Cross-matching
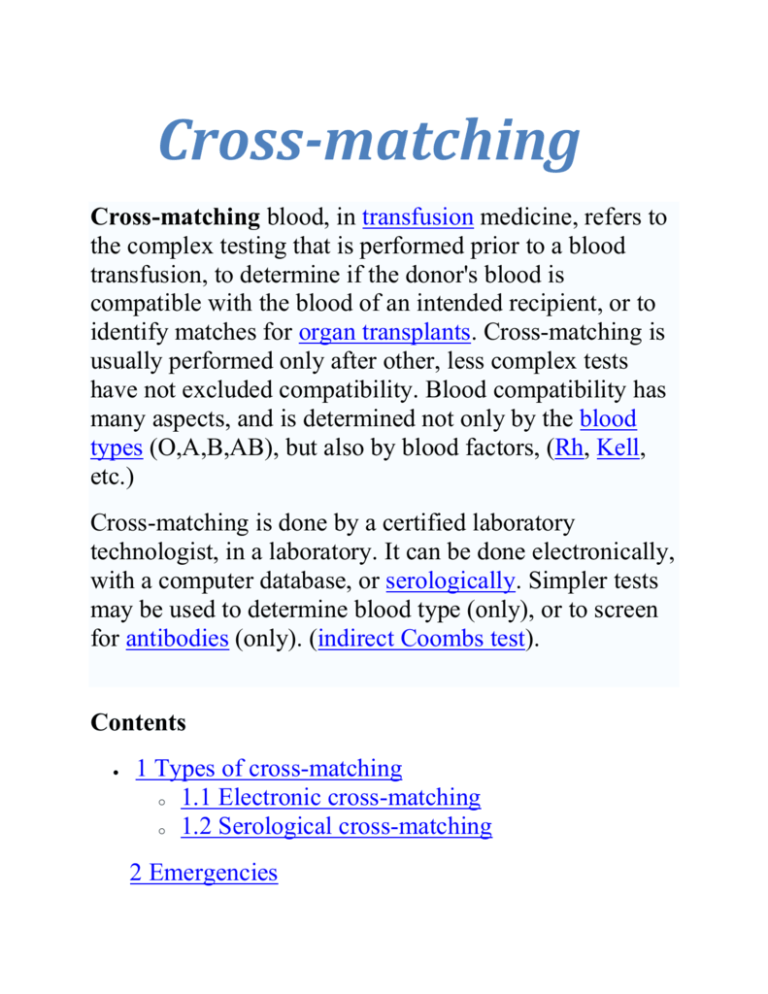
Cross-matching blood, in transfusion medicine, refers to
the complex testing that is performed prior to a blood
transfusion, to determine if the donor's blood is
compatible with the blood of an intended recipient, or to
identify matches for organ transplants. Cross-matching is
usually performed only after other, less complex tests
have not excluded compatibility. Blood compatibility has
many aspects, and is determined not only by the blood
types (O,A,B,AB), but also by blood factors, (Rh, Kell,
etc.)
Cross-matching is done by a certified laboratory
technologist, in a laboratory. It can be done electronically,
with a computer database, or serologically. Simpler tests
may be used to determine blood type (only), or to screen
for antibodies (only). (indirect Coombs test).
Contents
1 Types of cross-matching
o 1.1 Electronic cross-matching
o 1.2 Serological cross-matching
2 Emergencies
Types of cross-matching
Electronic cross-matching
Electronic cross-matching is essentially a computerassisted analysis of the data entered from testing done on
the donor unit and blood samples drawn from intended
recipient. This includes ABO/Rh typing of the unit and of
the recipient, and an antibody screen of the recipient.
Electronic cross-matching can only be used if a patient
has a negative antibody screen, which means that they do
not have any active red blood cell atypical antibodies, or
they are below the detectable level of current testing
methods. If all of the data entered is compatible, the
computer will print a compatibility label stating that the
unit is safe to transfuse.
Serological cross-matching
In serological cross-matching, red blood cells from the
donor unit are tested against the plasma of the patient in
need of the blood transfusion. If the patient’s serum
contains antibodies against the antigens present on the
donor red blood cells, agglutination will occur.
Agglutination is considered a positive reaction indicating
that the donor unit is incompatible for that specific
patient. If no agglutination occurs the unit is deemed
compatible and is safe to transfuse.
Emergencies
In the case of an emergency a physician can request
"uncross-matched blood", or donor units of blood that
have not been cross-matched. It is thought that this
lifesaving measure is of more benefit than any risk of an
antibody-mediated transfusion reaction. In addition, the
risk of a serious transfusion reaction can be minimized if
the donor unit is both ABO-compatible and Rhesus (Rh)compatible. Type O and Rh negative blood can be given
if the recipient's blood group is not known, as may happen
in an emergency. In an emergency, blood grouping can be
done easily and quickly in 2 or 3 minutes in the laboratory
on glass slides with appropriate reagents, by trained
technical staff. This method depends on the presence or
absence of agglutination, which can usually be visualized
directly, although occasionally a light microscope may be
needed. If laboratory services are not available, another
system of deciding which type of blood to use in an
emergency is the bedside card method of blood grouping,
where a drop of the intended recipients' blood is added to
dried reagents on a prepared card. This method may not
be as reliable as laboratory methods, which are preferable.
Disclaimers
CROSSMATCH
General Information
The Crossmatch also known as compatibility testing,
pretransfusion testing or type and crossmatch (Type and
Cross; T & C). The definition of a compatibility test
(crossmatch) is a series of procedures use to give an
indication of blood group compatibility between the
donor and the recipient and to detect irregular antibodies
in the recipient's serum.
The main purpose for performing a crossmatch is to
promote (not ensure) the safe transfusion of blood. We are
performing testing to the best of our ability that will
demonstrate that the donor blood is compatible with the
recipient's blood. Crossmatch procedures should be
designed for speed and accuracy - get the safest blood
reasonably possible available to the patient as soon as
possible. In summary, the AABB Technical Manual
states the goals of a compatibility test is to:
Detect as many clinically significant antibodies as
possible
Detect as few clinically insignificant antibodies as
possible
Complete the procedure in a timely manner. (p. 379)
Once donor blood is crossmatched with a potential
recipient, the results of the crossmatch is good only 3
days. If the physician wants the donor blood available
longer, we must get a new recipient sample and repeat
tests. This protocol helps detect new antibodies that may
be forming, especially when patient has been transfused
within past three months.
Parts of the Crossmatch
The AABB Standards for Blood Banks and Transfusion
Services requires that certain procedures are performed
before blood is transfused to a recipient:
Identification of the recipient and recipient blood sample
is crucial since the major of the hemolytic transfusion
reactions are due to errors in patient or sample
identification.
ABO and Rh typing of the recipient's blood and resolving
any ABO discrepancies. If the discrepancy can not be
resolved before the patient needs the transfusion type O
blood should be given. If problems arise with the D
testing, Rh negative blood should be given.
Performing an antibody screen on the recipient's serum
for clinically significant antibodies. These antibodies are
most likely to occur in the 37oC and AGT phases of
testing. Each negative AGT test must be followed by
"Coombs Control Check Cells." An autocontrol may or
may not be used. Some labs prefer to perform this
routinely during the antibody screen while others will
only include it if an antibody needs to be identified. The
autocontrol has to be part of the antibody identification
procedure. The SOP of each institution must be followed
by all individuals performing these tests.
