problem 65- diarrhoea
advertisement
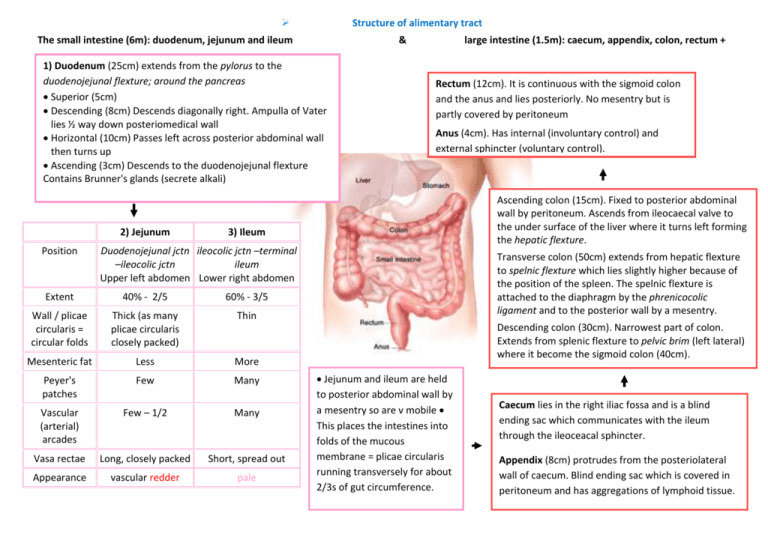
Structure of alimentary tract
The small intestine (6m): duodenum, jejunum and ileum
&
1) Duodenum (25cm) extends from the pylorus to the
duodenojejunal flexture; around the pancreas
Superior (5cm)
Descending (8cm) Descends diagonally right. Ampulla of Vater
lies ½ way down posteriomedical wall
Horizontal (10cm) Passes left across posterior abdominal wall
then turns up
Ascending (3cm) Descends to the duodenojejunal flexture
Contains Brunner's glands (secrete alkali)
2) Jejunum
Position
large intestine (1.5m): caecum, appendix, colon, rectum +
anal canal.
Rectum (12cm). It is continuous with the sigmoid colon
and the anus and lies posteriorly. No mesentry but is
partly covered by peritoneum
Anus (4cm). Has internal (involuntary control) and
external sphincter (voluntary control).
Ascending colon (15cm). Fixed to posterior abdominal
wall by peritoneum. Ascends from ileocaecal valve to
the under surface of the liver where it turns left forming
the hepatic flexture.
3) Ileum
Duodenojejunal jctn ileocolic jctn –terminal
–ileocolic jctn
ileum
Upper left abdomen Lower right abdomen
Extent
40% - 2/5
60% - 3/5
Wall / plicae
circularis =
circular folds
Thick (as many
plicae circularis
closely packed)
Thin
Mesenteric fat
Less
More
Peyer's
patches
Few
Many
Vascular
(arterial)
arcades
Few – 1/2
Many
Vasa rectae
Long, closely packed
Short, spread out
Appearance
vascular redder
pale
Transverse colon (50cm) extends from hepatic flexture
to spelnic flexture which lies slightly higher because of
the position of the spleen. The spelnic flexture is
attached to the diaphragm by the phrenicocolic
ligament and to the posterior wall by a mesentry.
Descending colon (30cm). Narrowest part of colon.
Extends from splenic flexture to pelvic brim (left lateral)
where it become the sigmoid colon (40cm).
Jejunum and ileum are held
to posterior abdominal wall by
a mesentry so are v mobile
This places the intestines into
folds of the mucous
membrane = plicae circularis
running transversely for about
2/3s of gut circumference.
Caecum lies in the right iliac fossa and is a blind
ending sac which communicates with the ileum
through the ileoceacal sphincter.
Appendix (8cm) protrudes from the posteriolateral
wall of caecum. Blind ending sac which is covered in
peritoneum and has aggregations of lymphoid tissue.
Functions of alimentary tract (e.g. motility, fluid and electrolyte balance, absorption, immunity)
The small intestine
-
Secretes digestive enzymes for digestion, and absorbs water
1. Duodenum
-
Receives bile from the gall bladder (via common bile duct) and pancreatic juice and digestive enzymes are
activated here
-
Its wall contains various glands e.g. Brunner’s glands, that secrete alkaline juice, rich in mucus, that
protects the duodenum from the effects of the acidic chime coming from the stomach
2. Jejunum
-
It contains muscles to help move the food along and aid digestion
-
Villi and microvilli ↑ SA available to absorb nutrients
-
It has many large circular folds in its submucosa called plicae circulares to ↑ SA
-
Across epithelial cells: passive transport of sugar fructose and the active transport of amino acids,
small peptides, vitamins, and most glucose.
3. Ileum
-
Absorption of Vitamin B12, bile salts and remaining products of digestion
-
Villi + micro villi to ↑ SA for absorption and adsorption (attachment) of enzyme molecules and for
the absorption of products of digestion
-
Villi contain many capillaries: take A.As and glucose to the hepatic portal vein and the liver, and
lacteals: small lymph vessels that absorb fatty acid and glycerol
-
Secretes protease and carbohydrase enzymes (gastrin, secretin, cholecystokinin) responsible for
the final stages of protein and carbohydrate digestion.
-
Layers of circular and longitudinal smooth muscle enable the digested food to be pushed along the
ileum by waves of muscle contractions called peristalsis.
-
Contains payer’s patches: which contain macrophages, dendritic cells, B-lymphocytes, and Tlymphocytes etc
Large intestine
-
Mainly responsible for storing waste, reclaiming water, maintaining the water balance, and
absorbing some vitamins, such as vitamin K.
1. Caecum
2. Colon
-
Some electrolytes like sodium, magnesium, and chloride are left as well as indigestible
carbohydrates known as dietary fiber
-
Most of the remaining water is removed
-
Chyme is mixed with mucus and bacteria known as gut flora, and becomes faeces
-
The bacteria break down some of the fiber for their own nourishment and create waste products
the cell lining of the colon uses for nourishment
-
The large intestine produces no digestive enzymes — chemical digestion is completed in the small
intestine before the chyme reaches the large intestine.
3. Rectum
-
A temporary storage facility for feces
-
When rectal walls expand stretch receptors from the ANS stimulate the desire to defecate.
-
Intrarectal pressure forces the walls of the anal canal apart allowing the faeces to enter the canal.
The rectum shortens and peristaltic waves propel the feces out of the rectum.
-
The internal and external sphincter allow the feces to be passed by muscles pulling the anus up
over the exiting feces.
Fluid:
Where do fluid volumes come from:
– 1200ml ingested per day (along with 800g food)
– 7000ml fluid from salivary glands, gastric glands, pancreas, liver and intestinal glands.
Water most abundant substance in chyme
Approx. 8000ml ingested and secreted water enters the small intestine each day, but only
1500ml passes onto the large intestine.
80% absorbed in the small intestine into the blood – here osmotic potential created by the
active absorption of solutes, mostly salts (ions) known as electrolytes.
100ml fluid lost in faeces – represents only 4% of total daily fluid loss. Most lost via the
kidneys in urine, and the respiratory system in expiratory air due to the moist lung lining.
Electrolytes:
Sodium ions account for much absorption because most abundant solute in chime - Active
transport occurs using Na+/K+ -ATPase pumps.
Other minerals in smaller concentrations include potassium, magnesium, and calcium.
Trace elements include iron, zinc and iodide.
Na+/K+ -ATPase pump:
1. Transporter protein, with associated ATP molecule, binds 3 sodium ions at high-affinity sites
on the intra-cellular protein surface.
2. Phosphorylation of intracellular surface of protein through the action of ATPase catalysing
ATP → ADP + phosphorous.
3. Phosphorylation initiates conformational change in protein, releasing sodium ions into the
extra cellular fluid.
4. New conformation results in increase affinity of the 2 binding sites for potassium.
5. Potassium binds causing dephosphorylation, returning the protein pump to its original form.
6. Potassium ions released into intracellular fluid, allowing the process to start again.
Motility
GI smooth muscle is inherently active. The ‘gastric pacemaker’ is on the greater curvature, the
interstitial cells of Cajal)
- Parasympathetic: Acetylcholine (stimulated by gastrin)
- Sympathetic: Adrenaline (inhibited by dopamine / opiates)
3 types of movement:
1) Peristalsis = coordinated action to move food from one portion of the GI tract to another,
in the direction of mouth→anus
2) Mass movement = the intense contraction beginning ½ way along the transverse colon that
pushes intestinal contents towards the rectum – only occurs a few times a day and is
responsible for colonic evacuation
3) Segmentation = alternate contraction and relaxation along the GI tract to mix food, with no
forward movement
Even without food in the lumen, there is a continuous muscle contraction sequence, the MMC
‘migrating motor complex’, which is initated in the antrum, and has 4 phases.
