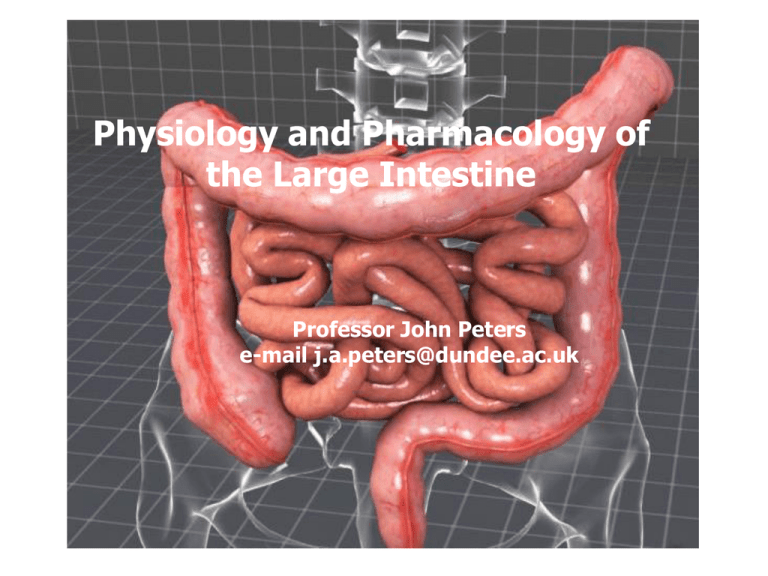
Physiology and Pharmacology of
the Large Intestine
Professor John Peters
e-mail j.a.peters@dundee.ac.uk
Learning Objectives
After this lecture, students should be able to:
Describe the structure and function of the large intestine and the
patterns of motility that it exhibits
Provide an account of the defaecation reflex
Outline the causes of constipation and its treatment by purgatives
Describe water balance within the G.I. Tract
Understand the principles of oral rehydration therapy and the role of
SGLT1 in this process
Outline the causes of diarrhoea and its treatment by antimotility
agents
The Large Intestine - General
Approximately 1.5 m long, 6 cm diameter
Comprises
• Colon
o Ascending
o Transverse
o Descending
o Sigmoid
• Caecum
• Appendix
• Rectum
Normally receives approximately 500 ml of chyme (indigestible
residues, unabsorbed biliary components, unabsorbed fluid) per day –
entry permitted by the gastroilial reflex
Is primarily involved in:
• Absorption of fluids and electrolytes (Na+, Cl-)
• Secretion of electrolytes (K+ and HCO3-) and mucus
• Formation, storage and periodic elimination of faeces
Patterns of Motility in the Large Intestine (1)
Haustration
Peristaltic propulsive movements
Mass movement
Defaecation
Haustration - haustra are saccules caused by contraction of the circular
muscle – similar to segmentation in function, but much lower frequency
Peristaltic propulsive movement – occur in both the aboral and oral
directions. Oral movements occur principally in the ascending and
transverse colon – contributes to long transit time (16 – 48 hours)
Mass movement – simultaneous contraction of large sections (about 20
cm) of the circular muscle of the ascending and transverse colon - drives
faeces into distal regions
•
•
Occurs about one to three times daily
Typically triggered by a meal (often breakfast) via the gastrocolic
response involving
o gastrin
o extrinsic nerve plexuses
Patterns of Motility in the Large Intestine (2)
Defaecation
Pelvic nerve
Activation of afferents to
spinal cord
Activation of
parasympathetic
efferents
Mass movement rectum fills with faecal
matter
Activation of rectal
stretch receptors
Activation of afferents to
brain (urge to defaecate)
Contraction of smooth
muscle of colon and
rectum – internal anal
sphincter relaxes
Relaxation of skeletal
muscle of external anal
sphincter
Defaecation assisted by abdomenal
contraction and expiration against
closed glottis
Pudendal nerve
Altered firing in efferents
to spinal cord
Contraction of skeletal
muscle of external anal
sphincter
Defaecation delayed – rectal wall
gradually relaxes
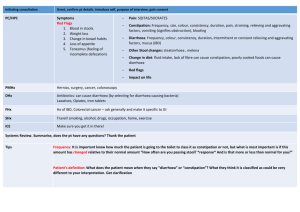
CONSTIPATION and PURGATIVES
Numerous causes of constipation: e.g. improper diet, drugs, metabolic
disorders
Constipation is the presence of hard dried faeces within the colon
Pugatives:
increase peristalsis and/or soften faeces causing, or assisting,
evacuation
are resorted to far too readily in some societies by
individuals obsessed by ‘regularity’
can be abused in eating disorders and may
also disguise underlying disease
Medically sound uses of laxatives include:
• when ‘straining’ is potentially damaging to health (e.g. patients with
angina), or when defaecation is painful (e.g. haemorrhoids) predisposing
to constipation
• to clear the bowel before surgery or endoscopy
• to treat drug-induced constipation, or constipation in bedridden, or