Comparing present findings with previous records for the
recipient. If previous testing has been performed on the
recipient and should match current testing. These
comparisons can give assurance that no identification
errors have occurred, but it is not proof. Records would
also show if clinically significant antibodies have been
detected in the past. These antibodies may be presently at
undetectable levels. Any history of clinically significant
antibodies, even if undetectable now in the patient,
dictates an antiglobulin phase crossmatch needs to be
done between the recipient's serum and the donor's cells.
Confirmation of the ABO and Rh type of the red cell
components being given when the shipment of blood is
received in the laboratory.
Selection of appropriate ABO and Rh component units for
the recipient first would be the same ABO and Rh type.
Transfused donor red cells must be ABO compatible with
the patient's plasma and whatever antibodies may be
present. Transfused plasma must be ABO compatible
with the recipient's red cells. AABB Technical Manual's
Table 18-2
Selection of Components When ABO-Identical Donors
Are Not Available, p 385
ABO Requirements
Whole Blood Must be identical to that of the recipient
Red Blood Cells (most plasma removed)
compatible with the recipient's plasma.
Granulocytes, Pheresis
recipient's plasma.
Must be
Must be compatible with the
Fresh Frozen Plasma Must be compatible with the
patient's red cells.
Platelets, Pheresis
All blood groups acceptable;
components compatible with the recipient's red cells
preferred
Cryoprecipitated AHFAll ABO groups acceptable
Rh-positive components should be given to Rh-positive
individuals and Rh-negative units should be reserved for
D-negative individuals. The physician needs to be
involved in any decisions relating to giving Rh-positive
blood to an Rh-negative individuals since those
individuals have an 80% chance of making an anti-D
following transfusion.
Perform a crossmatch either serologically or via a
computer. If no clinically significant antibodies are found
in the recipient the institution has the option of choosing
an immediate-spin crossmatch (serologic technique) or a
computer crossmatch. If clinically significant antibodies
are found, an antiglobulin crossmatch must be performed.
Label the components with the recipient's identifying
information
Type and Screen
The type and screen consists of ABO/Rh, antibody screen,
and a records check. This order is used when likelihood
of needing blood is low. Therefore, no donor blood
crossmatched to patient. If need for blood suddenly
arises, you can take sample that is already typed and
screened, and perform a crossmatch with donor units from
the specimen. Type and screen protocol cannot be used
if patient has an antibody. Then an antiglobulin
crossmatch must be performed.
Benefits of a Crossmatch
Performing a crossmatch before transfusing blood has the
following benefits:
Detects major ABO errors (ie. crossmatching an A donor
with an O or B recipient )
Detects most recipient antibodies to antigens on donor red
cells (if the antibody is in high enough titer to react) One
of the most common clinically significant antibodies that
are missed are the Kidd antibodies.
Limitations of a Crossmatch:
A crossmatch also has limitations:
Will not detect errors in patient identification (unless a
previous record exists)
Will not detect ABO mix-ups if blood types are
compatible (can crossmatch group A donor blood for an
AB recipient)
Will not detect Rh errors (can crossmatch Rh+ donor
blood with Rh negative recipient with no reaction if the
patient has no anti-D)
Will not detect all recipient antibodies to donor antigens
(antibody may be too weak to detect, but still cause
transfusion reaction such as the Kidd antibodies)
Will not prevent alloimmunization of recipient (only
ABO and Rh antigens matched - patient can potentially
make antibody to all the other antigens) This is why
many of the discovered antibodies are found in multitransfused patients.
Immediate Spin versus Antiglobulin, Coombs,
Crossmatch
The purpose of Immediate spin step of crossmatch is to
detect major ABO incompatibility between donor and
recipient. ABO incompatibility is the most common lifethreatening type of transfusion reaction and is often due to
clerical errors.
It is permissible to stop at immediate spin step of
crossmatch if:
Immediate spin is negative and
Antibody screen is negative in all phases and
There is no record of previous antibodies
It is NOT permissible to stop at the immediate spin step
and you must incubate and carry crossmatch through
antiglobulin, Coombs, phase if:
Immediate Spin test agglutinated or
Patient has an antibody (screening cells are positive) or
Patient has a record of a previous antibody
Benefits of an Immediate Spin only crossmatch:
Makes blood available to patient faster
More cost-effective
90% of patients are eligible for immediate-spin
crossmatches
Electronic or Computer Crossmatch As An Alternative to
the immediate-spin crossmatch
An institution may choose to perform computer
crossmatches instead of an immediate-spin crossmatch.
They must meet specific criteria in order to do electronic
crossmatches. Electronic crossmatches have no mixing
of patient serum and donor cells in test tube - computer
verifies ABO/Rh compatibility of donor and recipient
Computer system must be FDA-approved and validated
to do this
Patient ABO/Rh must have been typed at least twice - by
two different technologists
Patient has no antibodies and no record of previous
antibodies
Donor information must be bar-coded into computer
inventory for accuracy
Computer does not allow use of donor unit until its
ABO/Rh is verified
Computer does not allow issue of ABO/Rh incompatible
blood
Crossmatch Problems:
OBJECTIVES - COMPATIBILITY TESTING
Discuss the steps in compatibility testing and explain
their purpose.
Discuss the reasons for compatibility testing.
Discuss the limitations of compatibility testing.
Explain what a Type and Screen consists of, and when it
would be used.
Explain when a LISS-Coombs crossmatch would be done
versus an immediate-spin crossmatch.
Explain what an electronic crossmatch is.
Describe what additional testing must be done when
crossmatching a patient with an antibody.
Describe how to determine the number of units to
screen when crossmatching blood for a patient with an
antibody
Discuss how to resolve the following problems
encountered in compatibility testing:
Test results not matching previous records
Screening cells positive at room temperature, negative in
Coombs
Screening cells positive in Coombs only - new antibody
Screening cells positive in Coombs only - previously
identified antibody
Screening cells positive both at RT and in Coombs
Negative screening cells, but records show a previouslyidentified antibody
Negative screening cells but crossmatch positive at
immediate spin
Positve autocontrol
State how long you may keep blood crossmatched,
before having to get a new sample and repeat the test
Chart Of A-B-O Blood Donor & Recipient Compatibility
RECIPIENT
D
O
N
O
R
Antibodies
Alleles &
O
anti-A
anti-B
A
anti-B
B
anti-A
AB
None
O
None
None
None
None
A
Clump None
B
Clump Clump None
AB
Clump Clump Clump None
Clump None
None
Chart of A-B-O Blood Donor-Recipient Compatibility. Serious problems may arise when the antibodies of
the recipient clump the blood cells of the donor. [The reverse scenario is not as serious because the
antibodies of the donor are diluted by the recipient's blood volume.] Clumping of the donor's blood is
indicated by the word "Clump" in the red squares. No clumping of the donor's blood is indicated by the
word "None" in the green squares. None also denotes the lack of anti-A or anti-B antibodies in the type
O recipient. It is clear from this chart that the "universal donor" is type O, while the "universal recipient"
is type AB. If you include the Rh factor, then the universal donor becomes O Negative while the universal
recipient becomes AB Positive.