-
This removes indigestible particles
Prevents bacterial growth
Microbiology of alimentary tract
Mouth -
-
200+ species of oral bacteria: Streptococci, lactobacilli, staphylococci and
corynebacteria. Streptococcus salivarius (up to 98%)
Eruption of the teeth : colonization by S. mutans and S. sanguis.
The onset of puberty : colonization by Bacteroides and spirochetes.
Plaque = build-up of material on the teeth, and 60% of this material is microbial
e.g. S. mutans and S. sanguis.
Gingivitis : caused by increased populations of Actinomyces and other anaerobes
Stomach
Helicobacter pylori (up to 50%)
In the stomach ↑ acidity kills all but the most acid-tolerant (mainly streptococci)
Small
intestine
Lactics, enterics, enterococci, bifidobacteria
Microbial populations are much higher in the proximal end of the small intestine
than in the stomach, but are still relatively sparse vs the colon
Gram-positive bacteria (mainly lactobacilli + Enterococcus faecalis), enteric rods
and Bacteroides colonize the small intestine
synthesize vitamins K and B complex
metabolize some compounds that we cannot
can metabolize compounds to produce damaging products e.g. carcinogens +
are opportunistic pathogens e.g. if damage to the intestinal wall.
Colon
Bacteroides, lactics, enterics, enterococci, clostridia, methanogens
Same sorts of species as rest of GI tract but many more in numbersIncl. enteric
rods, streptococci, clostridia and lactobacilli.
The predominant species by far are the strictly anaerobic e.g. bacteroides fragilis
Intestinal flora facilitate: conjugated bilirubin → urobiligen, + remaining urobiligen
→ stercobiligen
If Pts on a broad spectrum antibiotic commensals are killed allowing gut infections
e.g C. Dif
Able to perform examination of alimentary system
Able to perform rectal examination
See clinical examination handbook
Able to explain to family issues relating to hygiene (e.g. infant feeding, food preparation)
The Foods Standards Agency in the UK has identified the '4 Cs' to help prevent food poisoning,
including food poisoning caused by Salmonella:
Cleanliness
Keep work surfaces and utensils clean.
Wash and dry your hands regularly but especially after going to the toilet, before preparing
food, after handling raw food, after touching pets, after gardening, and before touching
'ready-to-eat' food.
Don't prepare food for others if you have diarrhoea or vomiting.
Cover any sores or cuts on your hands with a waterproof plaster before you touch food.
Change dishcloths and tea towels regularly.
You should also wash your hands after touching pets or animals, after visiting farms and after
gardening to help avoid infection.
Cooking
Make sure that you cook food thoroughly, especially meat. This will kill bacteria. Food should
be cooked right through and be piping hot in the middle.
If you are reheating food, it needs to be cooked right through and be piping hot in the middle.
Don't reheat food more than once.
You should also wash raw fruits and vegetables before you eat them.
Don't drink water thought to be unsafe (including avoiding drinks containing ice cubes that
may have been made from unsafe water). This includes untreated water from rivers, lakes and
streams.
Drink pasteurised or boiled milk and avoid raw eggs.
Chilling
Food that needs to be chilled or refrigerated should be. If food is left out of the fridge,
bacteria may multiply to levels that can cause food poisoning.
Your fridge needs to be kept between 0°C and 5°C. Don't leave the door open.
Cool leftover food quickly and then refrigerate. Taking it out of the cooking pot and putting it
into a shallow container can speed the cooling process up.
Cross-contamination
Wash your hands after touching raw foods.
Separate raw and cooked or 'ready-to-eat' foods.
Keep raw meat in a sealable container at the bottom of the fridge.
Don't use the same surface or chopping board for preparing raw and ready-to-eat foods.
Make sure that knives and utensils are cleaned after preparing raw foods.
In addition to these measures, as reptiles and amphibians including terrapins and tortoises
can commonly carry bacteria, you should not keep them in a house where children under the
age of one year live, or where someone with a weakened immune system also lives.
Able to institute methods to reduce risk of spread of diarrhoea
In addition to the above
If your baby has diarrhoea, be especially careful to wash your hands after changing nappies and
before preparing, serving, or eating food.
For older children/adults, whilst they have diarrhoea, the following are recommended:
Regularly clean the toilets used with disinfectant. Also, clean the flush handle, toilet seat, sink
taps, bathroom surfaces and door handles at least daily with hot water and detergent. Disposable
cleaning cloths should be used (or a cloth just for toilet use).
If a potty has to be used, wear gloves when you handle it, dispose of the contents into a toilet,
then wash the potty with hot water and detergent and leave it to dry.
If clothing or bedding is soiled, first remove any faeces into the toilet. Then wash in a separate
wash at as high a temperature as possible.
Don't share towels and flannels.
Don't prepare food for others.
Stay off school/nursery, work/college etc, until at least 48 hours after the last episode of diarrhoea
or vomiting. Sometimes this time may be longer with certain infections.
If the cause of diarrhoea is known to be (or suspected to be) Cryptosporidium, one should not
swim in swimming pools for two weeks after the last episode of diarrhoea.
Take extra measures when in countries of poor sanitation. E.g. avoid tap water, avoid food washed
in unsafe water.
Breast-fed babies are less likely to develop infectious diarrhoea compared to bottle-fed babies.
Role of carriers of disease
A 'carrier' is a person who is well, has no symptoms, but is infected with a bacterium.
Carriers are at risk of passing on the infection to others if their personal hygiene is not good.
C. difficile lives harmlessly in the gut of many people (~3/100 adults, 7/10 babies)
The vast majority of people with a salmonella infection clear the infection and bacteria
completely from their body soon after symptoms ease. Rarely, on recovery from a salmonella
illness, some people become carriers and continue to pass out salmonella bacteria in their
faeces for weeks or months. This is more common in children. A small number of children
aged less than five years pass out salmonella bacteria for up to a year. Over the age of five
years, salmonella carriers are rare, and the maximum duration of shedding appears to be up
to 12 weeks.
(Note: this is different to people with typhoid or paratyphoid. A small number of people who
recover from these diseases remain carriers for life.)
Able to take a focussed history from patient or parent regarding diarrhoea
HPC
-
What does the patient mean by diarrhoea?
What is the normal bowel habit
Duration and severity of diarrhoea
Frequency and timing of bowel movements
Presence of blood, mucus
Changes in colour or consistency - evidence of steatorrhea
Circumstances of onset (including recent travel, food ingested (meat, poultry, dairy,
shellfish), source of water)
Triggers
Does anything relieve it / Have you tried any treatments
Associated symptoms
- Constipation
- Abdominal pain or vomiting
- Rectal bleeding
- Mouth ulcers
- Other upper GI symptoms
- Associated changes in weight or appetite
- Rectal urgency or tenesmus
- Altered size of stools passed
- Systemic symptoms – malaise, lethargy, fever, night sweats, weight loss, anorexia
- Simultaneous occurrence of diarrhoea in close contacts should be ascertained
- Signs of thyrotoxicosis
PMH
-
Recent admittance to hospital
Recent surgery to bowel
Hyperthyroidism, Diabetes mellitus, Hypoparathyroidism, Addison's disease
DH
-
-
Any antibiotics within the previous 3 months - is it C. Dif? – is it an antibiotic reaction e.g.
erythromycin?
Mg containing drugs, NSAIDs, theophyllines, anti-arrhytmics, anti-neoplastic agents – all
can cause diarrhoea
On laxatives?!
-
Are close contacts well?
History of coeliacs, inflammatory bowel disease
Autoimmune disorders / endocrine disorders
-
Recent travel abroad
High alcohol intake
Food additives such as sorbitol and fructose
-
FH
SH
Able to take a dietary history
Adult / child
1. Have you experienced any change in weight?
2. How many meals and snacks do you eat in at 24 hour period?
3. How many times a week do you eat the following meals away from home?
Breakfast ______ Lunch ______ Dinner ______
4. What types of eating places do you frequently visit?
Fast-food ______ Diner/cafeteria ______ Restaurant ______ Other ______
5. On average, how many pieces of fruit or glasses of juice do you eat or drink each day?
Fresh fruit ______ Juice (8 oz cup) ______
6. On average, how many servings of vegetables do you eat each day?
7. On average, how many times a week do you eat a high-fiber breakfast cereal?
8. How many times a week do you eat red meat (beef, lamb, veal) or pork?
9. How many times a week do you eat chicken or turkey?
10. How many times a week do you eat fish or shellfish?
11. How many hours of television do you watch every day?
12. Do you usually snack while watching television?
13. How often do you usually consume dairy products, and what type?
14. How many times a week do you eat desserts and sweets?
15. What types of beverages do you usually drink? How many servings per day?
Water ____ Juice ______ Soda ____ Diet soda ____ Sports drinks ______ hot drinks +/- sugar
_____ Milk (whole, semi-skimmed, skimmed)______Alcohol (Beer, Wine, spirits) ______
Infant
o
Is the baby bottle or breast fed?
