ret 2835 respiratory care clinic 4 - MDC Faculty Home Pages
advertisement

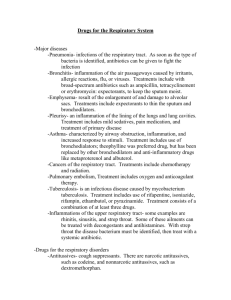
Miami Dade College Medical Campus School of Health Sciences Respiratory Care Program RET 2835 Respiratory Care Clinic 4 (Revised: April 2015) MIAMI DADE COLLEGE MEDICAL CAMPUS SCHOOL OF HEALTH SCIENCES RESPIRATORY CARE PROGRAM COURSE OUTLINE RET 2835 RESPIRATORY CARE CLINIC 4 COURSE OVERVIEW: RET 2835 is designed to allow the student to develop psychomotor skills related to critical care procedures of Respiratory Care. The student is responsible for all objectives in prerequisite and co-requisite courses. During the course, the student is provided with the opportunity to apply and discuss the theory and techniques as learned in prerequisite and co-requisite courses. Clinic Days: _____________________ Clinic Location: ________________________ Clinic Location: ______________________ Instructor: ______________________ Office #: ______________________________ Phone #: ______________________ Beeper #: _____________________________ Office Hours: __________________________________________________________ EVALUATIONS: 1st Clinic Evaluation 40% 2nd Clinic Evaluation 40% Case Study 10% Case Presentation 10% RET 2835 TABLE OF CONTENTS MODULE 1.0 MONITORING TECHNIQUES MODULE 2.0 NEONATES MODULE 3.0 PEDIATRICS MODULE 4.0 HYPERBARIC MEDICINE MODULE 5.0 SUBACUTE CARE MODULE 6.0 SPECIALIZED CRITICAL CARE MODULE 7.0 CASE PRESENTATION MODULE 1.0 MONITORING TECHNIQUES General Objective: Upon completion of the module, the student will understand various monitoring techniques, invasive and non-invasive, utilized in critical care. Specific Objectives: 1.1 Describe the balancing and calibration procedure for the transducer pressure systems used in hemodynamic monitoring 1.2 Identify the components that comprise an arterial line monitoring system and pulmonary artery catheter monitoring system 1.3 Identify precautions in preparing and setting up an arterial line and pulmonary artery catheter 1.4 Describe the technique for drawing blood specimens from arterial line and pulmonary artery catheter 1.5 Explain the daily maintenance required for a transducer pressure monitoring system 1.6 List the parameters that can be monitored using an arterial line and pulmonary artery catheter 1.7 Differentiate between the various pressure readings and waveforms associated with arterial line and pulmonary artery catheter 1.8 Compare and contrast the hemodynamic data presented by patients to normal values and identify the cause and effect of that data. MODULE 2.0 NEONATES General Objective: Upon completion of the module, the student will understand the various techniques and procedures utilized with neonates in the critical care area. Specific Objectives: 2.1 Identify normal ABG and CBG values for a newborn 2.2 Explain the different assessment scales utilized in the assessment of an infant at birth (APGAR, etc.) 2.3 Demonstrate skills in collection and evaluation of nursing and respiratory care data from the patient chart and flow sheet 2.4 Identify important steps to take in the stabilization of a distressed newborn 2.5 Describe and demonstrate neonatal CPR techniques, based upon current American Heart Association and American Academy of Pediatrics standards and obtain Neonatal Resuscitation Program (NRP) and Pediatric Advanced Life Support (PALS) certification. 2.6 Explain techniques of oxygen administration to newborns, and identify the responsibilities of the respiratory care practitioner in oxygen administration to the newborn 2.7 Develop an explanation of the etiology, pathophysiology, and treatment of neonatal pathology/conditions including: 1. 2. 3. 4. 5. 6. 7. 8. HMD IVH ROP (RLF) RDS II PFC/PPHN BPD IRDS Apnea of prematurity 2.8 Explain the rationale for and implement the type of ventilation plans and programs used on newborns in the intensive care unit, particularly the use of IMV, high frequency ventilation, and inverse I:E ratios 2.9 Explain and demonstrate special considerations in the use of bag/mask and bag/tube ventilation in the newborn 2.10 Describe and demonstrate techniques for both arterial and capillary sampling 2.11 Discuss the indications, contraindications and hazards of nitric oxide therapy 2.12 Discuss the physiological aspects of nitric oxide (INO) therapy and implement therapy 2.13 Demonstrate safe setup and use of equipment used to provide and monitor nitric oxide therapy 2.14 Discuss the indications, contraindications, hazards and physiological aspects of Extracorporeal Membrane Oxygenation (ECMO) 2.15 Identify the equipment used and the procedure for initiating Extracorporeal Membrane Oxygenation (ECMO) 2.16 Explain the rationale and techniques for the use of transcutaneous monitors and pulse oximeters, and compare their use to that of serial arterial sampling as a tool for the continuous evaluation of oxygenation and ventilation status 2.17 Interpret ABG/CBG results on a variety of patients in the intensive care unit, and discuss changes in oxygen administrations and/or ventilator parameters, based upon the interpretation with the respiratory care practitioner 2.18 Participate in physician/patient therapist/patient rounds 2.19 Discuss the importance of thermal regulation in neonates and implement appropriate procedures. 