Simplified Explanation For Rh Blood Factor
Rh Neg
Blood
Add a drop of anti-Rh antibodies (anti-D serum) to a drop of blood
on a slide labeled Rh. The Rh negative blood (shown above) will
not clump, while the Rh positive blood (below) will show clumping:
Rh Pos
Blood
Placing the Rh slide on a warming box will hasten the agglutination reaction. Backlighting will also make
it easier to see the clusters of agglutinated red blood cells that appear like minute grains of sand in the
blood. Rocking the slide back and forth also makes it easier to see the grainy texture of the agglutinated
blood.
An Rh Blood Typing (Warming) Box.
Remember that the anti-Rh serum will only agglutinate the positive D factor. There are technically three
positive genes called C, D and E. The negative alleles for these three genes are usually denoted by small
case c, d and e. This is an example of multiple gene (polygenic) inheritance which is explained in more
detail at the following URL:
Multiple Gene Inheritance In The Rh Factor
Although it is much more complicated, the Rh blood factor can be explained by a pair of alleles on
homologous chromosome pair #1. The dominant Rh positive gene (+) produces the Rh antigen, a
glycoprotein constituent of the RBC membrane (see above Rh positive RBC illustration). Like the type O
gene, the recessive Rh negative gene (-) does not produce an antigen. The following table summarizes
Rh inheritance in humans:
Blood Phenotype
Blood Genotype
Antigen on
RBC Membrane Immune (IgG)
Antibodies
Rh Positive
(85% of U.S.)
+ + or + -
Rh antigen
None
Rh Negative
(15% of U.S.)
--
No antigen
May Produce
anti-Rh
If Rh positive blood is accidentally given to an Rh negative recipient, the recipient will begin producing
anti-Rh antibodies. Because of the time factor involved in building up a concentration (titre) of
antibodies, the first transfusion may not cause any major problems; however, a subsequent transfusion
of Rh positive blood could be very serious because the recipient will clump all of the incoming blood
cells. The donor-recipient scenario with Rh blood types is summarized in the following table:
Donor
Recipient
Anti-Rh Antibodies
in Recipient's Blood
Rh Positive
Rh Negative Will Produce
anti-Rh Antibodies
Rh Negative
Rh Positive
Will Not Produce
anti-Rh Antibodies
Since Rh negative people may produce anti-Rh antibodies, Rh positive blood should not be given to an
Rh negative recipient. Based upon the above table, Rh positive recipients can theoretically receive
positive or negative blood, and Rh negative donors can theoretically give to Rh positive and Rh negative
recipients. Therefore, the "universal donor" is O Negative, while the "universal recipient" is AB Positive.
Anti-Rh (immune-type) antibodies can readily pass through the placental capillary membranes. A serious
potential problem called maternal-fetal blood incompatibility or Rh Disease could occur with a pregnant
Rh negative mother who carries an Rh positive fetus. Leakage of fetal red blood cells (RBCs) into the
mother's system through minute lesions in the placenta may cause her to produce anti-Rh antibodies.
This could occur during the latter months of pregnancy or when the baby is delivered. Because of the
time interval involved in producing a concentration (titre) of antibodies, the first Rh positive child may
not be adversely affected. However, a subsequent Rh positive child may be at risk because the mother's
anti-Rh can pass through the placenta, thus entering the fetal circulatory system and clumping fetal
RBCs.
The medical term for this maternal-fetal condition is "erythroblastosis fetalis" because of the presence
of nucleated, immature RBCs called erythrobasts in the fetal circulatory system. The fetus bone marrow
releases immature erythroblasts because of the destruction of mature RBCs (erythrocytes) by the
mother's anti-Rh antibodies. RhoGam®, a serum containing anti-Rh antibodies, is now given to Rh
negative woman within 72 hours after giving birth to their Rh positive baby. The RhoGam® enters the
mother's circulatory system and destroys any residual fetal positive RBCs that may be present in her
system. This prevents her from producing anti-Rh antibodies. RhoGam® must be given after each Rh
positive baby. In this scenario of erythroblastosis fetalis, the fetus must be Rh positive, the mother Rh
negative and the father Rh positive. You can easily determine the exact genotype of the mother and
fetus, but the father's genotype could be homozygous or heterozygous Rh positive. Rh incompatibility is
summarized in the following table:
Rh Pos Father
+ + or + -
X
Rh Neg Mother
- 1st Rh Pos Child
+ Rh positive RBCs from the fetus enter the mother's circulatory system.
After several days, the mother begins to produce anti-Rh antibodies.
2nd Rh Pos Child
+ Anti-Rh antibodies from mother pass through placenta and enter fetal
circulatory system. The antibodies begin clumping fetal positive RBCs.
There are also reported cases of maternal-fetal blood incompatibility with the A-B-O blood groups;
however, the Rh factor appears to be much more common. The larger anti-A and anti-B antibodies (IgM
type) with molecular weights of 950,000, apparently don't penetrate the placental membranes as
readily. In the case of A-B-O blood incompatibility, the anti-A and anti-B antibodies of a type O mother
may enter the circulatory system of a Type A or Type B fetus, thus causing agglutination of the fetal
RBCs. If the fetal blood cells just happened to be Rh positive and entered the mother's circulatory
system, they would be destroyed by the mother's anti-A or anti-B antibodies before her system began to
produce anti-Rh immune-type (IgG) antibodies. In this latter case, the anti-A or anti-B antibodies would
actually serve as a natural immunity to Rh maternal-fetal blood incompatibility.
Like most topics in biology, the true life explanation is a lot more complicated. Rh inheritance is no
exception. It actually involves three different pairs of genes at three different loci on homologous
chromosome pair #1. The gene pairs are C & c, D & d and E & e. The terms "positive" and "negative"
essentially refer to the D factor, so homozygous DD and heterozygous Dd are positive, while
homozygous recessive dd is negative. For a more in depth explanation of this interesting example of
polygenic inheritance, please refer to the following hyperlink:
Rh Factor: Another Example Of Polygenic Inheritance
Rh Factor: Another interesting example of polygenic inheritance is the Rh factor. Unlike the A-B-O blood
types where all the alleles occur on one pair of loci on chromosome pair #9, the Rh factor involves three
different pairs of alleles located on three different loci on chromosome pair #1. In the following diagram,
3 pairs of Rh alleles (C & c, D & d, E & e) occur at 3 different loci on homologous chromosome pair #1.
Possible genotypes will have one C or c, one D or d, and one E or e from each chromosome. For
example: CDE/cde; CdE/cDe; cde/cde; CDe/CdE; etc.