If breast fed
o What is the duration of exclusive breast feeding?
o Was this a satisfying experience for mother and baby?
o How often did she feed?
o Was the infant content? Were there any problems?
o How did he sleep, feed and gain?
o Did she feed on demand or to some sort of schedule?
o Was she complementing the breast milk with anything else?
If bottle fed
o Was he fed on formula or unmodified cow’s milk?
o Which formula did he receive? How was it prepared?
o What volume did he take each feed and how long did he take over it?
o Frequency of feeds?
o Total daily intake? Any additives (iron or vitamins) given with milk?
o Duration of exclusive milk feeding?
Determinants of nutritional status
Nutritional status = The condition of health of a person that is influenced by the intake and
utilisation of nutrients. Malnutrition covers both the states of undernutrition and overnutrition.
Causes
Decreased availability of food due to:
- Increased in population / Low
production / stocks
Decreased absorption of foods e.g.
coeliacs
Poor education
Economic conditions
Stress conditions (increased
nutritional need)
Poor personal hygiene and
environmental sanitation
-
Outcome
Lowered food intake
-
Lowered intake of foods / nutrients
-
Wrong feeding practices
Inability to make correct choice of food resulting in
over/under-nutrition
Lowered purchasing power causing undernutrition
Higher purchasing power causing overnutrition
Inability to meet the increased nutrient needs during
periods of rapid physical growth e.g. in young
children, adolescents, pregnant women, lactating
mothers
Inability to meet increased demands of illness
Increased susceptibility to infections and thereby
illnesses
-
-
Able to prepare patient for imaging and endoscopic procedures
Colonoscopy
What is colonoscopy?
A colonoscopy is a test where an operator (a doctor or nurse) looks into your colon (large
intestine/bowel).
A colonoscope is a thin, flexible, telescope. It is about as thick as a little finger. It is passed
through the anus and into the colon. The colonoscope contains fibre optic channels which
allow light to shine down so the operator can see inside your colon.
The colonoscope also has a 'side channel' down which devices can pass. These can be
manipulated by the operator. For example, the operator may take a small sample (biopsy)
from the inside lining of the colon by using a thin 'grabbing' instrument which is passed down
a side channel
The procedure
Colonoscopy is usually done as an outpatient or day case.
You will usually be given a sedative to help you to relax. This is usually given by an injection
into a vein in the back of your hand. This makes you drowsy but it is not a general anaesthetic.
You will be asked to wear a gown, and lie on your side on a couch. The operator will gently
push the colonoscope into your anus and up into the colon. This can be a little uncomfortable.
The operator can look down the colonoscope and inspect the lining of the colon. Modern
colonoscopes transmit pictures through onto a TV monitor for the operator to look at.
Air is passed down a channel in the colonoscope into the colon to make the inside lining easier
to see. This may cause you to feel as if you want to go to the toilet. The air may also make you
feel bloated, cause some mild 'wind pains', and may cause you to pass wind. This is normal
and there is no need to be embarrassed, as the operator will expect this to happen.
The operator may take biopsies (small samples) of some parts of the inside lining of the colon.
This is painless. It is also possible to remove polyps (small lumps of tissue which hang from the
inside lining of the colon.) At the end of the procedure the colonoscope is gently pulled out.
A colonoscopy usually takes about 20-30 minutes. However, you should allow at least 2 hours
for the whole appointment.
What preparation do I need to do?
The colon needs to be empty so that the operator can get a clear view. You will be instructed
on how to take a special diet for a few days before the test. You will also be given some
laxatives to take.
You will need somebody to accompany you home, as you will be drowsy with the sedative.
Side effects
The sedative may cause you to feel tired or sleepy for several hours afterwards.
You may pass some blood from your anus if a biopsy was taken, or a polyp removed.
Occasionally, the colonoscope may cause damage to the colon. This may cause bleeding,
infection and, rarely, perforation.
If any of the following occur <48 hours after a colonoscopy, consult a doctor immediately:
× Abdominal pain. (In particular if it becomes gradually worse, and is different or more
intense to any 'usual' pains that you may have.)
× Fever (raised temperature).
× Passing a lot of blood from your anus.
Sigmoidoscopy
What is sigmoidoscopy?
The sigmoid colon is the final portion of the bowel that is joined to the rectum.
A sigmoidoscope is a small tube with an attached light source about the thickness of your
finger. A doctor or nurse inserts the sigmoidoscope into the anus and pushes it slowly into the
rectum and sigmoid colon. This allows the doctor or nurse to see the lining of the rectum and
sigmoid colon.
The procedure is not usually painful but it may be a little uncomfortable.
The flexible sigmoidscope allows your doctor to see around bends in the colon and usually
makes the examination more comfortable.
The rigid sigmoidoscope allows your doctor to look into the rectum and the bottom part of
the colon, but it does not reach as far into the colon as the flexible sigmoidoscope.
What preparation do I need to do?
The colon needs to be empty so that the operator can get a clear view. This is usually by
taking powerful laxatives for a day or two, or by using one or two enemas prior to the
procedure. A commonly used laxative to clear the bowel is called Picolax.
The procedure
This test takes just a few minutes. Usually you do not need an anaesthetic or sedation.
You wear a hospital gown so that the lower half of your body is exposed. You will be asked to
lie on your left side with your knees drawn up toward your chest.
First the doctor or nurse will gently insert a gloved and lubricated finger (or fingers) into the
rectum to check for blockage and to widen the anus. Then the sigmoidoscope will be inserted
and gently pushed further into the rectum and colon.
Air is gently pumped through the sigmoidoscope to help viewing. This can cause you to feel
bloated and uncomfortable, and give you an urge to defecate ('move your bowels'). As the
sigmoidoscope is slowly removed, the lining of the bowel is carefully examined.
A small sample (biopsy) of bowel lining may be taken during the procedure. The sample is sent
to the laboratory to be looked at under the microscope. It may also be tested for various
conditions that can affect the bowel.
Side-effects
Some people have some crampy pains and excess wind after the procedure.
Occasionally, the sigmoidoscope causes some damage to the rectum or colon. This may cause
bleeding, infection and, rarely, perforation of the colon.
If any of the following occur within 48 hours after a sigmoidoscopy, consult a doctor immediately:
× Severe abdominal pain.
× Bloody bowel movements or rectal bleeding.
× Fever.
Barium enema
What is a barium enema?
A barium enema is used to look for problems in the colon, such as polyps, inflammation
(colitis), narrowing of the colon, tumours, diverticula, etc.
The gut does not show up very well on ordinary X-ray pictures. However, if a liquid that
contains barium is placed in the gut, the outline of the intestines (gut) shows up clearly on Xray pictures. This is because X-rays do not pass through barium. A thick white liquid that
contains barium is used as an enema to place in the colon (lower gut)
The procedure
You will be asked to wear a gown and to lie on a couch on your side or front. A small tube is
then put into your anus (back passage) and gently pushed up a few centimetres. Barium liquid
is then passed through the tube into your colon.
The aim is to get the barium liquid to spread all along the colon as far as the caecum (where
the small intestine joins the colon). To help with this, the person doing the test may:
Ask you to move into different positions to help with the flow of the barium liquid.
Give you an injection of a drug that makes the muscles in the wall of the colon relax.
Pass some air down the enema tube into the colon. (This may feel a little uncomfortable like 'trapped wind'.)
When the barium has spread throughout the colon, several X-ray pictures are taken with
you in different positions. The aim is to have pictures of all parts of the colon. (Low-dose
X-rays are used so the total amount of radiation is quite small and thought to be safe.)
The tube is then removed and you can go to the toilet. The test takes 15-20 minutes.
What preparation do I need to do?
The preparation aims to clear out any faeces (stools) from your colon before the test. So, you
should be given some strong laxatives.
You should also be advised on the kind of food to eat for a day or so before the test.
You will usually be advised to carry on with your normal medication, except iron tablets.
You will need to arrange travel home as you may not be able to drive safely*
Are there any side-effects or risks from a barium enema?
The barium does not get absorbed into the body!
Some people feel a little sickly or have stomach cramps for a few hours afterwards.
The barium may make you constipated. So, to help prevent constipation:
o Have lots to drink for a day or so to flush the barium out of your gut.
o Eat plenty of fruit for a day or so.
o See your doctor if you haven't passed any faeces (stools) after three or four days.
The barium will make your faeces white or pale until it has all passed out from your colon
(after a day or so).
If you had an injection to relax the muscles in your colon, it may cause some blurring of your
vision for an hour or so. If this happens it is best not to drive until this passes*
Rarely it can cause perforation of the colon (making a small hole in the wall of the colon). This
is generally only a risk if you have a badly inflamed colon.
Rarely a person may have a reaction to the injection of muscle relaxant mentioned above.
DIARRHOEA
= Diarrhoea means 'loose or watery stools (faeces), usually at least three times in 24 hours' – can
be defined as the passage of more than 300 g of stool per day. Often there is an increase in the
frequency of defaecation and a loosening of the consistency.