elderly patients
PURGATIVES AND THEIR MECHANISM(S) OF ACTION
Bulk laxatives
(e.g. methylcellulose -orally)
Stimulant purgatives
(e.g. bisacodyl – oral or
suppository)
Retain H2O
volume
Retain H2O
volume
Osmotic laxatives
(e.g. magnesium sulphate / hydroxide – orally
sodium citrate – rectally)
Stimulate peristalis;
cause H2O and
electrolyte secretion
Faecal
softening
Faecal softners
(e.g. docusate sodium – orally)
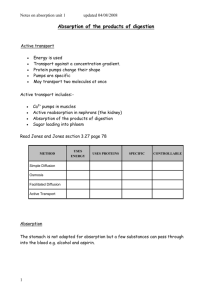
Absorption of Water in the GI Tract
Absorption of water is a passive process
driven by the transport of solutes
(particularly Na+) from the lumen of the
intestines to the bloodstream
Water ingested and secreted is normally
in balance with water absorbed
Typical values are:
9.3 litre entering tract per day
8.3 litre absorbed by small intestine
1 litre enters large intestine of which
90% is absorbed
Thus faeces normally contain 100 ml
water along with 50 ml cellulose,
bilirubin and bacteria
Diarrhoea is defined as loss of fluid
and solutes from the GI tract in
excess of 500 ml per day
CAUSES OF DIARRHOEA (1)
Diarrhoea can have numerous causes:
infectious agents – viruses, bacteria (e.g. traveller’s diarrhoea)
chronic disease
toxins
drugs
psychological factors
Diarrhoea
may involve the small, or large, intestine
can result in dehydration, metabolic acidosis (HCO3- loss) and
hypokalaemia (K+ loss)
may be fatal if severe (e.g. cholera)
Treatment of severe acute diarrhoea can include:
maintenance of fluid and electrolyte balance (first priority)
use of anti-infective agents (if appropriate)
use of non-antimicrobial antidiarrhoeal agents (symptomatic)
CAUSES OF DIARRHOEA (2)
•
•
•
Impaired absorption of NaCl
Congenital defects
Inflammation
Infection (e.g. enterotoxins from
some strains of E.coli and
campylobacter sp.)
• Excess bile acid in colon
Non-absorbable, or poorly
absorbable, solutes in
intestinal lumen
• Lactase deficiency
Hypermotility
Excessive secretion
• Cholera provides a classic (and
extreme) example
•
•
•
•
•
•
cholera toxin enters enterocyte
enzymatically inhibits GTPase activity of
the Gs subunit
increased activity of adenylate cyclase
increased concentration of cAMP
cAMP stimulates CFTR
hypersecretion of Cl-, with Na+ and water
following
Na+/K+ ATPase
Na+/K+/2Clco-tranporter
Chloride channel
(CFTR)
Rehydration Therapy Exploits SGLT1
1. 2 Na+ bind
2. Affinity for glucose increases,
glucose binds
3. Na+ and glucose translocate from
extracellular to intracellular
4. 2 Na+ dissociate, affinity for
glucose falls
5. Glucose dissociates
6. Cycle is repeated
Oral rehydration salts contain (for example)
• Glucose 20 g
• Sodium chloride 3.5 g
• Sodium bicarbonate 2.5 g
• Potassium chloride 1.5 g
Dissolved in a volume of 1 L drinking water
Absorption of Na+ and glucose by
SGLT1 cause accompanying
absorption of H20
ANTIMOTILITY AGENTS USED IN TREATMENT OF
DIARRHOEA
Many morphine-like (or opiate) drugs have anti-diarrhoeal activity
The actions of opiates on the alimentary tract include:
• inhibition of enteric neurones (hyperpolarization via activation
of -opioid receptors)
• decreased peristalis, increased segmentation (i.e. constipating)
• increased fluid absorption
• constriction of pyloric, ileocolic and anal sphincters
The major opiates used in diarrhoea are:
• codeine
• diphenoxylate - low CNS penetration, low solubility in water
(abuse potential)
• loperamide – low CNS penetration, low solubility in water,
undergoes enterohepatic recycling