In order to determine how many different genotypes are possible, you must first determine how many
different gametes are possible for each parent, then match all the gametes in a genetic checkerboard
(See the following Table 3). Although the three pairs of genes are linked to one homologous pair of
chromosomes, there are a total of eight different possible gametes for each parent: CDE, CDe, CdE, Cde,
cDE, cDe, cdE, and cde. This number of gametes is based on all the total possible ways these genes can
be inherited on each chromosome of homologous pair #1. [It is not based on the random assortment of
these genes during meiosis in the parents because all three genes are closely linked together on the
same chromosome; therefore, all three genes tend to appear together in the same two gametes: CDE
and cde.] The possible different genotypes are shown in the following Table 3:
Gametes
CDE
CDE
CDE/
CDE
CDE/
CDe
CDE/
CdE
CDE/
Cde
CDE/
cDE
CDE/
cDe
CDE/
cdE
CDE/
cde
CDe
CDe/
CDE
CDe/
CDe
CDe/
CdE
CDe/
Cde
CDe/
cDE
CDe/
cDe
CDe/
cdE
CDe/
cde
CDe
CdE
Cde
cDE
cDe
cdE
cde
CdE
CdE/
CDE
CdE/
CDe
CdE/
CdE
CdE/
Cde
CdE/
cDE
CdE/
cDe
CdE/
cdE
CdE/
cde
Cde
Cde/
CDE
Cde/
CDe
Cde/
CdE
Cde/
Cde
Cde/
cDE
Cde/
cDe
Cde/
cdE
Cde/
cde
cDE
cDE/
CDE
cDE/
CDe
cDE/
CdE
cDE/
Cde
cDE/
cDE
cDE/
cDe
cDE/
cdE
cDE/
cde
cDe
cDe/
CDE
cDe/
CDe
cDe/
CdE
cDe/
Cde
cDe/
cDE
cDe/
cDe
cDe/
cdE
cDe/
cde
cdE
cdE/
CDE
cdE/
CDe
cdE/
CdE
cdE/
Cde
cdE/
cDE
cdE/
cDe
cdE/
cdE
cdE/
cde
cde
cde/
CDE
cde/
CDe
cde/
CdE
cde/
Cde
cde/
cDE
cde/
cDe
cde/
cdE
cde/
cde
Polygenic inheritance in the Rh blood factor. Every genotypic combination with DD or Dd is classified as
Rh Positive (red). This is about 85% of the U.S. population because the D gene is more common than the
C and E genes. Every genotypic combination with dd is classified as Rh Negative (blue). Since the ratio of
C and E genes is much less than D genes, approximately 15% of the U.S. population are Rh negative (dd).
Consolidating the duplicates, a total of 10 genotypes are homozygous recessive for the d allele (dd);
however, nine of these genotypes are actually positive for the C and E factors: Cde/cde (0.46%),
Cde/Cde (0.0036%), cdE/cde (0.38%), cdE/cdE (0.0025%), Cde/cdE (0.006%), CdE/cde (0.008%), CdE/Cde
(0.0001%), CdE/cdE (0.0001%), and CdE/CdE (0.00001%). Therefore, only about 0.86% of the U.S.
population are positive for C and E. Expressed as a decimal, this is 0.0086 or 8.6 out of 1000. This is why
Rh incompatibility involving the C and E genes is rare in the U.S. population.
Other Examples Of Polygenic Inheritance
Antigen
Immune Antibodies (In Blood Plasma)
(RBC Membrane)
anti-C
anti--D
anti-E
C (RhC)
------
------
------
D (RhD)
------
RhoGAM & Biology TypingSerum
E (RhE)
------
------
------
------
Rh antibodies primarily utilized in immunoglobulin serums.
More than 98% of all cases of hemolytic disease of the newborn (maternal-fetal blood incompatibility)
are caused by the D antigen, also referred to as RhD and Rh Positive (+). This is why RhoGam and
standard blood typing kits for general biology labs only contain anti-RhD (anti-D) antibodies. Anti-C and
anti-E antibodies against the C and E antigens can be associated with maternal-fetal blood
incompatibility, but this is uncommon and only occurs in a small percentage of non-RhD cases.
Apparently immune globulins (such as RhoGam) are not available to prevent these rare cases. According
to Dr. Kenneth J. Moise, Jr., Director of the Division of Maternal-Fetal Medicine at University of North
Carolina Medical School at Chapel Hill, more than 43 other RBC antigens have been implicated in the
non RhD cases. Especially problematic are the Kell (K1), c, Duffy (Fya) and Kidd (Jka and Jkb) antigens. A
recent study from a tertiary referral center in New York found 550 cases of antibodies associated with
hemolytic disease of the newborn in 37,506 blood samples taken from women of reproductive age
(1.1% incidence). Anti-D occurred in 25% of the samples, anti-Kell in 28%, anti-c in 7%, anti-Duffy in 7%,
anti-Kidd in 2%, anti-E in 18%, anti-C in 6%, anti-MNS in 6%, and anti-Lutheran in 2%. The following link
contains a summary of Rh maternal-fetal blood incompatibility from the UNC Department of Obstetrics
and Gynecology:
Information Abou
University of Iowa
Hospitals and Clinics
00979071757102
w w w .medicine.u
COURSES/HOME
PLANNING
NEWSLETTERS
FORID:11
Search
ABOUT
FAQ
Hematology in the Physician Office Laboratory Section I
Practice Test (No Cost) | CME Credit Test (20 module Course Registration =
425.00)
Kathleen Kelly B.S., MT(ASCP)
Objectives
Section I
I. Introduction
II. Samples
III. Complete Blood Count (CBC)
A. Table Top Analyzers
1. Cell Counts
2. Hemoglobin
3. Hematocrit
4. Correlating Hemoglobin and Hematocrit Values
5. Comparing Automated and Manual Hematocrits
B. Manual Methods
1. Cell counts
2. Hematocrits
a. quality assurance
3. Hemoglobins
C. Red Cell and Platelet Indices
Objectives
Kathleen Kelly B.S., MT(ASCP)
Upon completion of this module, the participant will be able to:
1. State the preferred anticoagulant for most hematologic testing.
2. Discuss the most common principles utilized in table top hematology analyzers.
a. Cell counts
b. Hemoglobin
c. Hematocrit
3. Briefly discuss sources of error in CBC results.
a. Cell counts
b. Hemoglobin
c. Hematocrit
4. Correlate hemoglobin and hematocrit results.
5. Discuss the use and reliability of hemacytometer cell counts, centrifuged hematocrits, and alternative
hemoglobin procedures.
6. Discuss the centrifuged hematocrit, including sources of error, preventive maintenance, and quality control.
7. Discuss the differences between automated and centrifuged hematocrits.
8. Discuss the derivation and use of red cell indices.
Section Top | Title Page
I.Introduction
Kathleen Kelly B.S., MT(ASCP)
Hematology testing has long been part of the Physician office laboratory testing. Historically, the centrifuged
hematocrit has been one of the most popular laboratory tests. The value of this test has not diminished; however
the availability of cost-effective tabletop instrumentation has put the manual hematocrit in the back seat.
Simple equipment that requires minimal operator intervention has made a complete blood count (CBC) readily
available. The through put of these instruments is fast enough to give cell counts, indices, hemoglobin, hematocrit,
and even a differential in the same time it takes to perform a manual hematocrit. Most of the instruments
currently marketed to physician office laboratories are specifically designed to be user friendly and can be
purchased with ready to use charts and procedures for the required preventive maintenance and quality
assurance.
This unit will discuss the hematology testing most often done in a physician office laboratory. The intent is to
discuss general information on instrumentation and commonly performed tests. Specific manufacturer's
information will not be included. This can be obtained from the individual manufacturer.
Section Top | Title Page
II. Samples
Kathleen Kelly B.S., MT(ASCP)
Sample procurement is addressed in the phlebotomy module, but proper sample handling can not be over
emphasized. Most hematology testing is done on blood anticoagulated with di- or tri- potassium EDTA (ethylene
diamine triacetic acid). Laboratories in the U.S.A. have commonly used K3EDTA in liquid form in a glass or plastic
tube. The International Council for Standards in Hematology recommends K2EDTA sprayed on the walls of plastic
collection tubes.1 The decision to change anticoagulants requires consideration of manufacturer's directions,
reference laboratory preferences, reference ranges, and available literature.