Global impact on infant mortality
Diarrhoeal disease is the second leading cause of death (16%) in children under five years old.
It is both preventable and treatable.
Diarrhoeal disease kills 1.5 million children every year.
Globally, there are about two billion cases of diarrhoeal disease every year.
>50% of these are in Africa and South Asia
Diarrhoeal disease mainly affects children under two years old.
Diarrhoea is a leading cause of malnutrition in children under five years old.
Able to detect features of dehydration in infancy and childhood
Feature
Consciousness
Cap refill
Alert
2 sec
Moderate (610%)
Lethargic
2-4 sec
Mucous
membranes
Tears
Normal
Dry
Normal
↓
Passing little urine
Sunken eyes
Weakness
Being irritable or lethargic
Tachycardia
Mild (<5%)
Severe (>10%)
Obtunded
>4 seconds +
cool limbs
Parched,
cracked
Absent
Hypotension
Fast (but often shallow) breathing
Pale or mottled skin
Altered skin turgor
Cold hands or feet
Able to maintain fluid balance change (e.g. in children with acute diarrhoea)
Able to commence and monitor rehydration therapy particularly in children
When to start a fluid chart
1) Actual or potential dehydration
o Nil by mouth
5) Actual or potential acute illness
o Diarrhoea
o Risk of level 2 or 3 care
o Excessive vomiting
o Sepsis
o Excessive surgical loss
o EWS triggered/patient unstable
o Excessive wound exudate
2) Commencing IV fluid
3) Routine post op management
4) Doubt over fluid status
6) Fluid restriction
o Unstable cardiac failure
o Liver failure
o Acute renal failure
Daily maintenance
0-10 kg : 100ml/kg
10-20kg : 50ml/kg
20+kg : 20ml/kg
→ divide by 24 to get mls/hr
Estimate of weight
(Age + 4) x 2 = kg
Rehydration for deficit
Kg x est % deficit x 10 = ml
Which fluids?
Need: Na, K, dextrose
<6 months – 10% dextrose + electrolytes
Other children – 5% d.extrose + electrolytes
MATINTENANCE = 0.45% NaCl + 10% dextrose
BOLUS = 0.9% NaCl (normal saline)
Able to explain use of oral rehydration therapy
Oral rehydration therapy
o
Principally this involves giving the dehydrated individual glucose and sodium (salt).
1) WHO ORS (sodium chloride 3.5g, sodium citrate 2.9g, potassium chloride 1.5g and glucose in
one litre).
2) Dioralyte
Ingredients: Na+, K+, Cl-, citrate and glucose
Dose: 200-400ml solution after every loose motion
- Infant: 1-1 1/2 times usual feed volume
- Child: 200ml after every loose motion
Instructions:
Sachets: make up one sachet with 200 ml of water, freshly boiled and cooled for infants
Effervescent tablets: 2 tablets in 200 ml of water, only for adults and for children over 1 year
Fluids to prevent dehydration
Encourage plenty of fluids.
Breast or bottle feeds should be encouraged as normal.
ADULTS - As a rough guide, drink at least an extra 200 mls after each bout of diarrhoea (after
each watery stool).
Rehydration drinks are recommended for people who are frail, or over the age of 60, or who
have underlying health problems: salts, sugar and water
Do not use home-made salt/sugar drinks, as the quantity of salt and sugar has to be exact.
Avoid fruit juices or fizzy drinks as these can make diarrhoea worse.
In conditions where the sterility of bottles and teats is in question, the fluid should be given
via a cup and spoon.
Sometimes a child may need to be admitted to hospital for treatment if they are dehydrated:
Treatment in hospital usually involves rehydration solution via a special tube called a
'nasogastric tube'. This tube passes through the nose, down the throat and into the stomach.
An alternative treatment is with intravenous fluids (fluids given directly into a vein).
Eat as normally as possible once any dehydration has been treated + keep drinking
Do not 'starve' a child with diarrhoea this is now known to be wrong.
Breast-fed babies should continue to be breast-fed if they will take it. This will usually be in
addition to extra rehydration drinks.
Bottle-fed babies should be fed with their normal full-strength feeds if they will take it. Again,
this will usually be in addition to extra rehydration drinks.
Older children/adults – small light meals when ready
If you do feel like eating, avoid fatty, spicy or heavy food at first.
Plain foods such as wholemeal bread and rice are good foods to try eating first.
Medication (usually needed)
You should not give medicines to stop diarrhoea to children under 12 years old.
You can give paracetamol or ibuprofen to ease a high temperature or headache.
ADULTS may take loperamide to decrease number of diarrhoeal episodes for up to 5 days
Initiates appropriate investigations (e.g. stool exam and culture; imaging; endoscopy; serum
electrolytes; tests for malabsorption)
Able to interpret basic investigations
Key Investigations to consider include:
●
digital rectal examination, to exclude overflow diarrhoea due to constipation and a low rectal
carcinoma
●
blood tests include:
o full blood count, ESR
o creatinine and electrolytes, glucose
o C reactive protein
o clotting screen
o B12 and folate
o TIBC
o thyroxine
o immunoglobulins
o fasting gut hormones - if other tests negative
●
Radiology:
o especially important when the abdomen is distended or tender
o a plain abdominal film may reveal fluid levels, gas- filled loops or loss of gas in parts
where the loops are inflamed
o barium enema
●
sigmoidoscopy +/- biopsy
●
colonoscopy +/- biopsy
●
stool microbiology, including microscopy, culture and antibiotic sensitivity determination
●
stool for faecal fat estimation to exclude steatorrhoea
Disorders of fluid/ electrolyte balance
Condition
Definition
Hyponatraemia
Serum Na < 136
mEq/L caused by an
excess of water
relative to solute.
Aetiology
Common
causes
include diuretic use,
diarrhea,
heart
failure, and renal
disease.
Clinical
features
Primarily neurologic
(due to an osmotic
shift of water into
brain cells causing
oedema): headache,
confusion,
seizures
and coma.
Serum Na. Serum and urine electrolytes and
osmolality help determine the cause.
Restricting water
Controlled water
intake and promoting replacement. If poor
its loss, replacing any response, testing (e.g.
Na deficit, and
monitored water
treating the cause.
deprivation or
vasopressin) to detect
other causes
Tests
Treatment
Hypernatremia
Hypokalaemia
Hypernatraemia
is Serum K < 3.5 mEq/L
serum Na > 145 mEq/L. (deficit in total body K
stores or abnormal
movement of K into
cells)
It implies a deficit of
Excess losses from
total body water
kidneys or GI tract e.g.
relative to total body
chornic diarrhoea,
Na, caused by water
vomiting, protracted
intake being less than
gastric suction, clay
water losses.
(bentonite) ingestion
(binds to K), villous
adenoma of the colon
Thirst; neurologic (due Muscle weakness and
to an osmotic shift of polyuria; cardiac
water out of brain hyperexcitability may
cells):
confusion, occur with severe
seizures, coma neuro- hypokalemia.
muscular excitability
Serum K
measurement.
Giving K and
managing the cause.
Hyperkalaemia
Serum K > 5.5 mEq/L
(excess total body K
stores or abnormal
movement of K out of
cells)
Increased K intake,
drugs that impair renal
K excretion, and acute
or chronic kidney
disease. It can also
occur in metabolic
acidosis as in diabetic
ketoacidosis.
Neuromuscular: muscle
weakness and cardiac
toxicity
Hypocalcaemia
Hypocalcemia is total
serum Ca < 8.8 mg/dL &
normal plasma protein
conc.s OR serum ionized
Ca < 4.7 mg/dL
Causes include
hypoparathyroidism,
vitamin D deficiency, and
renal disease.
Serum K, and ECG.
Serum Ca with adjustment
for serum albumin.
Treatment is
administration of Ca,
sometimes with vitamin D.
Decreasing K intake,
adjusting drugs, giving
a cation exchange resin
and, in emergencies, Ca
gluconate, insulin, and
dialysis.
Manifestations include
paresthesias, tetany, and,
when severe, seizures,
encephalopathy, and
heart failure.
Condition
Definition
Aetiology
Clinical
features
Tests
Treatment
Hypercalcaemia
Hypercalcemia is total
serum Ca
concentration > 10.4
mg/dL or ionized
serum Ca > 5.2 mg/dL.
Hyperparathyroidism,
vitamin D toxicity, and
cancer.
Hypophosphatemia
Serum phosphate
(PO4) < 2.5 mg/dL
Alcoholism,
starvation,
diuretic use.
Hyperphosphatemia
Hypomagnesemia
Serum phosphate (PO4) Serum Mg < 1.4
> 4.5 mg/dL
mEq/L (< 0.70
mmol/L).
burns, Chronic renal failure,
and
hypoparathyroidism,
and metabolic or
respiratory acidosis.