2.20 Discuss and demonstrate the indications, use of, and contraindications of exogenous surfactant in the newborn 2.21 Explain the problems associated with fluid balance in the neonate and recommend corrective action as appropriate. MODULE 3.0 PEDIATRICS General Objective: Upon completion of the module, the student will understand procedures related to the care and treatment of the pediatric patient in the critical care area. Specific Objectives: 3.1 Identify the common pathologies found in the pediatric population 3.2 Differentiate among oxygen therapy equipment and techniques used on pediatric patients 3.3 Identify and discuss pharmacological agents used in the pediatric population including brand and generic name, dosage, actions, contraindications, indications, hazards, and adverse reactions 3.4 Define the specific disease entity or condition of assigned children in the pediatric critical care area 3.5 Describe the hospital course of treatment for the disease or condition and justify its appropriateness or inappropriateness 3.6 Discuss the indications and patient needs for continuous mechanical ventilation 3.7 Utilizing the patient's chart, investigate data appropriate to the child's clinical status 3.8 Participate in physician/therapist and therapist/patient rounds MODULE 4.0 HYPERBARIC OXYGEN THERAPY (HBO) General Objective: Upon completion of this module, the student will have a basic understanding of HBO and its clinical utilization, and chamber operation. Specific Objectives: 4.1 Define hyperbaric oxygen and hyperbaric medicine 4.2 Discuss the physical and physiological aspects of HBO 4.3 Compare and contrast monoplace and multiplace chambers 4.4 Identify and discuss the criteria utilized during a "dive " procedure 4.5 Review the clinical indications for HBO 4.6 Identify and discuss problems/hazards associated with HBO 4.7 Review the operation of a multiplace and monoplace chamber 4.8 Discuss the role of transcutaneous oxygen and perfusion measurement in HBO MODULE 5.0 SUBACUTE CARE General Objective: Upon completion of the module, the student will have an understanding of the type of patient and routine of care found in the subacute setting. Specific Objectives: 5.1 Describe the major types of patients and pathologies encountered in the subacute setting 5.2 Discuss the routine of care including medical and respiratory care 5.3 Monitor patients receiving continuous mechanical ventilation 5.4 Effectively and safely provide all types of respiratory care as ordered by a physician and as appropriate to established protocol 5.5 Compare the routine of care in the subacute setting to the acute setting 5.6 Describe the role of the respiratory care practitioner in the subacute setting 5.7 If utilized, discuss the use of therapist driven protocols (TDP) in the subacute setting MODULE 6.0 SPECIALIZED CRITICAL CARE General Objective: Upon completion of the module, the student will have an understanding of the type of patient and routine of care found in the specialized critical care settings of Trauma Intensive Care, Surgical Intensive Care (including transplant and open heart), Neurologic/Neurosurgical Intensive Care, and Medical Intensive Care. Specific Objectives: 6.1 Describe the major types of patients and pathologies encountered in each of the specialized critical care settings 6.2 Discuss the routine of care including rounds, medical and respiratory care 6.3 Monitor patients receiving continuous mechanical ventilation in each of the specialized critical care settings 6.4 Effectively and safely provide all types of respiratory care as ordered by a physician and as appropriate to established protocol, in each of the specialized critical care settings 6.5 Compare and contrast the routine of care in the each of the specialized critical care settings to the routine of care found in other acute care settings 6.6 Describe the role of the respiratory care practitioner in each of the