Bullet tubes, with EDTA, are available for collecting blood from skin punctures. The bullet tube must fill quickly and
the blood mixed with the EDTA before coagulation begins. The quality of the skin puncture sample is very
technique dependent.
Samples collected in EDTA must be well mixed at the time of draw and before sampling. The correct mixing time
before sampling is five minutes on an aliquot mixer or, if they are mixed manually, a minimum of sixty inversions.
However, avoid over mixing. Prolonged mixing on aliquot mixers causes hemolysis.
As a safety precaution, always open evacuated tubes under a protective shield.
Residual vacuum causes
aerosols.
1. Recommendations of the ICSH for EDTA anticoagulation of blood for blood cell counting and sizing. Amer J Clin
Pathol. 1993:100:371
Brunson D, Smith D, Bak A, et al. Comparing hematology aK2EDTA vs. K3EDT. Laboratory Hematology 1995, 1:112119.
Section Top | Title Page
Protective Shields
Kathleen Kelly B.S., MT(ASCP)
These are examples of freestanding protective shields. They are available through laboratory supply and safety
product distributors. Previous Page |
Section Top |
Title Page
III. Complete Blood Count (CBC)
Kathleen Kelly B.S., MT(ASCP)
The CBC is the meat and potatoes of hematology. Over the years, the components of the CBC have expanded, as
the instrumentation has become more sophisticated. The CBC test menu on basic instruments usually includes cell
counts (red cells, white cells, and platelets), hemoglobin, hematocrit, and red cell indices. More complex
instrumentation adds automated differentials, platelet indices, and white cell differentials. Performing complete
blood counts using multiple manual or semi-automated methods is no longer cost or time effective. The manual
and semi-automated methods are useful for measuring single parameters and as back up procedures.
A. Table Top Analyzers
These analyzers vary in the extent of the automation involved. The simplest analyzers require the operator to mix
the sample and present an open sample tube to the instrument. Sampling units that pierce the cap of the tube
save time, are readily available, and are safer. The more sophisticated systems read bar coded labels, mix, and
sample through the cap of the tube. Skin puncture samples may need to be diluted and/or presented to a different
sampling probe. The ease of testing skin puncture samples and 2 or 3 ml tubes may be an important consideration
in choosing an instrument. The top of the line hematology systems can make peripheral smears, store thousands
of results, and store and manipulate quality control data. Most of the instruments can be interfaced with a
laboratory information system.
The following URLs will connect to some of the manufacturers of table top hematology analyzers.
1. http://www.beckmancoulter.com/products/instrument/hematology/actseries.asp
Beckman Coulter
2. http://www.bayerdiag.com/
Bayer Diagnostics
3. http://www.sysmex.com/usa/ourbusiness/ourbusiness.cfm?dis_id=1
Dade Sysmex
Section Top | Title Page
1. Cell Counts
Kathleen Kelly B.S., MT(ASCP)
On any given instrument, all of the cell counts are based on the same principle. The Coulter (principle of electrical
impedance or a modification is the most common principle used in the smaller hematology instruments. This
principle is based on the ability of the saline diluent to conduct electricity while the suspended cells are
nonconductive. As the cells pass through an aperture they break the current between the external and internal
electrode and are enumerated and sized. Red cells and white cells are counted in separate baths or channels, with
the red cells lysed when white cells are counted. Platelets are usually counted with the red cells and the cells are
differentiated by size. All cells are reported in units per volume of whole blood.
Red cell histograms
derived from these counts have a small tail to the right of the curve. This
represents coincidence, which is multiple cells passing through the aperture at the same time. The correction for
coincidence takes place in the cell count calculation and is not a concern.
The other basic counting principle is based on light scatter. Here, a single cell passes through a beam of light from a
laser or tungsten-halogen light source. The cell is counted as it breaks the beam of light and the light is scattered.
The scattered light is measured and translated into cell size. The counts are reported in units per volume of whole
blood.
Some hematology instrumentation prints the red cell and platelet histograms as part of the report. These
histograms give a visual interpretation of the cell population and correlate with the indices.
A third type of instrument is advertised as a dry system that works by centrifugation. It generates the cell counts,
hemoglobin, and hematocrit from a centrifuged specimen. These are light, portable instruments made by Becton
Dickinson. The rest of this discussion does not apply to this type of instrument.
Sources of error in cell counts include:
1. Cold agglutinins - low red cell counts and high MCVs can be caused by a decreased number of large red cells or
red cell agglutinates.
If agglutinated red cells are present, the automated hematocrits and MCHCs are also
incorrect. Cold agglutinins cause agglutination of the red cells as the blood cools. Cold agglutinins can be present in
a number of disease states, including infectious mononucleosis and mycoplasma pneumonia infections. If red cell
agglutinates are seen on the peripheral smear, warm the sample in a 37 degrees C heating block and mix and test
the sample while it is warm. Strong cold agglutinins may not disperse and need to be redrawn in a pre-warmed
tube and kept at body temperature.
2. Fragmented or very microcytic red cells
these may cause red cell counts to be decreased and may flag
the platelet count as the red cells become closer in size to the platelets and cause an abnormal platelet histogram.
The population is visible at the left side of the red cell histogram and the right end of the platelet histogram.
3. Platelet clumps
and platelet satellitosis
- these cause falsely decreased platelet counts.
Platelet clumps can be seen on the right side of the platelet histogram. Decreased platelet counts are confirmed by
reviewing the peripheral smear. Always scan the edge of the smear when checking low platelet counts.
4. Giant platelets
- these are platelets that approach or exceed the size of the red cells. They cause the
right hand tail of the histogram to remain elevated and may be seen at the left of the red cell histogram.
5. Nucleated red blood cells
- these interfere with the WBC on some instruments by being counted as
white cells/lymphocytes
Red cell histograms - histograms are derived by plotting the size of each red cell on x axis and the relative number
on the y axis. They are used to determine the average size, distribution of size, and to detect subpopulations.
Section Top | Title Page
Red Cell Histogram
Kathleen Kelly B.S., MT(ASCP)
Red cell histograms are derived by plotting the size of each red cell on x axis and the relative number on the y axis.
They are used to determine the average size, distribution of size, and to detect subpopulations. This histogram
represents a normal red cell distribution. The small tail to the right of the curve represents coincidence, multiple
cells passing through the aperture at the same time. Previous Page |
Section Top |
Title Page
Agglutinated Red Blood Cells
Kathleen Kelly B.S., MT(ASCP)
The arrow points to a red cell agglutinate. Previous Page |
Section Top |
Title Page
Microcytic and Fragmented Red Cells
Kathleen Kelly B.S., MT(ASCP)
Previous Page |
Section Top |
Title Page
Red Cell and Platelet Histograms
Kathleen Kelly B.S., MT(ASCP)
The black curves on the red cell and platelet histograms indicate ìexpectedî or normal cell distributions. The red
curves demonstrate the effect of very microcytic red cells on the histograms. Since microcytic red cells only effect
the right end of the platelet curve, the black and red lines are superimposed for most of the curve. Previous Page |
Section Top |
Title Page
Platelet clumps
Kathleen Kelly B.S., MT(ASCP)
There is a large clump of platelets in the center of the field. Previous Page |
Section Top |
Title Page
Platelet Satellitosis
Kathleen Kelly B.S., MT(ASCP)
The neutrophils in the center of the field are surrounded by platelets. This is an uncommon phenomenon seen in
EDTA samples. The platelets surround the neutrophils and "stick". This results in a false decrease in the platelet
count. Previous Page |
Section Top |
Title Page
Giant Platelets
Kathleen Kelly B.S., MT(ASCP)
Platelets that are 6 microns in diameter or larger, are considered giant platelets. Multiple giant platelets are visible
in this field. Previous Page |
Section Top |
Title Page
Red Cell and Platelet Histograms
Kathleen Kelly B.S., MT(ASCP)
The black curves on the red cell and platelet histograms indicate "expected" or normal cell distributions. The red
curves demonstrate the effect of giant platelets on the red cell and platelet histograms. Previous Page |
Section Top |
Title Page
Nucleated Red Blood Cells
Kathleen Kelly B.S., MT(ASCP)
The two nucleated cells are immature red cells that have been released from the bone marrow ahead of schedule.