Hypermagnesemia
Serum Mg > 2.1 mEq/L (>
1.05 mmol/L).
Inadequate Mg intake The major cause is renal
and absorption or
failure.
increased excretion
due to hypercalcemia
or drugs such as
furosemide.
Polyuria, constipation, Muscle
weakness, Features may be due to Features due to
Symptoms include
muscle weakness,
respiratory
failure, accompanying
accompanying
hypotension, respiratory
confusion, and coma. and heart failure; hypocalcemia
e.g. hypokalemia and
depression, and cardiac
seizures and coma can tetany.
hypocalcemia:
arrest.
occur.
lethargy, tremor,
tetany, seizures, and
arrhythmias.
Serum ionized Ca and
Serum PO4 concentration.
Diagnosis is by serum Mg concentration.
parathyroid hormone.
Increase Ca excretion PO supplementation. Restriction of PO
Mg replacement.
IV administration of Ca
4
4
and reduce bone
gluconate and possibly
intake and
resorption of Ca
administration of PO4furosemide; hemodialysis
involves saline, Na
binding antacids, such
can be helpful in severe
diuresis, and drugs
as Ca carbonate.
cases.
such as pamidronate.
Able to classify type of diarrhoea
Anatomically
Colonic:
o Diverticular disease
o Colonic neoplasia
o
o
Ischaemic colitis
Overflow diarrhea secondary to
constipatoin
Ulcerative colitis and Crohn's
colitis
o Infective colitis
Small bowel:
o Coeliac disease
o Crohn's disease
o Terminal ileitis e.g. TB
o Other small bowel
enteropathies (e.g. Whipple's
disease, tropical sprue,
amyloid, intestinal
lymphangiectasia)
o Bile acid malabsorption
o Disaccharidase deficiency
o Small bowel bacterial
overgrowth
o Mesenteric ischaemia
o Radiation enteritis
o Lymphoma
Pancreatic:
o Chronic pancreatitis
o Pancreatic carcinoma
o Cystic fibrosis
o
By aetiology
Viral e.g. rotavirus, adenovirus
Bacterial food poisoningCampylobacter, Salmonella
and Escherichia coli.
o Recent antibiotic therapy and
Clostridium difficile infection.
Previous surgery:
o Extensive resections of the
ileum and right colon lead to
diarrhoea
o Bacterial overgrowth,
particularly in bypass
operations such as in gastric
surgery and jejunoileal bypass
procedures for morbid obesity
o Shorter resections of the
terminal ileum can lead to bile
acid diarrhoea that typically
occurs after meals and usually
responds to fasting and
cholestyramine
o Chronic diarrhoea may also
occur in up to 10% patients
after cholecystectomy
Drugs:
o Up to 4% of cases
o Particularly magnesiumcontaining products,
antihypertensive and nonsteroidal anti-inflammatory
drugs, theophyllines,
antibiotics, anti-arrhythmics,
and anti-neoplastic agents
o Also food additives such as
sorbitol and fructose
Other non-infective
o Alcohol: diarrhoea is common
in alcohol abuse.
o Anxiety
o Immunodeficiency.
o Autonomic neuropathy.
o Factitious diarrhoea
o Irritable bowel syndrome.
o
o
Endocrine:
o Hyperthyroidism
o Diabetes mellitus
o Hypoparathyroidism
o Addison's disease
o Hormone secreting tumours
(VIPoma, gastrinoma, carcinoid)
Infective
o Chronic infection, e.g.
amoebiasis, giardiasis,
hookworm.
Acute diarrhoea can be categorised into (a) osmotic; (b) secretory; (c) inflammatory and (d)
dysmotility.
Clinico-pathological features of index conditions / Able to provide advice to travellers about
prevention and management of diarrhoeal illness / Epidemiology of infective diseases in
UK/overseas / Prevention of traveller’s diarrhoea / Pharmacology of treatments for diarrhoeal
disease / Role of surgery in index conditions / Able to initiate appropriate drug therapy and
monitor its effectiveness…. To follow:
Infective diarrhoeas – incl Microbiology of infective diarrhoea
-
-
-
Infection of the gut – gastroenteritis
A virus is the common cause of infective diarrhoea in the UK. Various viruses are easily spread
from person-to-person by close contact, or when an infected person prepares food for others.
Infection with rotavirus is the most common cause of diarrhoea in children in the UK. Almost every
child in the UK has a rotavirus infection before they are five years old. Adenovirus is another
common cause.
Food poisoning causes some cases of diarrhoea. Food poisoning is usually caused by a bacterial
infection. Common examples are bacteria called Campylobacter, Salmonella and Escherichia coli.
Toxins (poisons) produced by bacteria can also cause food poisoning. Parasites can also be a cause
of food poisoning.
Water contaminated by bacteria or other germs is another common cause of infective diarrhoea,
particularly in countries with poor sanitation.
Symptoms of infective diarrhoea
Can range from a mild stomach upset for a day or two with slight diarrhoea, to severe watery
diarrhoea for several days or longer.
Blood or mucus can appear in the stools with some infections.
Crampy pains in the abdomen (tummy) are common. Pains may ease each time some
diarrhoea is passed.
Vomiting
High temperature (fever), aching limbs and headache may also develop.
Diarrhoea often lasts for 3-5 days, sometimes longer. It often continues for a few days after
any vomiting stops.
Slightly loose stools (loose faeces) may persist for a week or so further before a normal
pattern returns.
Causes
Parasites: Cryptosporidium parvum, Giardia lamblia, Entamoeba histolytica etc
Bacteria : Campylobacter, Clostridium dificile, Escherichia coli, Listeria monocytogenes,
salmonella enteritidis, Shigella
Viral : HIV, rotavirus, Hepatitis A and E
SHIGELLA
Source – contaminated foods
Diarrhoea (bloody)
Fever
Abdominal cramps
SHIGELLA = Gram –ve,
bacilli, aerobic, simple
growth requirements,
non-lactose fermenting,
oxidase -ve
ESCHERICHIA COLI
Source – raw meat and unpasteurised milk
E. COLI = Gram –ve,
bacilli, aerobic, simple
growth requirements,
lactose fermenting
Severe diarrhoea (bloody)
Abdominal cramps
Usually no fever
E. coli 0157:H7 = very serious, kills the elderly and the very young
! Can cause haemolytic uraemic syndrome: haemolytic anaemia, acute renal failure,
thrombocytopenia
Listeria
Source – unpasteurised milk, hot dogs, deli meats, raw meats
(poultry), raw vegetables
Diarrhoea
Fever and muscle ache
Nausea
Can cause headaches, confusion, fits
Can lead to listeria meningitis
LISTERIA= Gram +ve,
bacilli, aerobic
E.g. L. monocytogenes
SALMONELLA
Aetiology
Transmission
Salmonella typhi can cause typhoid fever (more severe)
Salmonella paratyphi (types A,B,C), can cause paratyphoid fever.
Symptoms /
signs
Salmonella can contaminate meat, poultry, eggs, milk and other dairy
Sometimes, other foods such as fruit and vegetables can become
contaminated via contact with manure / Shellfish may be contaminated if
in contact with infected sewage in the water.
Adequate cooking of meat and poultry usually kills salmonella bacteria.
Dogs, cats and rodents can sometimes become infected with salmonella
and tortoises and terrapins are also common salmonella carriers.
Diarrhoea +/- blood
Stomach cramps
Nausea and vomiting
Fever
Onset within 12-72 hours of eating the contaminated food / being in
contact with the infected animal or person = 'incubation period'
Symptoms are usually relatively mild and improve within 4-7 days
If severe, dehydration can occur
Typhoid fever
Symptoms
Malaise
High fever
Headache
CNS: coma, delirium, meningism
Pea soup diarrhoea (+/- constipation in 1st week)
Signs
High fever with bradycardia
Hepatosplenomegaly
Abdominal distension
Rose spots: pink blanching papules found on the trunk (40% of patients)
Tachypnoea (3rd week)
Parathyroid fever – is a similar illness to typhoid fever but symptoms are
generally milder.
Investigations
Often remains undiagnosed, if patients do not seek medical help.
Temperature, pulse, BP
Abdominal exam
Stool culture – diagnosis of salmonella
Bloods: LFTS ↑, WCC↓, anaemia
SALMONELLA = Gram –
Typhoid / paratyphoid fever
Blood culture (1st 10 days)
Bone marrow culture (idea)
Urine / stool culture
ve, bacilli, aerobic, simple
growth requirements,
non-lactose fermenting ,
oxidase –ve
Management
Most do not need specific treatment – see info on general tx for diarrhoea
Babies <6 months old - seek medical advice if they develop gastroenteritis.
