and facilitating change for patients • Advocacy • Conceptual analysis of CNL role • Lateral integration of care for a unit of care/population Leadership • Leadership practice at the microsystems level • Leadership vs. Management • Leadership theories: • • • • • • Great Man Situational Leadership style Servant leadership Transformational leadership Complexity science leadership New ORG Theories for health care system • Learning organization theory • Chaos theory • Complexity science theory • Change theories: • Lewin’s force field • Roger’s - Diffusion of innovation model • Complexity science – strange attractor • New role for a new organization: CNL • The Clinical Nurse Leader is the frontline change agent in health care organizations ORG THEORIES for Health care systems Learning organizations • Organizations are living and thinking open systems that learn from experience and engage in complex mental processes. Theorist: Peter Senge The Learning Organization • Adaptive (single-loop) Learning • Involves coping with a situation • Limited by the scope of current organizational assumptions • Occurs when a mismatch between action and outcome is corrected without changing the underlying values of the system that enabled the mismatch. • Generative (double-loop) Learning • Moves from COPING to CREATING an improved organizational reality • Necessary for eventual survival of the organization • Both are central features to the learning organization • Synergy and nonsummativity are Important The Learning Organization • Through communication, teams are able to learn more than individuals operating alone. • Leadership is a key element in creating and sustaining a learning organization. • Leaders are responsible for promoting an atmosphere conducive to learning • CREATIVE TENSION New Directions in Org theories for health care Chaos theory • Every complex system has a life of its own, with its own rule book. • Change is normal – chaos is part of change – look for the patterns that emerge out of the chaos • Fractals Theorists: Fritjof Capra New Directions in Systems Thinking Organizations as Complex Adaptive Systems aka Complexity Science Theory – Leadership and the New Science (Wheatley, 2006). • Organizations are adaptive, living organisms with a life of their own • Not predictable yet adaptable • Complex systems are self-organizing. • Small changes can have big effects • Relationships are all there is • Information is the life force of any organization • It is normal for organizations to grow, die and reinvent themselves • A static organization is a “dead” organization Lewin’s change theory Force Field Analysis Begin change by analyzing the entire system in order to identify the forces for and against the change: driving & restraining forces Need to add driving forces or remove restraining forces Change Model Unfreezing Change Refreezing (Lewin, 1951) Rogers’ (1995) Diffusion of Innovation Stages of adoption: Awareness - the individual is exposed to the innovation but lacks complete information about it Interest - the individual becomes interested in the new idea and seeks additional information about it Evaluation - individual mentally applies the innovation to his present and anticipated future situation, and then decides whether or not to try it Trial - the individual makes full use of the innovation Adoption - the individual decides to continue the full use of the innovation Roger’s Diffusion of Innovation Model Positive Deviance • Identifies change process by looking at the solution first then designing the change process around success • • • • Define Determine Discover Design • Answers the question: • What enables some members of the community (the “Positive Deviants”) to find better solutions to pervasive problems than their neighbors who have access to the same resources? Traditional vs PD Problem Solving Approach Flows from problem analysis towards solution Flows from identification and analysis of successful solution to problem solving Fixed Solution Space Perceived Problem Parameters PD Perceived Problem Parameters Traditional Perceived Problem Parameters Actual Problem Actual Problem Parameters Parameters Expanded Solution Space Actual Problem Parameters why focus on the “clinical microsystem?” • Basic “building block” of health care as a system. • Where “good value” and “safe” care are made. • Unit of clinical policy-in-use. • Where most health professional “formation” occurs after initial preparation. • Locus of most workplace “motivators” and many “demotivators” • It’s the front line • Most variables relevant to patient satisfaction controlled here. • It’s where everything happens with, to and for the patient and family 20 The CNL Can assess the Clinical Micro-system with the “5 Ps” • Purpose • Patients • Professionals • Processes • Patterns Nelson, Splaine, Godfrey, et al, JQI, Dec. 2000. 21 HEALTH CARE QUALITY & Patient safety • Institute for Healthcare Improvement (2004) Patient Safety Initiative • Apply methods and tools of industrial quality improvement • Process improvement and team problem solving Quality • Must be defined & measured • Is a moving target - must always be current • Provides a competitive edge • Doing things “right” the first time • Focus on results - outcomes • Must be strongly embedded in culture • Must be linked to costs Quality Improvement IOM Report (Crossing the Quality Chasm) recommends six dimensions as potential themes for quality improvement: 1. Safety 2. Effectiveness 3. Patient-centeredness 4. Timeliness 5. Efficiency 6. Equity Quality improvement Tools and Techniques • PDCA • Plan-Do-Check-Act • Plan-Do-Study-Act (Deming, 1993) • Other Problem-solving tools • Process mapping • Flow charts • Check sheets • Pareto analysis • Cause and effect diagrams • PDSA • Objective • Questions and predictions (why) • Plan to carry out the cycle (who, what, where , when) •What changes are to be made? •Next cycle? ACT STUDY •Complete the analysis of the data •Compare the data to predictions •Summarize what was learned PLAN DO •Carry out the plan •Document problems and unexpected observations •Begin analysis of the data AONE: Core Patient Safety Technology Competencies • Systems: Process management & process improvement • Human factors • Failure Mode Effects Analysis/Root cause analysis • Safety rounding • Teaming • Risk management Failure mode effects analysis (FMEA) • FMEA purpose: Eliminate or reduce failures/harm • Failure mode – manner in which failure occurs and is observed • Failure effect – consequences of failure (prioritized by severity) • Root cause analysis • Common cause analysis When Solving Problems… • Focus on prevention, not blame • Realize a cause never stands alone • A problem description is not analysis • Start analysis with an impact to the goals not the causes • Apply the basics of cause and effect, avoid buzzwords • Analyze all - not only problems but success to determine cause and effect (Galley, 2007) Client centered practice is intra- and inter-disciplinary • Effective communication skills – listen, listen, listen • Team coordination and collaboration • • • • • Delegation and supervision Interdisciplinary care and roles of the health care team Group process Handling difficult people Conflict Resolution • Leadership is all about communication Social justice • An essential value for the CNL • Demonstrated through compassion, cultural competence, patient advocacy and an understanding of health disparities • Support that health is a “right” not a “privilege” CNL is the Guardian of the Nursing profession • CNL role is helping professional nursing to evolve to a higher level of maturity and complexity • CNL role helps to maintain focus of all activities on patients and their well-being/safety • CNL role continues to demonstrate that nursing is more than just a job – it’s a vocation • CNL role exemplifies the responsibility of knowledge workers in an information society References • American Association of Colleges of Nursing (2007). White paper on education and the role of the Clinical Nurse Leader. Washington, DC: American Association of Colleges of Nursing. • Institute of Medicine (2000). To err is human: Building a safer health system. Washington, DC: National Academy Press. • Institute of Medicine (2001). Crossing the quality chasm: A new health system for the 21st century. Washington, DC. National Academy Press. • Nelson, E. C., Batalden, P. B. & Godfrey, M. M. (2007). Quality by design: A clinical Microsystems approach. San Francisco: Jossey-Bass. • Wheatley, M. (2006). Leadership and the new science: Discovering order in a chaotic world 3rd ed. San Francisco: Berrett-Koehler.