Previous Page |
Section Top |
Title Page
2. Hemoglobin
Kathleen Kelly B.S., MT(ASCP)
Hemoglobin, on most automated systems, is measured as cyanmethemoglobin. This is a long-standing method
that reliably measures all the hemoglobin variants except sulfhemoglobin. However, some manufacturers indicate
that their instruments now include sulfhemoglobin in the total hemoglobin measurement.
Red cells are lysed and potassium ferricyanide oxidizes hemoglobin to methemoglobin, which combines with
potassium cyanide forming cyanmethemoglobin. The brown color is measured spectrophotometrically and the
corresponding hemoglobin reported. The end point of the reaction is stable and the reaction is linear to 20 g/dL or
higher. Reagents for cyanmethemoglobin are light sensitive and poisonous.
However, the Sysmex systems can use a sulfhemoglobin methodology to measure total hemoglobin. The reagent
sodium lauryl sulfate disrupts the red cell membrane and binds to the globin chains, causing methemoglobin to be
formed. This binds to the sulfate group producing a conjugate with an absorption peak at 535 nm. No hazardous
waste is produced.
Common sources of error in measuring hemoglobin include anything that will cause turbidity and interfere with a
spectophotometric method. Examples are a very high WBC or platelet count, lipemia and hemoglobins that are
resistant to lysis, such as hemoglobins S and C. The hemoglobin will be falsely increased with turbidity.
Manufacturer's guidelines address interferences.
A simple method for obtaining a hemoglobin value from a lipemic sample is to use plasma replacement.
Plasma replacement - centrifuge a whole blood specimen and remove the plasma with an automatic pipettor.
Record the volume removed and, with the same pipettor and a clean tip, replace the exact volume removed with
isotonic saline. Mix the sample well and retest.
Section Top | Title Page
3. Hematocrit
Kathleen Kelly B.S., MT(ASCP)
A hematocrit is the volume of the red cells as compared to the volume of the whole blood sample. Hematocrits on
the automated systems are calculated. The volume of each red cell is measured as it is counted and a mean cell
volume is derived. The calculations are not precisely the same. But, they can be summarized as mean corpuscular
red cell volume (MCV) multiplied by the red cell count (RBC). Hematocrits are reported in L/L or the traditional %.
When electrolyte displacement is used, the resulting hematocrit is sometimes called the CCV, or conductance cell
volume.
Hematocrits calculated by automated instruments depend on correct red cell counts and red cell volumes to arrive
at an accurate hematocrit. Hence, anything affecting the red cell count or volume measurement will affect the
hematocrit. This method is not as sensitive to the ratio of blood to EDTA as the centrifuged hematocrit. Since the
red cells are resuspended in isotonic saline, they regain their normal shape and size. The practical side of this is
that a reliable automated hematocrit can frequently be obtained from a short sample.
It is very useful to have a hematocrit centrifuge for back up. It can be used when the main instrument is down and
to trouble shoot or check hemoglobins that do not correlate with the other results.
short sample - an evacuated tube that is not full or does not have enough blood to satisfy the manufacturer's
recommended anticoagulant to blood ratio.
Section Top | Title Page
4. Correlating Hemoglobin and Hematocrit Values
Kathleen Kelly B.S., MT(ASCP)
The hemoglobin times three roughly equals the hematocrit in most patients.
Example:
14.8 x 3 = 44 (patient's hematocrit result is 45 L/L)
11.0 x 3 = 33 (patient's hematocrit result is 32 L/L)
The exception to this rule is in patients with hypochromic red cells.
These patients will have hematocrits
that are more than three times the hemoglobin.
Hypochromic red cells- red cells that have an increased zone of pallor on Wright's stain. These cells contain
decreased hemoglobin for their size and have a decreased MCHC.
Section Top | Title Page
Hypochromic Red Cells
Kathleen Kelly B.S., MT(ASCP)
Hypochromic red cells have an increased zone of pallor on Wright's stain. These cells contain decreased
hemoglobin for their size and have a decreased MCHC. Previous Page |
Section Top |
Title Page
5. Comparing Manual and Automated Hematocrits
Kathleen Kelly B.S., MT(ASCP)
Understanding the differences in hematocrit methodology helps explain why some patient's hematocrits vary
more than others do when comparing an automated hematocrit with a centrifuged hematocrit. Theoretically,
measuring each red cell and adding those volumes to get a total red cell volume is the most accurate method.
However, we use the centrifuged hematocrit as our "gold standard" and may even calibrate the automated
hematocrit to match the packed cell volume (PCV). Centrifuged hematocrits have a built in bias due to the trapped
plasma. When red cells have very abnormal shapes, this trapped plasma may be increased enough to cause a
significant change in the centrifuged hematocrit. Some studies have shown that the two methods show better
correlation if K2EDTA is used as the anticoagulant.
Understanding how the automated hematocrit is derived is very important when trouble shooting or using back up
methods such as a centrifuged hematocrit. If the hematocrits appear incorrect on the automated equipment, it
means that the MCV and/or red cell count are also suspect. If a centrifuged hematocrit is substituted for an
automated value, the MCV must be manually calculated.
Section Top | Title Page
1. Cell Counts
Kathleen Kelly B.S., MT(ASCP)
The UNOPETTE® (system has made manual cell counts much easier and more reliable, but hemacytometer cell
counts are still very technique dependent. Manual cell counts should always be diluted and counted in duplicate.
The two WBC dilutions must match within 10% and platelet dilutions must match within 20%. Manual platelet
counts are more difficult than manual white cell counts, especially without the aid of a phase microscope.
Errors occur in all three steps of the procedure; diluting, plating, and counting. Dilution errors occur when the
pipettes are under-filled, not wiped correctly, or blood is left in the neck of the reservoir. Plating errors include
errors in expelling well-mixed sample, filling technique, and handling the hemacytometer between filling and
counting. Scanning each chamber for even cell distribution before it is counted can help identify some errors.
Counting errors include choosing an inappropriate area to count based on the number of cells present, improper
counting technique, missing cells, counting junk, and misidentifying cells. Manual WBC and platelet counts should
be confirmed with an estimate performed on a Wright's stained peripheral smear.
Manual red counts are inaccurate and imprecise. The hemoglobin and/or hematocrit are usually adequate if a CBC
is not available.