An antibiotic (usually ciprofloxacin) is givien to:
- Children <6 months with salmonella
- Adults >50 years
- Malnourished or immunocompromised
- Patients with heart valve problems
- For thyphoid/parathyphoid fever
Loperamide for adults
Probiotics are not generally recommended
Prevention
Vaccine for:
Travellers o endemic areas (e.g. South Asia and Africa)
Laboratory workers at risk of contact with S. typhi
Prognosis
Parathyroid/Typhoid fever: Untreated 20% die, commonly in 2-4 weeks due
to: Toxaemia, Encephalopathy, GI perforation and haemorrhage,
Peritonitis, Toxic myocarditis
CLOSTRIDIUM DIFFICILE
Epidemiology /
incidence
Most cases occur in people who are in hospital (or care homes), or who
have recently been in hospital because:
a) bacteria and spores more likely to be found
b) people in hospital are more likely to have been given antibiotics.
1/5 people with diarrhoea post-antiobiotics have C. difficile
C. difficile infection is more common in older people. Over 8 in 10 cases
occur in people over the age of 65 because
a) older people are more commonly in hospital
b) older people more prone to this infection.
Risk factors include:
- Age
- Time spent in hospital
- Immunosuppression / comorbidities
- Takeing PPIs (proton pump inhibitors) e.g. omeprazole, lansoprazole
- Previous C. difficile infection (1 in 4-5 chance of re-infection)
C. difficile lives harmlessly in the gut of many (~3/100 adults, 7/10 babies)
C. difficile produces spores (like 'seeds') which are resistant to ↑ temps.
C. difficile bacteria make toxins that damage the colon.
Strain 027 produces more toxins than most other strains and is more likely
to cause severe illness.
Aetiology
Transmission
Spores are passed out with the faeces of those with C. difficile in their gut –
they can persist (on clothes, bedding, surfaces, etc) for several months/yrs
The spores can also be spread through the air
They may get on to food, and into the mouth and gut of some people.
Symptoms /
signs
Many cases are mild
Mild or moderate watery diarrhoea.
Crampy abdominal pains
Nausea
Fever
Symptoms may last from a few days to several weeks. In mild cases,
symptoms often clear away without any specific treatment.
Pseudomembranous colitis
This occurs in some cases and is more serious. Colitis = colon inflammation
Pseudomembranous = membrane-like patches on the inside lining of the
colon. This can cause:
Bloody diarrhoea
Abdominal pain
A distended colon and abdomen
Fever
In some cases it becomes severe and life-threatening ('fulminant colitis').
The colon may perforate causing serious infection +/- death.
Investigations
Management
Suspected in:
C. DIF = Gram
Anyone who develops diarrhoea who has had antibiotics
within the previous 2 months ..and/or…
+ve, bacilli,
When diarrhoea develops during (or within few weeks)
aerobic
of a hospital stay
Stool sample – confirms diagnosis by detecting the C. difficile toxin
Blood tests, an abdominal X-ray or a CT scan may be indicated if severe
Prevention - not prescribing unnecessary antiobiotics
No treatment for carriers
If mild symptoms: treat at home, If severe: admission
Note: remain off work / school until free from diarrhoea for 48 hrs.
Stop any antibiotics
Allows normal bacteria to thrive again
The ‘overgrowth’ of C. difficile should reduce
Start vancomycin / metronidazole
These antiobiotics kill C. difficile
Symptoms then improve in 2-3 days (in severe cases, may prevent
perforation)
Ensure plenty of fluids to avoid dehydration (see earlier notes)
Surgery in rare cases
In cases of fulminant colitis, especially if the colon perforates
Avoid anti-diarrhoeals e.g. loperamide – they may slow rate of clearance
Probiotics (‘good’ bacteria and yeasts) are not recommended
Prognosis
Most patients recover, some without treatment
Death and perforation of the colon can occur in fulminant colitis
CAMPLYLOBACTER
Epidemiology
The most common bacteria causing food poisoning in the UK.
More common in certain groups of people:
Children under the age of five and adults over the age of 60.
People who travel to developing countries where sanitation and food
hygiene may be less strict.
People working with farm animals.
People who work in the meat industry.
Transmission
Camplylobacter bacteria are commonly found in raw meat, esp poultry.
Adequate cooking of meat thoroughly kills salmonella bacteria.
Camplylobacter may also be found in unpasteurised milk or untreated
water (including ice cubes made from untreated water).
Occasionally mushrooms and shellfish can contain campylobacter
Pets (incl cats and dogs) and other animals can also pass on campylobacter
to you (without any symptoms themselves!)
Symptoms /
signs
Investigations
Management
Diarrhoea
Nausea +/- vomiting
Stomach cramps
Fever
Onset within 2-5 days of eating the food / being in contact with the
contaminated animal… but sometimes the incubation period can be as long
as 10 days
In most, symptoms are mild and improve within 2-3 days
About 9/10 recover in a week
If severe, dehydration can occur
Often remains unconfirmed, if patients do not seek
medical help.
Signs of dehydration
Temperature, pulse, BP
Abdominal exam
Stool sample – diagnosis of campylobacter
CAMPYLOBACTER =
Gram +ve, bacilli,
aerobic, fastidious
growth requirements
Most patients do not need specific treatment.
Occasionally, admission to hospital is needed if symptoms are severe, or if
complications develop. Antibiotics may then be given.
Ensure plenty of fluids to avoid dehydration (see oral rehydration therapy
notes for adults/children)
Babies under six months old are at increased risk of dehydration. You
should seek medical advice if they develop gastroenteritis.
Paracetamol / ibuprofen to ease a high temperature or abdominal pain
Loperamide for adults
Probiotics are not generally recommended
Anti-diarrhoeals not indicated for children <12
CHOLERA
Epidemiology
Endemic in portions of Asia, the Middle East, Africa, South and Central
America, and the Gulf Coast of the US – here incidence is highest in
children, and tends to decrease with age due to acquired immunity
In non-endemic areas: cholera prevalence is not age dependent - this
reflects that most of the population have no immunity
Aetiology
Cholera is caused by infection with the bacterium Vibrio cholera =
Over 100 serotypes of V. cholerae exist but only two cause disease: V.
cholerae 01 (two biotypes - classic and El Tor) and O139.
There are other types of species of V. cholerae which also cause
infection in humans including V. parahaemolyticus, V. mimicus, V.
damsela and V. hollisae and they also cause diarrhoea.
Transmission is usually from contaminated water and direct person-toperson transmission is rare.
It is not endemic to UK.
Most patients are free of V. cholerae within 2 wk after cessation of
diarrhea; chronic biliary tract carriers are rare.
Pathophysiology
Symptoms
Vibrio cholerae colonises the small intestine and produces a potent
endotoxin which binds the GMI-ganglioside receptor on cell membrane
The active subunits of the endotoxin enters the cell and activates the
adenyl cyclise – causing accumulation of cyclic AMP
This stimulates active secretion of ionic sodium, chloride, potassium
and HCO3 into the lumen, and with it water = diarrhoea
The incubation period is 6 to 72 hours.
1) Most people infected do not become ill although they may be excreting
the organism for 7 to 14 days.
2) A number of people develop diarrhoea that is undistinguishable from
other forms of gastroenteritis.
3) ~10% develop severe illness (3 stages)
Evacuation phase - abrupt onset of profuse, watery diarrhoea (rice
water stools - because mucus flecks may be seen floating in the watery
stools) +/- vomiting
Collapse phase - features of circulatory shock, and dehydration. Often
apathetic but not usually delirious. +/- severe muscle cramps +/- renal
failure. A child may present with convulsions due to hypoglycaemia.
Recovery phase - if the patient survives the collapse phase then there is
a gradual return to clinical and biochemical normality over 1-3 days
Signs
Circulatory collapse e.g. tachycardia, cold clammy skin, peripheral
cyanosis, hypotension.
Dehydration
Investigations
●
●
●
●
●
●
CHOLERA = Gram –ve,
Stool specimen to identify organism.
curved bacilli, aerobic,
U&E, as likely to be significantly dehydrated, and to
simple growth
monitor IV fluid replacement. Creatinine may rise if
requirements, nonkidneys fail with prolonged hypovolaemia (via renal
lactose fermenting,
tubular necrosis).
Severe metabolic acidosis with K+ depletion (but
oxidase +ve
normal serum Na+ concentration) occur.
FBC will show a high Hb with haemoconcentration.
WCC (raised, but will not aid diagnosis or management)
A good way of estimating net fluid loss or gain if changes are large is to
weigh the patient daily. 1 kg of weight represents 1 litre of fluid.
Treatment
► ! notifiable disease
► Resuscitation
Replacement of fluid lost.
To replace K+ losses, KCl can be added to the IV solution (esp
important for children)
Oral glucose-electrolyte solution is effective in replacing stool losses
► Antibiotics
However, if fluid loss is profuse, antibiotics may help.
Tetracycline, erythromycin, doxycycline, norfloxacin, ciprofloxacin and
furazolidone may be used - reduce the rate of stool output (minimises
fluid loss, stops excretion of vibrio)
► Feeding
Feeding during and after cholera is emphasised.