specialized critical care settings 6.7 If utilized, discuss the use of therapist driven protocols (TDP) in each of the specialized critical care settings MODULE 7.0 – CASE PRESENTATION During this clinical rotation, the student will present a critical care patient case study. It shall be typed in the approved format and must be submitted in hard copy (paper) form. The care study will contribute towards the student's clinic grade. The patient selected for the case presentation must meet the following criteria: 1. Patient must be on some form of mechanical ventilation 2. Patient should have a pulmonary artery catheter inserted (exceptions can be made with permission from the Director of Clinic Education [DCE]) 3. Case studies may be chosen from the following patient groups: a. Adult ICU b. Pediatric ICU c. Neonatal ICU d. A homecare, ventilator-dependent patient with a unique diagnosis, e.g., ALS The written case presentation can be no longer than five typed double space pages in 12-point Arial font. Margins must be no greater than 1 inch on both sides and bottom and top. It will be written in the narrative form (except for Section Two). ALL CASE PRESENTATIONS ARE DUE ON: _________________. PRESENTATIONS WILL NOT BE ACCEPTED AFTER THIS DATE. The student is responsible to provide information on the selected patient from the date of admission up the last date of the student’s rotation at the facility. If the selected patient is transferred from the ICU and/or expires, the student will present the time period from the date of admission to the date of transfer or expiration. CASE PRESENTATION FORMAT The case presentation will be divided into three sections: Section One: Introduction, Section Two: Assessment Section Three: Conclusion. Each section must be identified in the paper. Each will have specific information that the student will obtain from a number of sources including the patient's chart, nursing flow sheet, ventilator flow sheet, and the student’s own knowledge base. Section One: Introduction The content of this phase should be developed from information gathered from the patient's chart and your interpretation of that information. It should contain the name of the hospital/facility the patient was admitted to, patient age, sex, date of admission, chief complaint on admission, diagnosis, findings on physical examination and history, and respiratory status. The information and the manner in which you present this information should develop both Section Two and Section Three. The information you have presented here should be consistent which your information listed in Section Two and discussed in Section Three. Section Two: Assessment This portion of the case presentation should contain a synopsis of the patient's hospital stay from date of admission to present. This time span may be as little as one day to as much as several weeks, depending upon the patient you have selected. The information in this section may be listed according to the numbered categories that follow. Data for this phase should come from a variety of sources, including the patient's chart, personal assessment of the patient, nursing flow sheet, etc. This section should contain the following information: 1. Indication(s) for patient needing ventilatory assistance or support (related to diagnosis, surgery, etc.) 2. Number of days on the ventilator 3. Type of ventilator ( brand name and classification) 4. Type of ventilatory program instituted ( orders, progress, changes) 5. Respiratory Care orders 6. Summary of ABG's (results must be accompanied by interpretations) 7. All other respiratory care being given to the patient 8. Briefly describe chest x-ray findings (initial and present) 9. What respiratory related medications the patient is receiving (name, type, route, dosage, indication) 10. Other drug therapy that the patient is receiving (name, type, route, dosage, indication) 11. Summary of fluid balance (including pulmonary artery catheter findings) 12. Major medical problems and/or conditions (non respiratory) Section Three: Conclusion The content of this phase should be developed primarily from direct evaluation of your patient and patient information. This section will contain the "How and Why" of your presentation. A concise, organized overview of the medical and cardiopulmonary orders, status, and assessment made by you should be developed in this section. Be sure to include your rationale for agreement and/or disagreement with the patient's medical and respiratory care plan. It should contain what you interpret as the outcome of the current medical and cardiopulmonary regimen.