Using manual cell counts for back up is usually more trouble than it is worth. Besides requiring excellent technique,
UNOPETTES® outdate and are expensive. The procedure is time consuming. In a pinch it may be preferable to look
at a well prepared, stained peripheral smear. An increase in white cells, the presence of immature cells, or reactive
lymphocytes may answer the immediate question.
Quality control of manual cell counts is time consuming. At least two levels of controls for all cell types counted
must be counted on every shift and the diluent from the vials must be examined in the hemacytometer to ensure
that there is nothing contaminating the diluent that might be counted as a cell. It is also necessary to do counts on
proficiency samples and to ensure that everyone who is performing counts is getting equivalent results, i.e.,
competency testing.
Hemacytometers are necessary for body fluid counts. Laboratories that examine synovial and other body fluids
may perform cell counts as well as a crystal analysis performed on a polarized microscope.
In summary, if you do not do manual cell counts on blood samples, do not start.
Section Top | Title Page
2. Hematocrits
Kathleen Kelly B.S., MT(ASCP)
When considering back up equipment, the hematocrit centrifuge is probably the most useful. It requires little
expenditure after the initial cost and has simple preventive maintenance and quality control (PM and QC)
requirements.
A centrifuged hematocrit is also called a packed cell volume (PCV). As in the automated hematocrit, a hematocrit is
the volume of the red cells as compared to the volume of the whole blood sample and is reported in L/L or as a %.
The packed cell volume is determined by centrifuging the specimen in capillary tubes and measuring the height of
the red cell column.
The sample is venous blood drawn in EDTA or capillary blood collected in heparinized (red banded)
microhematocrit tubes. A short EDTA sample will have an increased anticoagulant to red cell ratio, which causes
the red cells to shrink and the hematocrit to be falsely decreased. EDTA must not exceed 2 mg/ml of whole blood.
For EDTA samples use blue banded, plain capillary tubes. Traditional tubes are glass and unplugged. Mylar coated
tubes, plastic tubes, and pre-plugged tubes are available. Plastic pre-plugged tubes are a good choice. They
decrease the risk of breaking a tube and puncuturing the finger of the person performing the test and avoid some
sources of error.
To perform a microhematocrit:
1. Fill two red or blue banded capillary tubes, from the end without the colored band, 1/2 to 2/3 full. Tilt each tube
so that the blood is near the colored band. Hold the tube horizontally and wipe all of the excess blood off of the
tubes before it dries. Be careful not to wipe across the end of the tube. Absorbent material will pull out more
plasma than cells.
2. For unplugged tubes, hold each tube horizontally and seal the end with the colored band by inserting it into the
clay.
This is the fire-polished end. Add the sealant until it is just above or below the colored band. Filling
and sealing this way keeps the clay from becoming contaminated with blood, helps prevent leakage, is safer for the
person testing, and keeps the gasket in the centrifuge from being cut by the capillary tubes.
3. Insert the capillary tubes into the centrifuge with duplicate samples across from each other. Place the sealed
end toward the outside, making sure that the tubes are seated in the groves and firmly against the gasket.
4. If there is an internal cover, make sure it is screwed down. The tubes will break if the cover is not on correctly.
Centrifuge the specimens for five minutes at 11,000 to 12,000 rpms.
5. Open the centrifuge after it has come to a complete stop. Read the results immediately after the centrifuge
stops. If this is not possible, place the tubes upright until they are read. The red cells will slide if the tubes are left
in a horizontal position and the hematocrit will be falsely increased.
6. When reading hematocrits, make sure the clay red cell interface is aligned with the 0% line and the bottom of
the plasma meniscus is at the 100% line. The reading that corresponds to the top of the red cell column is the
hematocrit.
7. Duplicate readings should match within 1 L/L and must be within 2 L/L. Readings that match can be averaged
and reported in 0.5 L/L. Centrifuged hematocrits are always reported in whole numbers or halves.
Effect of Error on the
Error
Solution
Decreased
Sample drawn above the IV line
Redraw sample from another site
Decreased
Red cell leakage
Check sealant. Hard sealant causes
Hematocrit
leaks.
Check gasket for cuts.
Do not fill and seal from the same end
of the capillary tube.
Decreased
Short sample, red cells shrink
Perform an automated hematocrit or
redraw the sample.
Decreased/Increased
Mixing errors
Mix sample well before each use.
Increased/Decreased
Reading errors
Check reading device by reading the
hematocrits on a card reader or with a
ruler.
Check employee competence.
Increased
Time too short, timer not
working Inadequate rpms
Increased
Increased
Centrifuge longer, check timer.
Check centrifuge with tachometer.
Sample allowed to stay in the
Remove samples immediately and
centrifuge after it has stopped
store them upright.
Buffy coat included when
Carefully read the top of the red cell
reading the red cell column
column below the layer of white cells
and platelets.
Increased
Abnormal red cell morphology
that results in increased trapped
plasma
Section Top | Title Page
Drawing of a centrifuged Hematocrit
Kathleen Kelly B.S., MT(ASCP)
Perform an automated hematocrit.
Previous Page |
Section Top |
Title Page
Hematocrit Tubes
Kathleen Kelly B.S., MT(ASCP)
Previous Page |
Section Top |
Title Page
Sealing a Hematocrit Tube
Kathleen Kelly B.S., MT(ASCP)
Filling and sealing with the clay perpendicular to the table keeps the clay from becoming contaminated with blood,
helps prevent leakage and is safer. Previous Page |
Section Top |
Title Page
Correctly Aligned Hematocrit Tube
Kathleen Kelly B.S., MT(ASCP)
The 100 % line must bisect the bottom of the meniscus and the zero line must align with the red cell/clay interface.
When both the 0% and 100% lines are positioned correctly, the hematocrit in per cent is the line that aligns with
the top of the red cells. The buffy coat, which is comprised of white cells and platelets, is not included. Previous
Page |
Section Top |
Title Page
a. Hematocrit centrifuge quality assurance
Kathleen Kelly B.S., MT(ASCP)
Quality assurance includes documented quality control and preventive maintenance plus the proficiency and
competency testing. Quality control Good quality control includes running duplicate samples on all patients and
performing at least two levels of commercial controls with known values. If clay is used to plug the tubes, it must
be soft, pliable, and inserted into the end that has not been coated with blood. Duplicate readings must be within
2% and are frequently within 1%.
Everyone performing hematocrits must demonstrate competency. An easy way to do this is to have everyone run
the same sample or a split sample and compare the results. This should include samples with normal and abnormal
hematocrits and be done on a quarterly basis. Quality assurance could also include documenting that multiple
people read the same spun hematocrits and obtained the same results. Proficiency testing samples are available
and may be combined with the proficiency testing done on a hematology multi parameter instrument.
Preventive maintenance
These are generic recommendations. Always check manufacturer's guidelines for specific instructions.
Daily:
Clean the inside of the centrifuge and the gasket.
Monthly:
Check the reading device. Misuse and zeroing of the reading devices can inject large errors. Always use a second,
simple reading device to check the fancier devices. Use a ruler or a flat plastic card.
These cards are
available from laboratory vendors and are inexpensive.
Quarterly:
1. Check the brushes if they are present - this may need to be done more often.
2. Check the gasket for cuts and breaks. Cut gaskets allow tubes to leak and need to be replaced.
3. Check the timer with a stopwatch.
4. Check the speed of the centrifuge with a tachometer. These can easily be shared among multiple laboratories.
5. Perform a maximum cell pack to verify the time required for complete packing.
Centrifuge hematocrits (low, normal, high) for 2 minutes and then repeat the procedure adding 30 seconds each
time you centrifuge until the results are the same for two consecutive centrifugations. The required time is 30
seconds longer than the second time the hematocrit results match.