× Antidiarrhoeals and antisecretory drugs
Prevention
Avoid drinking untreated water or eating poorly cooked seafood in
endemic areas.
An oral cholera vaccine is now available in the UK - not required by
most but may be suitable for aid workers assisting in disaster relief or
refugee camps, and more adventurous backpackers who do not have
access to medical care.
Inflammatory bowel disease
Crohn’s
Ulcerative Colitis
Epidemiology
●
●
●
●
Peak onset: 20-40
Slight F>M
Slightly ↑ smokers than expected
Common in whites / jews
● Peak onset: 20-40
● Slight F>M
● Slightly ↓ smokers than
expected
● Common in whites / jews
Symptoms
Diarrhoea
Abdominal cramps (on eating)
Weight loss & Anorexia
Fever & malaise
Vomiting & nausea
Diarrhoea
Lower abdominal pain
Weight loss & Anorexia
PR bleeding +/- mucus
Urgency and tenesmus
May be: relapsing + remitting,
continuous, or single episode
Signs
Pyrexia
Abdominal tenderness
Perianal lesions
Anaemia
Mouth ulcers
Clubbing
Pyrexia, tachycardia, tender
distended abdo (severe)
Clubbing
Investigations
Bloods
● FBC, U+E, LFTs, CRP/ESR
● ANCA (Anti-Neutrophil Cytoplasmic Antibody): Raised in UC, not Crohn’s
● ESR and CRP: ↑ in active Crohn’s, ESR ↑ also in UC
PR / stool
● Rectal exam
● Stool sample- exclude infectious causes
Imaging
● Sigmoidoscopy and biopsy
● Capsule endoscopy for small bowel in Crohn’s
● Barium study- cobblestoning in Crohn’s
Pathology
Crohns
Anywhere mouth → anus
may also be inflammation in regional
lymph nodes.
UC
Large bowel only, spreads from
rectum proximally
Skip lesions
Continuous (from rectum)
Transmural / deep ulcers
Superficial / shallow ulcers
Non-caseating granulomas
Goblet cell mucus depletion, crypt
abscesses, haemorrhagic
+ adenocarcinoma risk
+++ adenocarcinoma risk
Management
Anti-diarrhoeals: Loperamide
Supplements: vitamin and nutrient
Anti-inflammatory: Prednisolone ,
Hydrocortisone if severe.
Immunosuppressive: Ciclosporin /
Azathioprine
For fistulae: Infliximab
Complications
Malabsorption
Small bowel syndrome
Fistulae
Obstruction ( by strictures)
Perforation +/- peritonitis
Haemorrhage
Anal fissures, fistulas and skin tags
(rarely) Systemic
amyloidosis
Acute - Prednisolone
Maintaining remission- 5Aminosaliculic acid
(Mesalazine)
Curative surgery:
pancolectomy, with ileoanal
anastomosis/ileostomy
Colon - haemorrhage, toxic
megacolon (>6cm),
adenocarcinma
Joints - ankylosing spondylitis,
arthritis
Eyes - iritis, uveitis, episcleritis
Skin – pigmentation, erythema
nodosum, pyoderma
gangrenosum
Liver - fatty change, chronic
pericholangitis, sclersosing
Cholangitis, cirrhosis, hepatitis
Systemic: anaemia, venous
thrombosis, electrolyte
disturbances
Extraintestinal: pyoderma gangrenosum, erythema nodosum, primary sclerosing cholangitis, fatty
liver/abscesses, iritis / episcleritis, arthiritis, spondylitis.
GI malignancy
Colorectal adenocarcinoma
Risk factors
× Age >50 years
× IBD (UC > Chron’s disease)
× Hereditary non-polyposis colorectal
cancer (can do prophylactic
colectomies)
× Familial adenomatous polyposis
Symptoms
PR Bleeding / mucus
Altered bowel habit
Tenesmus
Fatigue / weight loss / pallor
(systemic/anaemia)
IF bowel obstruction: pain, bloating,
vomiting
Jaundice (if liver mets)
×
×
×
×
×
×
×
PMH/FH: colorectal or breast cancer
Alcohol abuse
Smoking
Low-fibre diet?
↑ animal fat/red meat diet?
Pre-menopause M > F
After menopause F > M
Signs
Rectal or abdominal mass
Weight loss
Anaemia
Hepatomegaly (if liver mets)
Cancers arising in the caecum and right colon are often asymptomatic and present as irondeficiency anaemia
Left – sided colonic cancers typically present with looser and more frequent stools +/- abdominal
pain
Rectal and sigmoid cancers commonly bleed, causing blood in stools, mixed in, as well as tenesmus
and ↓ stool diameter
Investigations
● Colonoscopy = gold standard. Allows imaging of whole colon and biopsy. Can’t do it in
clinic.
● Sigmoidoscopy = accurate for rectal / sigmoid tumours. Only images the last 1/3 of
colon. Can be done in clinic. Detects smaller adenomatous polyps than barium enema
● Double contrast barium enema = can visualise colonic tumours
● Endo anal US / pelvic MRI = staging rectal cancers
● CT / PET = assessment of metastases
● FBC – microcytic anaemia
● Faecal occult blood = screening for ages 60-69
● CEA (carcino-embryonic antigen) – may be used to monitor effectiveness of treatment
● If polyposis in family, refer for DNA testing once a patient is >15 years
DUKES
A
STAGING
5 year prognosis
B
C
D
Intramucosal
Invaded bowel
wall
Transmural +
lymph nodes
Distant
metastases
95%
75%
30%
<5%
Treatment
● Stenting – can give significant palliation, or be used pre-surgery to allow elective
resection
● Radiotherapy
● Chemotherapy
· Fluorouracil +/- agents such as folinic acid, lavamisole, is used in Dukes stage C
· Newer agents include: irinotecan, oxaliplatin
● Surgery
Tumour location
Surgical procedure
Caecal, ascending or proximal transverse
colon tumours
Right hemicolectomy
Tumours in the distal transverse or
descending colon
Left hemicolectomy
Sigmoid colon tumours
Sigmoid colectomy
Low sigmoid or high rectal tumours
Anterior resection – anastomosis / colostomy
Low rectal tumours (<8cm from anal canal)
Abdomino-perineal (A-P resection) – permenant
colostomy and removal of rectum and anus
Patients with single-lobe hapatic
metastases and no extrahepatic spread
May be suitable for curatice surgery with liver
reserction
Cause /
epidemiology
×
×
×
×
GASTRIC CANCER
Strong link with Helicobacter pylori and gastritis
Smoking ↑s risk
Pernicious anaemia has a small ↑ in risk
Veg + fruits, ↓ salt – protect from gastric cancer
× Peaks 50-70 years
× M>F
Symptoms
Epigastric pain – relieved by food and antacids (indistinguishable from
peptic ulcer)
Dyspepsia
o > 1 month
o Aged 55 and over
Vomiting (severe if ca is at pylorus)
Weight loss
Dysphagia (if ca invades fundus)
Anaemia (gross haematemesis is rare)
Signs
Tender epigastric mass (50%)
Weight loss
Hepatomegaly, jaundice, ascites (mets)
Troisier’s sign = Enlarged left supraclavicular node (Virchow’s node)
Gastric cancer is the cancer most commonly associated with
dermatomyositis and achanthosis nigricans
Investigations
● FBC, LFTs
● Gastroscopy + ulcer edge biopsies
● Staging CT
Management
Surgical
· Endoscopic mucosal resection (early)
· Partial or total gastrectomy
Chemotherapy
Palliative for obstruction/ pain/ haemorrhage
Malabsorption syndromes
Defective intraluminal digestion
Pancreatic insufficiency
– pancreatitis
– cystic fibrosis
defective bile secretion (lack of fat solubilisation)
– biliary obstruction
– ileal resection – decreased bile salt uptake
bacterial overgrowth
Insufficient absorptive area
– Coeliac’s disease (gluten sensitive enteropathy)
– Chron’s
– extensive surface parasitisation
– small intestinal resection or bypass (procedure for morbid obesity / Crohn’s disease /
infarcted small bowel)
Lack of digestive enzymes
disaccharidase deficiency (lactose intolerance)
bacterial overgrowth
– brush border damage
Defective epithelial transport
abetalipoproteinaemia
primary bile acid malabsorption
– mutations in bile acid transporter protein
Lymphatic obstruction
lymphoma
tuberculosis
Vitamin E deficiency
low birth weight
haemolytic anaemia of mother
Vitamin D deficiency
Osteomalacia / rickets
Vitamin K deficiency
Haemorrhage
Vitamin A Deficiency
Eye changes begin with night blindness. If it is not treated, it leads to complete blindness.
Drying of the white portion of the eye.
Increased rate of infections especially of the respiratory system.
Anaemia
General body weakness. The person complains of tiredness and breathlessness.
Loss of appetite.
Paleness of tongue, white portion of eye (conjunctival pallor) and nail beds.
Feeling of being pricked with pins and needles on the fingers and toes.