Example: The required time is 5 minutes.
Time
2 min.
2.5 min.
3 min.
3.5 min.
Result
26%
23%
22%
22%
Result
52%
49%
47%
46%
4 min.
4.5 min.
45%
45%
An easy way to check the maximum pack on a weekly basis is to read a sample and then recentrifuge it for one
minute. The results should be the same. If they are not, perform preventive maintenance on the centrifuge and
redo the maximum pack procedure.
Section Top | Title Page
Micro-Hematocrit Capillary Tube reader
Kathleen Kelly B.S., MT(ASCP)
Previous Page |
Section Top |
Title Page
3. Hemoglobins
Kathleen Kelly B.S., MT(ASCP)
Equipment that only performs hemoglobins is available. One of them is the HemoCue®. This small hand-held
equipment measures the hemoglobin in 10 microliters of blood. It measures azide methemoglobin by mixing
reagents and blood in a small disposable cuvet and measuring at two wavelengths. The higher wavelength
compensates for turbidity so lipemic samples are not a problem.
Stand-alone hemoglobinometers are also available. These are usually based on the same spectophotometric
principle as CBC analyzers and use cyanmethemoglobin as the end point.
With the inexpensive small multi parameter analyzers available, hemoglobin analyzers are no longer popular. The
use of the HemoCue® for back up and lipemic specimens is an exception.
Section Top | Title Page
C. Red Cell and Platelet Indices
Kathleen Kelly B.S., MT(ASCP)
Red cell indices include the mean corpuscular volume (MCV), mean corpuscular hemoglobin (MCH), mean
corpuscular hemoglobin content (MCHC) and red cell distribution width (RDW).
MCV is Mean Corpuscular Volume in femtoliters. On automated instruments, it is computed using the
measurements of each red cell. With manual methods, it is calculated using the hematocrit and the red cell count.
Hint: do not worry about the decimal points. This applies to the MCV, MCH and MCHC. Just divide the raw
numbers and place the decimal where it makes sense. It is a physiologic impossibility to have an MCV of 9.0 or 900.
It must be 90.
Manual
spun hematocrit in L/L
MCV =
-----------------------------red cells in millions/L -->
Automated Hematocrit = RBC x MCV
MCV correlates to the cell diameter on the peripheral smear. Macrocytes have a high MCV
have a low MCV.
average.
and microcytes
It is possible to have abnormal sized cells and a normal MCV because the MCV is an
Agglutinated red cells also cause an increased MCV. These samples need to be warmed in a 370
degrees C heating block and rerun warm.
MVC generic reference range: 82 - 99 femtoliters
MCH is Mean Corpuscular Hemoglobin weight in picograms. This is the average weight of the hemoglobin in
picograms in a red cell. It is a calculated value.
MCH =
hemoglobin in gm/L
-----------------------------red cell count in millions/L
MCH generic reference range: 27 - 32 picograms
MCHC is Mean Corpuscular Hemoglobin Content. This indicates the average weight of hemoglobin as compared to
the cell size. It is traditionally a calculated value. How ever some instruments may measure the density of the cells
as they are counted and use this value to compare to the calculated value. Bayer calls this measured value a CHCM
(Cellular Hemoglobin Concentration Mean) on the Bayer/Technicon hematology instruments.
MCHC
=
Hemoglobin in g/mL
-----------------------------Red cell count in millions/L
or
MCHC
=
MCH in picograms
------------------------------MCV in femtoliters
MCHC correlates with the degree of hemoglobinization of the red cells on the peripheral smear.
It is reported in gm/dL, picograms/100 femtoliter or in %. A decreased MCHC corresponds to cells with increased
zones of central pallor on a Wright's stained peripheral smear. These cells are called hypochromic red cells.
An increased MCHC is rarely a true value. MCHCs above the reference range are suspect. A large number of
spherocytes, the most common physiologic reason, is not common. A more likely reason is an error in the
hemoglobin or the hematocrit. Solutions include: checking the smear for spherocytes, retesting the sample,
performing a spun microhematocrit, performing an alternate hemoglobin method, and checking the quality control
and other patient results to identify shifts or trends in the hemoglobin or hematocrit determinations.
MCHC generic reference range: 32-36 g/dL or pg/fL
RDW is the Red cell Distribution Width. This value indicates the degree of red cell size variation or how much
difference exists between the largest and smallest red cells. This value is derived from the MCV histogram. An
increased RDW corresponds with an increase in anisocytosis on the peripheral smear.
The RDW is only
available if it is included in the instrument menu. Although different manufacturers use slightly different methods
of obtaining data the RDW is generally thought of as the coefficient of variation of red cell volume distribution.
RDW =
standard deviation x100
---------------------mean MCV
RDW generic reference range: 9.0 - 14.5
The RDW, coupled with the MCV, gives more relevant information than an individual index. The following is an
attempt to clarify the relationship of the MCV and RDW.
1.
Red cells that are all microcytic or macrocytic will have a RDW in the reference range and a decreased or an
increased MCV.
2.
Red cells that vary in size and have an average size within the reference range will have an increased RDW
and a normal MCV.
3.
Red cells that vary in size and have an average size below or above the reference range will have an
abnormal MCV and RDW.
There are varying opinions on the clinical value of red cell indices. They are used to morphologically classify
anemias and to select additional tests to determine the cause of an anemia. Indices also change in response to
treatment of some anemias.
Platelet Indices: These include the platelet distribution width and average platelet volume. They have limited use,
but do correlate to flags on the platelet histogram that indicate giant platelet or platelet clumps.
Anisocytosis - variance in red cell size as determined by viewing the diameter of the cells on a stained peripheral
blood smear.
Anemia - A reduction in the oxygen carrying capacity of the blood. Almost always manifested by a decreased
hemoglobin and frequently accompanied by a decreased hematocrit and red cell count.
Section Top | Title Page
Macrocytic Red Cells
Kathleen Kelly B.S., MT(ASCP)
Previous Page |
Section Top |
Title Page
Microcytic Red Cells
Kathleen Kelly B.S., MT(ASCP)
Previous Page |
Section Top |
Title Page
Macrocytic and Microcytic Red Cells
Kathleen Kelly B.S., MT(ASCP)
These red cells vary in size and have an average cell size that falls with in the reference range. Previous Page |
Section Top |
Title Page
Hypochromic Red Cells
Kathleen Kelly B.S., MT(ASCP)
Hypochromic red cells have an increased zone of pallor on Wright's stain. These cells contain decreased
hemoglobin for their size and have a decreased MCHC. Previous Page |
Section Top |
Title Page
Anisocytosis: Variation in Red Cell Size
Kathleen Kelly B.S., MT(ASCP)
These cells exhibit a large variation in size. The RDW (Red Cell Distribution width) is a numerical indication of this
morphologic abnormality. Previous Page |
Section Top |
Title Page
Hematology in the Physician Office Laboratory Section I
Practice Test (No Cost) | CME Credit Test (20 module Course Registration =
$425.00)
Evaluation Form
Copyright © 2008 University of Iowa. All rights reserved.
Comments or questions about our Web site? Contact the Webmaster.