Brittle and spoon shaped nails (koilonychia)
The capacity of a person to work decreases considerably.
Iodine Deficiency
Iodine is an important component of thyroxine. Iodine deficiency is most commonly seen as
goitre in adults and cretinism in young children.
In adults
Goitre.
Weight gain
The person feels tired and is unable to work properly.
Dry skin
Constipation
In young children
Growth retardation
Mental retardation
Speech and hearing defects
Disorders of nerves and muscles causing inability to control movements of limbs.
CARBOHYDRATE INTOLERANCE
Is the inability to digest certain carbohydrates due to a lack of one+ intestinal enzymes.
Symptoms include diarrhea, abdominal distention, and flatulence.
● Diagnosis is clinical and by an H2 breath test.
Treatment is removal of the causative disaccharide from the diet.
GLUTEN MALABSORPTION = COELIAC DISEASE
Pathophysiology
Coeliac disease is a state of heightened immunological response to
ingested gluten in genetically susceptible people.
Aetiology
achlorhydria:
Symptoms
Can be diagnosed in any age, presents in children and adults
May be asymptomatic
Chronic or intermittent diarrhoea
Failure to thrive in children
Sudden or unexpected weight loss
Persistent or unexplained GI symptoms e.g.
- nausea and vomiting
- Recurrent or abdominal pain
- Cramping
- Abdominal distension
Prolonged fatigue
Unexplained faints
Unexplained anaemia
Investigations
May be asymptomatic, therefore, serological testing should also be
offered in children and adults with first degree relatives with:
× Coeliac’s disease
× Autoimmune thyroid disease
× Dermatitis hepetiformis
× Irritable bowel syndrome
× Type 1 diabetes
Or other conditions: http://www.nice.org.uk/nicemedia/pdf/CG86FullGuideline.pdf
1)
2)
3)
4)
IgA tissue transglutaminase (tTGA)
If unequivocal: IgA endomysial antibodies(EMA) testing
If either above are –ve: IgA deficiency testing
If IgA deficient: IgG tTGA or EMA
● If any of the results are positive, refer for biopsy to exclude or confirm
Coeliac disease:
Marsh classification
Marsh stage 0: normal mucosa
Marsh stage 1: increased number of intra-epithelial lymphocytes
Marsh stage 2: proliferation of the crypts of Lieberkuhn
Marsh stage 3: partial or complete villous atrophy
Marsh stage 4: hypoplasia of the small bowel architecture
Treatment
Only current treatment is a life-long gluten free diet
Dietician input is generally requested
LACTOSE INTOLERANCE
Lactose intolerance is a result of lactase deficiency and is a form of carbohydrate
malabsorption.
Lactose is hydrolyzed by lactase in the intestinal mucosa. Lactase is one of many betagalactosidases seen in the small bowel and is most active in the jejunum. The byproducts of lactose hydrolysis are the monosaccharides:
1) glucose
2) galactose
When lactase is absent or deficient, hydrolysis of the sugar lactose is incomplete because it is osmotically active, the undigested sugar will pull fluid into the intestine.
Hydrogen and lactic acid, in addition to other organic acids, are produced when colonic
bacteria act on the undigested sugar
The combined osmotic effect of the undigested sugar and organic acids results in the
passage of acidic diarrheal stools. These stools can produce significant skin irritation and
breakdown
Infants with lactose intolerance may also present with abdominal distension and
vomiting
In its most severe forms lactose intolerance can lead to dehydration, electrolyte
abnormalities, and failure to thrive.
Lactase deficiency has been described as primary, secondary, or congenital
a) congenital lactase deficiency
A rare hereditary disorder in which lactase activity is absent
b) primary lactase deficiency
The normal gradual reduction in lactase production seen as an individual matures
from infancy into adulthood and is expressed variably across populations
c) secondary lactase deficiency
Lactase deficiency may also be a secondary occurrence because of gastroenteritis,
bowel surgery, cystic fibrosis, or immune disorders. (or transiently in infants
exposed to phototherapy and antibiotic therapy)
Blind loop syndrome
Pathophysiology
In blind loop syndrome a portion of the small intestine becomes
bypassed and thus cut off from the normal flow of food.
The digestion of food becomes slow or stops leading to the growth of
bacteria and malabsorption
A total aerobic plus anaerobic count of more than 100,000 is
diagnostic of bacterial overgrowth.
Aetiology
Radiation enteritis
duodeno-jejunal diverticulae
surgery e.g. Polya gastrectomy,
Billroth's operation II, Roux-enY procedure, gastric bypass for
obesity2
secondary to obstruction:
o Crohn's disease
o tumour
o radiation stricture
o pseudo-obstruction
fistulae:
o especially small bowel to
colon fistulae
hypogammaglobulinaemia
Symptoms
Loss of appetite and early satiety
Dyspepsia
Diarrhoea and steatorrhoea
Bloating, flatulence
Weight loss
Nausea
Signs
Cachexia
abdominal distension
evidence of vitamin and mineral deficiencies
Investigations
●
Bloods may reveal:
Macrocytic anaemia (due to vitamin B12 deficiency)
Hypocalcaemia
Iron deficiency
Raised INR (due to vitamin K deficiency)
Abdominal imaging including:
o Abdominal X-ray
o Abdominal CT scan
o Barium studies (may reveal diverticulae or strictures)
o
o
o
o
●
tropical sprue
systemic sclerosis /
scleroderma
autonomic neuropathy:
o diabetes mellitus
achlorhydria:
o vagotomy
o drugs
o autoimmune
o old age
●
●
●
Treatment
Hydrogen breath test to detect bacterial overgrowth
Specialised investigations looking at small intestine function:
o D-xylose breath test
o Faecal fat test
o Bile acid breath test
Small intestine aspirate with fluid culture - invasive and difficult
► Broad spectrum antibiotics - E. coli is the most common organism and
is sensitive to ampicillin, or tetracyclines (e.g. oxytetracycline)
► Nutritional supplements:
Vitamin B12 injections.
Oral iron supplements.
Oral calcium and vitamin D supplements; other vitamin
supplements.
Medium chain triglycerides (are more readily digested)
► Surgical correction of the affected small bowel segment
Motility disorders
Reduced contact time/surface area: Rapid intestinal transit and diminished surface area impair
fluid absorption and cause diarrhoea.
×
Small-bowel or large-bowel resection or bypass
×
Gastric resection
×
Inflammatory bowel disease
×
Microscopic colitis (collagenous or lymphocytic colitis)
×
Coeliac disease
× Stimulation of intestinal smooth muscle by drugs (eg, Mg-containing antacids, laxatives,
cholinesterase inhibitors, SSRIs) or humoral agents (eg, prostaglandins, serotonin) also can
speed transit.
Factitious diarrahoea
PAtiet acts as if he or she has an illness by deliberately producing, feigning, or exaggerating
symptoms. (aka Münchausen syndrome)
The primary aim is to obtain sympathy, nurturance, and attention accompanying the sick role.
This is in contrast to malingering, in which the patient wishes to obtain external gains such as
disability payments or to avoid an unpleasant situation, such as military duty
Epidemiological methods for investigating food poisoning outbreak
Food poisoning is one of a number of notifiable diseases. Doctors in Wales and England have a
statutory duty to notify a 'Proper Officer' of the Local Authority of suspected cases of food
poisoning based on clinical symptoms – under the Public Health (Control of Disease) Act 1984
These data are compiled into a weekly Statutory Notifications of Infectious Diseases (NOIDs)
report by the Health Protection Agency (HPA) Centre for Infections in Colindale, North London.
Laboratory testing of specimens submitted by patients may undergo laboratory testing to
establish the organism responsible for illness
Aware of disease notification requirements in relation to diarrhoeal diseases
NOTIFIABLE DISEASES RELATED TO DIARRHOEA
Food poisoning
Cholera
Haemolytic uraemic
Enteric fever (typhoid or
syndrome (HUS)
paratyphoid fever)
Infectious bloody
diarrhoea
Who to contact:
Notify a 'proper officer' of the Local Authority of suspected cases of certain infectious
diseases"; usually the consultant in communicable disease control (CCDC).
The GP should fill out a notification certificate immediately on diagnosis without waiting for
laboratory confirmation - and ensure it gets to the officer within 3 days (phone if urgent).
Books of certificates are available, and there is also a template notification document on
the Health Protection Agency website (Centre for Infections).
Include the following information:
Patient's name, date of birth, sex, and home address with postcode.
Patient's NHS number.
Ethnicity (used to monitor health equalities).
Occupation, and/or place of work or educational establishment if relevant.
Current residence (if it is not the home address).
Contact telephone number.
Contact details of a parent (for children).
The disease or infection, or nature of poisoning/contamination being reported.
Date of onset of symptoms and date of diagnosis.
Any relevant overseas travel history.
If in hospital, also:
o Hospital address.
o Day admitted.
o Whether the disease was contracted in hospital.